Abstract
Purpose: We investigated the nature of services providing community-based stroke rehabilitation across the UK, and goal setting practice used within them, to inform evaluation of a goal setting and action planning (G-AP) framework. Methods: We designed, piloted and electronically distributed a survey to health professionals working in community-based stroke rehabilitation settings across the UK. We optimised recruitment using a multi-faceted strategy. Results: Responses were analysed from 437 services. Services size, composition and input was highly variable; however, most were multi-disciplinary (82%; n = 335/407) and provided input to a mixed diagnostic group of patients (71%; n = 312/437). Ninety one percent of services (n = 358/395) reported setting goals with “all” or “most” stroke survivors. Seventeen percent (n = 65/380) reported that no methods were used to guide goal setting practice; 47% (n = 148/315) reported use of informal methods only. Goal setting practice varied, e.g. 98% of services (n = 362/369) reported routinely asking patients about goal priorities; 39% (n = 141/360) reported routinely providing patients with a copy of their goals. Conclusions: Goal setting is embedded within community-based stroke rehabilitation; however, practice varies and is potentially sub-optimal. Further evaluation of the G-AP framework is warranted to inform optimal practice. Evaluation design will take account of the diverse service models that exist.
Community-based stroke rehabilitation services across the UK are diverse and tend to see a mixed diagnostic group of patients.
Goal setting is implemented routinely within community-based stroke rehabilitation services; however, practice is variable and potentially sub-optimal.
Further evaluation of the G-AP framework is warranted to assess its effectiveness in practice.
Implications for Rehabilitation
Background
Goal setting is considered “best practice” in stroke rehabilitation [Citation1–3]; however, to date, no randomised controlled trials have been completed to demonstrate that goal setting makes a unique contribution to stroke survivors’ rehabilitation outcomes [Citation4]. This is not surprising as goal setting studies typically have weak methodological designs with poorly defined interventions that have little or no theoretical underpinning [Citation4–6]. In addition, the interaction between goal setting interventions and the context in which they are delivered is rarely considered; this is an important oversight if we are to understand how to optimise the implementation and adoption of goal setting interventions in practice [Citation7,Citation8]. The difficulties of designing a controlled trial of goal setting that is both methodologically sound and sufficiently powered to demonstrate an effect that have been documented [Citation9].
Addressing this evidence-practice gap has been the impetus behind our programme of research to develop and evaluate a goal setting and action planning (G-AP) practice framework. The G-AP framework guides health professionals through an optimal goal setting process with stroke survivors living in the community. It is evidence and theory based [Citation10] and has four key stages: (i) goal negotiation and setting; (ii) planning and measuring confidence; (iii) action; and (iv) appraisal, feedback and decision making [Citation11,Citation12]. G-AP shows promise as an acceptable and feasible framework for use in community-based stroke rehabilitation [Citation12]. The next stage is to evaluate the effectiveness of G-AP when compared to “usual” goal setting practice.
In line with the Medical Research Council guidelines for the development and evaluation of complex interventions [Citation13], we sought to understand both the context of services that could deliver G-AP and what “usual” goal setting practice looks like in these settings. This is important for two reasons. First, the interplay between an intervention and the context in which it is delivered influences how the intervention is implemented and whether it is successful or not [Citation14]. Pre-emptive consideration of this interplay highlights potential challenges that can be addressed during intervention development and evaluation [Citation7]. For example, development and evaluation of an oral health care intervention in stroke care settings was informed by a survey which found that use of oral health care protocols was sporadic, staff training in oral health care limited and equipment (such as tooth brushes) often not available [Citation15]. These findings confirmed the need for development and evaluation of an oral health care intervention. A training component and access to oral health care equipment was included within the intervention and a staff oral health care knowledge questionnaire added to the outcome measures used in its evaluation [Citation16]. Second, understanding “usual” goal setting practice (and variability in practice) allows investigation of the critical differences between G-AP and “usual” goal setting practice, what difference G-AP is likely to make over and above usual practice and how “usual” practice can be built on, or re-shaped, to put G-AP in place.
Enderby and Wade [Citation17] investigated community rehabilitation services in the UK. They reported “huge variation” between services in terms of their service model, management arrangements, composition, goals and life span of the service. Holliday et al. [Citation18] investigated goal setting methods used in community and in-patient rehabilitation settings in the UK. They reported that goal setting was used routinely in practice with a problem-orientated approach to goal setting most commonly reported. The majority of services elicited some degree of patient participation in the process. Whist informative, these surveys were relatively small (98 service responses in the former; 202 responses in the latter); are not current and did not focus on the details of goal setting practice in community-based stroke rehabilitation services. In short, we did not have the information required to inform further G-AP evaluation. To address this knowledge gap, we conducted a UK wide survey of goal setting practice in community-based stroke rehabilitation settings. The survey aimed to investigate:
The structure and nature of services providing community-based stroke rehabilitation across the UK.
What goal setting practice is in these settings, including reasons for non-use.
Methods
Study design
A bespoke electronic survey questionnaire was designed using Survey Monkey® to capture the required information at a national level (a copy of the survey is available on request from the first author). Development of the survey was informed by previous literature in this field [Citation11,Citation17–19]. The questionnaire covered five main topic areas: (i) the service profile (e.g. type, size, patient demographics, rehabilitation input provided), (ii) structures in place to support goal setting practice (e.g. goal setting meetings, documentation and methods used to guide practice), (iii) activities that comprised goal setting practice (which included goal setting activities included in the G-AP framework), (iv) priority given to goal setting, patient/carer involvement and inclusion of people with communication/cognitive difficulties and (v) reasons for non-use of goal setting (if applicable). The survey was subject to a piloting phase over a four-month period with health professionals (n = 12) working in community rehabilitation settings and academics (n = 10) with expertise in survey methods. Each expert was asked to review the electronic survey (including the study information sheet) and comment on the overall style and appeal of the survey, the relevance and clarity of each question, ease of navigation and time taken to complete. Feedback was provided to LS who iteratively revised the survey through three cycles of expert review and feedback.
Service inclusion/exclusion criteria
All services providing community-based rehabilitation to stroke survivors (either exclusively or with other diagnostic groups) living in the community were eligible to participate in the survey. In-patient services were excluded as were community-based services that did not provide services to stroke survivors.
Service recruitment strategy
As there is no centrally held list of community rehabilitation services in the UK, a three-pronged strategy was used to optimise team recruitment. Firstly, services across the UK were identified through various rehabilitation networks (such as The Community Therapists Network) and Allied Health Professions’ special interest groups (such as the College of Occupational Therapists specialist section for neurological practice). This approach was an extension of that used in previous surveys of this nature [Citation17,Citation18]. Secondly, rehabilitation coordinators and/or allied health professional leads in all 14 Scottish health boards were e-mailed and asked to provide a contact name and e-mail address for each community rehabilitation service manager or service lead in their area. Finally, a request to participate in the survey was included in presentations given by LS at two national UK conferences. A study information sheet and link to the electronic survey was e-mailed to each identified contact.
Survey respondents were asked to complete the on-line survey on behalf of their service. Due to the multi-faceted recruitment strategy, we anticipated that more than one health professional from an individual service could be invited to participate in the study. To identify multiple responses from the same service, respondents were asked (but not required) to state the name of their service and the town or city it was located in.
Ethics and research and development approvals
National Health Service research ethics committee approval was not required as the survey was to be completed by staff recruited on the basis of their professional role. Ethical approval was provided by The School of Nursing, Midwifery and Health Research Ethics Committee at the University of Stirling. Research and development approval was provided by individual health boards or trusts within Scotland, Wales and Northern Ireland but was not required for English sites.
Data collection and analysis
The survey was electronically distributed in June 2012 and data collected over a four-week period. Two reminders were e-mailed within the response period. Following data collection, data were downloaded from Survey Monkey® in an Excel format then imported into the Statistical Package for the Social Sciences (SPSS Version 19.0, IBM Corp, Armonk NY). Data were analysed using descriptive statistics. Responses to open-ended questions were categorised, counted and ranked.
Results
Response rate
A total of 573 health professionals responded to the survey. Forty-one responses were removed as they represented in-patient services. The remaining 532 responses were examined to identify multiple responses from the same service. Three hundred and eighty-two single service responses were identified and 150 multiple responses from 55 services. We aggregated data (using the mode response from each question) from multiple responses to create a single service response. Data were treated as missing in questions where no mode response was available (i.e. equal number of respondents from the same service gave a different response to a given question). Following this process, 437 individual service responses were identified and included in the analysis. Of these, 359 (82%) were complete and 78 (18%) incomplete. Sixty-four percent (n = 279) of services represented in the survey were from England; 27% (n = 118) from Scotland; 7% (n = 31) from Wales and 2% (n = 9) from Northern Ireland. Due to the multi-faceted, overlapping nature of the search strategy used to identify services, it is impossible to estimate recruitment rates; however, this is an excellent number of responses when compared to previous surveys of a similar nature [Citation17,Citation18].
Structure and nature of services providing community-based stroke rehabilitation across the UK
The characteristics of community-based stroke rehabilitation services are presented in . Most services reported that they were Early Supported Discharge Teams, Community Rehabilitation Teams or a combination of the two. Some health professionals (such as those who worked in specialist services or in remote areas) reported they created “bespoke” services with other health professionals on the basis of individual patient need. Services were highly variable in terms of their size, composition and the input they provide. The majority were multidisciplinary and included physiotherapists, occupational therapists and rehabilitation assistants. Typically, patients were seen their own home. The majority of services reported that input was provided for 5 to 12 weeks and for between two and five sessions a week. Most services saw a mixed diagnostic group of patients, both below and above 65 years of age.
Table 1. Characteristics of services providing community-based stroke rehabilitation.
Reported goal setting practice and reasons for non-use
Ninety-one percent (n = 358/395) of services reported that goal setting was used with all or most stroke patients; a further 8% (n = 33/395) reported that goal setting was used with some patients. Four services (1%) reported they did not use goal setting with any stroke patients. Reasons reported for non-use were: goal setting is not a valued activity within the service (Community Rehabilitation Team, Scotland); patients not able to participate in the goal-setting process (Bespoke team, Scotland; Bespoke Team, England); goal setting is too time consuming, not possible due to short duration of team input, team members lack confidence in their goal-setting skills and have not received adequate goal-setting training (Community Health and Social Care team, Northern Ireland).
Structures in place to support goal-setting practice
Goal setting method(s) used: Seventeen percent of services (n = 65/380) reported that no methods were used to guide goal-setting practice. The remaining 83% (n = 315/380) of services reported use of one or more formal and/or informal methods to guide practice ().
Table 2. Methods used to guide goal-setting practice.
Informal methods included the service using its own method or individual health professionals within the service using their own method. The most common formal methods reported by services were Goal Attainment Scaling and the Canadian Occupational Performance Measure. Other reported formal methods used by services included use of Specific Measurable Achievable Relevant Timed (SMART) goals (3%; n = 11/380), the East Kent Outcome System (2%; n = 8/380), the G-AP framework (2%; n = 6/380) and Malcomess Care Aims (1%; n = 5/380).
Data were aggregated within services into either: (i) formal methods only (Goal Attainment Scaling and/or Canadian Occupational Performance Measure and/or or other formal method); (ii) informal methods only (health professional or service used own method and/or other informal method) or a (iii) combination of informal and formal methods. Forty-seven percent (n = 148/315) of services reported use of informal methods only, 31% (n = 98/315) reported use of formal methods only and 22% (n = 69/315) a combination of formal and informal methods.
Goal setting meetings, documentation and training: Sixty percent (n = 230/382) of services reported they met to discuss patients’ goals once a week or more and 29% (n = 111/382) less than once a week; 11% (n = 41/382) reported that they never met to discuss patients’ goals. The majority of services (83%; n = 305/367) reported that they routinely documented goal setting activities; only one service reported never documenting goal setting activities. Fifty percent (n = 195/388) of services reported that most or some of their team members had participated in goal setting training; 32% (n = 122/388) reported that no team members had participated in training and 18% (n = 71/388) did not know.
Priority levels for goal setting and patient/carer involvement in the process
Respondents were asked to rate their service’s priority levels in relation to setting rehabilitation goals and involving patients (including those with cognitive or communication difficulties) and carers in the process. The vast majority reported that setting goals and involving patients (with or without cognitive/communication difficulties) was a high priority (). Involving carers was rated as a high priority for fewer services. The vast majority of services reported they set goals with the patient in one or more of the following ways: team set goals with the patient (n = 107/366; 29%); individual team members set goals with the patient (n = 254/366; 69%) or one team member set goals with the patient on behalf of the team (n = 57/366; 16%). Only 6% (n = 23/366) of services reported that they set goals as a team without the patient present.
Table 3. Reported service priority levels.
Reported use of goal setting activities
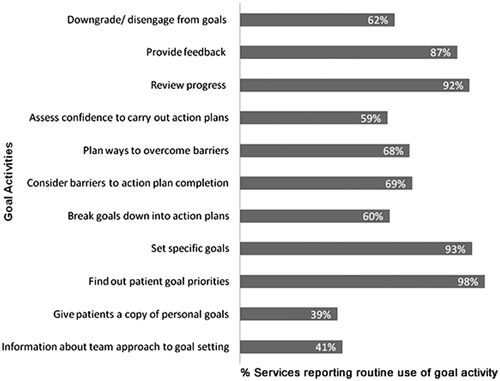
Reports of goal setting activities used within services indicated that some goal-related activities were implemented more routinely than others (: Reported use of goal setting activities). Over 90% of respondents reported that their team routinely: found out about patients’ goal priorities (n = 362/369); set specific goals to direct rehabilitation input (n = 343/370); reviewed goal progress (n = 342/371) and (to a slightly lesser extent) provided feedback to patients about their goal progress (n = 319/368).
Goal activities that appear to be less well established in practice with 59 to 70% of respondents reporting their routine use were: breaking down goals in action plans (or short term targets) (n = 216/359); assessing confidence to complete action plans (n = 212/360); identifying barriers that might hinder action plan completion (n = 250/361); planning ways to overcome barriers (n = 245/360) and downgrading or disengaging from goals if no progress is being made (n = 222/359).
The goal-related activities reported to be least well established in practice, with less than 40% of respondents reporting their routine use were: giving patients information about the team’s approach to goal setting (n = 147/359) and giving patients a copy of their personal goals (n = 141/360).
Discussion
This study investigated the nature of services providing community-based stroke rehabilitation across the UK and goal-setting practice used within them (including reasons for non-use) to inform evaluation of the G-AP framework. These aims were met through this survey which had excellent coverage and response at a national level. Our findings are discussed under the headings of service contexts and reported goal-setting practice. The implications for G-AP evaluation are highlighted.
Service contexts
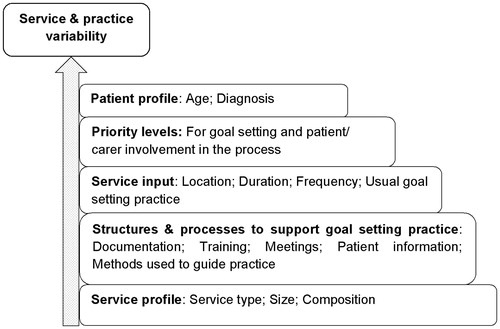
The survey responses show that, whilst commonalities exist in community-based stroke rehabilitation across the UK, individual services are complex and can differ in terms of their profile, the duration and intensity of input they provide and the structures and processes in place to support goal setting practice ().
Variability in community rehabilitation services have been noted in previous studies [Citation17,Citation20,Citation21]. We report two novel findings. First, whilst there is consensus that specialist stroke services are the optimal approach for hospital-based acute stroke care [Citation22], services providing community-based stroke rehabilitation tend not to be stroke specific. Most services see a mixed diagnostic group of patients, including stroke survivors. Second, Early Supported Discharge teams, Reablement teams and Intermediate Care teams have emerged as new models of service delivery in the UK. This may be in response to the evidence base indicating the benefits of early supported discharge with a selected group of stroke survivors [Citation23] and the UK policy initiatives to support people at home rather than in hospital [Citation24,Citation25]. The dynamic and changing nature of community rehabilitation contexts is likely to continue. For example, current policy initiatives in the UK are focusing on the integration of health and social care [Citation26,Citation27] which will influence how, where and by whom community rehabilitation is delivered to stroke survivors in the future.
Reported goal-setting practice
The vast majority of respondents reported that their service used goal setting with all or most stroke survivors; that goal setting was a high priority, that goal-related activities were routinely documented and that goal review meetings took place on a weekly basis. This reported commitment to goal setting in practice is encouraging and in keeping with the recommended use of goal setting across stroke clinical guidelines in the UK [Citation2,Citation3,Citation28]. However, our findings highlight important issues relating to the quality and delivery of goal setting in practice.
Patient involvement
The majority of services reported that they set goals with patients and that involving patients in the process (including those with communication and/or cognitive deficits) was a high priority. In contrast to this, and reflecting the findings of a previous survey [Citation18], most services reported they did not routinely provide patients with information about the team approach to goal setting or give patients a copy of their personal goals. Two recent systematic reviews have shown that patients want to be involved in the goal-setting process, but are often unclear about their role in the process and feel that they have no control over the goals [Citation4,Citation6]. Patients may be more likely to participate in the goal-setting process if they are clear about what the process is (or even that it exists) and how they can contribute to it. Whilst some stroke survivors will have agreed their goals and remember what they are over the course of their rehabilitation, others (such as those with cognitive or communication difficulties) may not. An accessible copy of rehabilitation goals may promote a sense of ownership and control over personal goals for these patient groups.
Variable and potentially sub-optimal practice
Service responses suggest that there is a high level of variability in the methods used to guide goal-setting practice. Some services do not use any methods to guide goal-setting practice, others use their own methods. Formal methods (either used exclusively or in combination with the services’ own methods) are evident in practice, the most common being Goal Attainment Scaling [Citation29] and the Canadian Occupational Performance Measure [Citation30]. The goal related activities that comprise “usual” goal setting practice also varies. The most common reported goal-related activities are congruent with some of those included in the G-AP framework: identifying patient priorities; setting specific rehabilitation goals, reviewing progress and providing feedback. Activities included within the G-AP framework that are less evident in practice are: - breaking down goals into action plans (or steps); identifying barriers to action plan completion; planning ways to overcome anticipated barriers; assessing confidence to complete plans and downgrading or disengaging from unattainable goals.
This noted variability in goal setting methods and practice suggests that a comprehensive, systematic approach to practice may be lacking. Use of Goal Attainment Scaling and the Canadian Occupational Performance Measure may address this issue to some extent. Both methods are clearly described and (in different ways) offer a standard approach to identifying patient-centred goals and measuring goal-related progress. However, they do not guide health professionals through all stages of the goal-setting process [Citation31]. The G-AP framework includes, (i) a patient-centred planning stage (which details goal-related activities that will optimise patients’ behaviour as they pursue their personal goals) and (ii) an appraisal, feedback and decision-making stage (which informs practice following goal-related successes, setbacks and failures) [Citation10–12]. These activities are not explicitly stated in other approaches to goal-setting practice. These findings support our view that whilst G-AP and “usual” practice will (to differing degrees) share commonalities, there are critical differences. These differences have the potential to improve patient outcomes by optimising goal attainment and/or facilitating goal adjustments or disengagement if progress is not being made [Citation12,Citation32,Citation33].
Implications G-AP evaluation
There is a strong theoretical rationale and developing evidence base that suggests use of the G-AP framework could enhance goal-setting practice and optimise patients’ goal-related outcomes [Citation10–12]. The findings of this survey will be used to decide the best way to approach the next stage of its evaluation. Evaluation of complex interventions is challenging and requires careful consideration of a range of study designs [Citation13]. To minimise the risk of bias, use of a randomised-controlled trial should always be considered when assessing effectiveness of an intervention [Citation13]. Patient-level randomisation is unlikely to be feasible for G-AP evaluation due to the risk of contamination between the intervention and control group. A cluster randomised control trial design reduces this risk, but may require large (and potentially impractical) number of services to create comparable clusters with enough statistical power to detect an effect [Citation34]. A stepped wedge design may be a better solution. Although large number of sites may still be required, their entry into the trial can be staggered which may help with logistical issues, e.g. completing G-AP training in individual services prior to implementation. Additionally, service variability issues may be more effectively managed as each service would act as its own control. Use of this design is becoming more evident in the evaluation of a range health care interventions [Citation35] including goal setting [Citation36]. Alternatively, other non-randomised designs may be preferable. Realist evaluation [Citation37] seeks to determine what works, for whom, under what circumstances. As such, the interplay between intervention and the context in which it is delivered is integral to the evaluation. These, and other, study designs will be fully considered in our next phase of work.
A further consideration is whether G-AP should be evaluated in stroke-specific services, as was our initial intention, or if services that see mixed diagnostic group of patients should be included. On the basis of our results, restricting G-AP to stroke-specific services will significantly limit the number of services in which it can be implemented and evaluated. Including services that see a mixed diagnostic group of patients will increase services available for recruitment and optimise the external validity of the findings. However, this may necessitate further development work to inform optimum implementation of G-AP with other patient groups.
Limitations of this study
Our recruitment strategy maximised reach to health professionals working across the UK in community-based stroke settings. In some cases, however, this resulted in more than one member of the same service responding to the survey. We developed an explicit decision-making framework to identify duplicate service responses (based on team name and location data if available or team location and patient age, diagnosis, usual place of input and core professional groups represented in service data). Whilst we may have missed some duplicate service responses or included service responses as duplicates that were not, we believe our decision-making framework minimised this to a level that did not pose a risk to integrity of our results.
We asked respondents to complete the survey on behalf of their service. Our rationale for this was that goal-setting practice in community-based stroke rehabilitation is a team endeavour organised around patients’ personal goals. However, our findings contradict this assumption. Often, goal-setting practice appears to operate at the level of the individual health professional rather than the team. Consequently, responding on behalf of their team may have been problematic for some respondents. Whilst we acknowledge this as a limitation, we were pleased with the high number of completed responses – this suggests that the survey was acceptable to respondents and they felt they could make a meaningful response on behalf of their service.
Finally, the results of this survey are based on health professional reports rather than on observed practice. Other studies have demonstrated that health professional reports of clinical practice can be unreliable and may reflect what “should” happen rather than what does happen [Citation38]. The results of this survey should be viewed from this perspective.
Conclusions
This is the largest survey to date of goal-setting practice in services delivering community-based stroke rehabilitation in the UK. The results underline the clinical importance of goal setting with stroke survivors in the community and the complexity of the community rehabilitation services in which it is delivered. Goal-setting practice is highly variable and potentially sub-optimal. A suitably designed evaluation of the G-AP framework is warranted to develop the evidence base to optimise goal-setting practice and patient outcomes in these settings.
Acknowledgements
We would like to thank all respondents from community rehabilitation services across the UK who kindly completed this survey.
Declaration of interest
The authors report no declarations of interest. This research was funded by the Chief Scientists Office grant number DTF/11/02.
References
- Scottish Intercollegiate Guidelines Network (SIGN). Management of patients with stroke or TIA: assessment, investigation, immediate management and secondary prevention. A national clinical guideline. Edinburgh: SIGN; 2008
- Intercollegiate Stroke Working Party. National clinical guidelines for stroke – 4th edition. London: Royal College of Physicians; 2012
- Scottish Intercollegiate Guidelines Network (SIGN). Management of patients with stroke: rehabilitation, prevention and management of complications, and discharge planning. A national clinical guideline. Edinburgh: SIGN; 2010
- Sugavanam T, Mead G, Donaghy M, van Wijke F. The effects and experiences of goal setting – a systematic review. Disabil Rehabil 2013;35:177–90
- Levack WM, Taylor K, Siegert RJ, et al. Is goal planning in rehabilitation effective? A systematic review. Clin Rehabil 2006;20:739–55
- Rosewilliam S, Roskell C, Pandyan A. A systematic review and synthesis of the quantitative and qualitative evidence behind patient-centred goal setting in stroke rehabilitation. Clin Rehabil 2011;25:501–14
- Wells M, Williams B, Treweek S, et al. Intervention description is not enough: evidence from an in-depth multiple case study on the untold role and impact of context in randomised controlled trials of seven complex interventions. Trials 2012;13:95
- Tomoaia-Cotisel A, Scammon DL, Waitzman NJ, et al. Context matters: The experience of 14 research teams in systematically reporting contextual factors important for practice change. Ann Family Med 2013;11:S115–23
- Taylor WJ, Brown M, William L, et al. A pilot cluster randomized controlled trial of structured goal-setting following stroke. Clin Rehabil 2012;26:327–38
- Scobbie L, Dixon D, Wyke S. Identifying and applying psychological theory to setting and achieving rehabilitation goals. Clin Rehabil 2009;23:321–33
- Scobbie L, Dixon D, Wyke S. Goal-setting and action planning in the rehabilitation setting: development of theoretically informed practice framework. Clin Rehabil 2011;25:468–82
- Scobbie L, McLean D, Dixon D, et al. Implementing a framework for goal setting in community based stroke rehabilitation: a process evaluation. BMC Health Services Res 2013;13:190
- Craig P, Dieppe P, MacIntyre S, et al. Medical Research Council. Developing and evaluating complex interventions: new guidance. Available from: http://www.mrc.ac.uk/documents/pdf/complex-interventions-guidance/ [last accessed 8 Aug 2014]
- Hoddinott P, Britten J, Pill R. Why do interventions work in some places and not others: a breastfeeding support group trial. Soc Sci Med 2010;70:769–78
- Talbot A, Brady M, Furlanetto DL, et al. Oral care and stroke units. Gerodontology 2005;22:77–83
- Brady MC, Stott DJ, Norrie J, et al. Developing and evaluating the implementation of a complex intervention: using mixed methods to inform the design of a randomised controlled trial of an oral healthcare intervention after stroke. Trials 2011;12:168
- Enderby P, Wade DT. Community rehabilitation in the United Kingdom. Clin Rehabil 2001;15:577–81
- Holliday RC, Antoun M, Playford ED. A survey of goal-setting methods used in rehabilitation. Neurorehabil Neural Repair 2005;19:227–31
- Playford ED, Siegert R, Levack W, Freeman J. Areas of consensus and controversy about goal setting in rehabilitation: a conference report. Clin Rehabil 2009;23:334–44
- McMillan TM, Ledder H. A survey of services provided by community neurorehabilitation teams in south east England. Clin Rehabil 2001;15:582–8
- Geddes J, Chamberlain MA. Stroke community rehabilitation: a classification of four different types of service. Int J Ther Rehabil 2003;10:299–304
- Stroke Unit Trialists' Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database of Systematic Reviews 2007. Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD000197.pub2/pdf [last accessed 8 Aug 2014]
- Fearon P, Langhorne P, Early Supported discharge trialists. Services for reducing duration of hospital care for acute stroke patients. Cochrane Database of Systematic Reviews 2012, Issue 9. Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD000443.pub3/pdf [last accessed 8 Aug 2014]
- Francis J, Fisher M, Rutter D. Reablement: a cost effective route to better outcomes. London: Social Care Institute for Excellence; 2011. Available from: http://www.scie.org.uk/publications/briefings/briefing36/index.asp [last accessed 8 Aug 2014]
- Maximising Recovery, Promoting Independence: the Intermediate Care Framework for Scotland. The Scottish Government. Edinburgh; 2012. Available from: http://www.scotland.gov.uk/Resource/0038/00386925.pdf [last accessed 29 April 2014]
- Integration of Health and Social Care. The Scottish Government, Edinburgh. Available from: http://www.scotland.gov.uk/Topics/Health/Policy/Adult-Health-SocialCare-Integration [last accessed 29 April 2014]
- Integrated Care: Our Shared Commitment. Department of Health; 2013. Available from: https://www.gov.uk/government/publications/integrated-care [last accessed 23 May 2014]
- National Institute for Health and Care Excellence (NICE). Stroke rehabilitation: long term rehabilitation after stroke. National Institute for Health and Care Excellence; 2013. Available from: http://www.nice.org.uk/Guidance/CG162 [last accessed 29 April 2014]
- Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil 2009;23:362–70 [published erratum appears in Clin Rehabil 2010;24:191]
- Carswell A, McColl MA, Baptiste S, et al. The Canadian occupational performance measure: a research and clinical literature review. Can J Occup Ther 2004;71:210–22
- Stevens A, Beurskens A, Köke A, van der Weijden T. The use of patient-specific measurement instruments in the process of goal-setting: a systematic review of available instruments and their feasibility. Clin Rehabil 2013;27:1005–19
- Dunne E, Wrosch C, Miller GE. Goal disengagement, functional disability, and depressive symptoms in old age. Health Psychol 2011;30:763–70
- Coffey L, Gallagher P, Desmond D, Ryall N. Goal pursuit, goal adjustment, and affective well-being following lower limb amputation. Brit J Health Psychol 2014;19:409–24
- Sanson-Fisher RW, Bonevski B, Green LW, D’Este C. Limitations of the randomized controlled trial in evaluating population-based health interventions. Am J Prev Med 2007;33:155–61
- Brown CA, Lilford RJ. The stepped wedge design – a systematic review. BMC Med Res Methodol 2006;6:54
- Kjeken I, Berdal G, Bo I, et al. Evaluation of a structured goal planning and tailored follow-up programme in rehabilitation for patients with rheumatic diseases: protocol for a pragmatic, stepped-wedge cluster randomized trial. BMC Musculoskel Disorders 2014;15:153
- Pawson R, Tilly N. Realist evaluation. London: Sage Publications Ltd; 1997
- Middleton S. Keeping it simple: the power of three clinical protocols. J Clin Nurs 2012;21:3195–7
- Reablement: the added value of Occupational Therapists. London: College of Occupational Therapists; 2010. Available from: www.cot.co.uk/sites/default/files/position_statements/public/positionstatement-reablement.pdf [last accessed 13 Aug 2014]
- National Service Framework for older people. London: Department of Health; 2001. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/198033/National_Service_Framework_for_Older_People.pdf [last accessed 13 Aug 2014]