Abstract
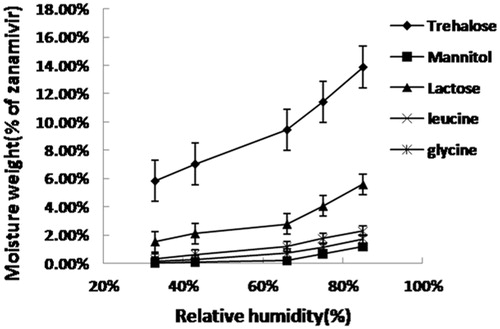
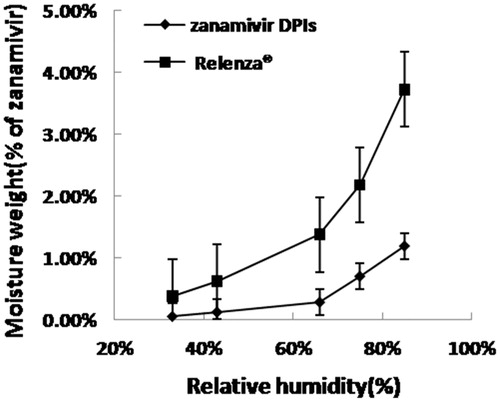
This work describes a new dry powder for inhalation containing zanamivir, which is less hygroscopic than Relenza®. The powders were prepared via a spray-drying technique using mannitol as the carrier. A 53 central composite design was used to optimize the formulations. The final optimized powders, characterized with an angle of repose 37.48°, an aerodynamic diameter of 2.346 μm and in vitro deposition of 58.54%, were obtained by using the predicted variable values. Relenza® absorbed a significant amount of water at 66%, 75% and 85% relative humidity (RH; weight changes of approximately 1.38%, 2.18% and 3.72%, respectively). In contrast, the weight change for the zanamivir dry powder inhalation (DPI) was negligible when the RH was increased to 66%. The in vivo potential for the optimized powders was studied further in rats via the endotracheal administration of an 8.4 mg/kg dose. The bioavailability was 116% relative to Relenza®. Fluorescence imaging monitored the zanamivir dry powder inhalers in rats. The results indicated that the zanamivir DPIs were effectively delivered to the lung. These results indicate that the spray-dried zanamivir DPIs were promising for pulmonary delivery.
Introduction
Zanamivir is a new anti-flu drug produced by Glaxo Wellcome. It is a potent and highly selective inhibitor of influenza A and B virus neuraminidase (Cox et al., Citation2001). When directly administered to the human respiratory tract, zanamivir has exhibited potent anti-viral effects. Relenza® (zanamivir for inhalation) consists of four regularly spaced double-foil blisters each containing a powder mixture with 5 mg of zanamivir and 20 mg of lactose. Although the dry powder (Relenza®) exhibited good aerosolization properties, it has drawbacks linked to lactose and air-jet milling (Yang et al., Citation2014). Therefore, developing a new inhalable zanamivir formulation could overcome these drawbacks.
Currently, nearly all dry powder inhalation (DPI) products (Relenza®, Seretide®, Spiriva®, Symbicort®, Beclophar® and Flixotide®) on the market rely on lactose as the carrier material. The advantages of lactose are its well-investigated toxicity, broad availability and relatively low price. In addition, lactose crystals have smooth surfaces, regular shapes and good flowability (Steckel & Bolzen, Citation2004). However, using lactose has certain disadvantages such as its hygroscopicity. Hygroscopicity increases powder agglomeration via interparticle capillary forces, which reduces the dry powder dispersibility. Relenza® is best stored below 30 °C, which may limit its use in some tropical and subtropical areas. In addition, increasing the humidity progressively modifies the surface adhesion forces between zanamivir and lactose, and diffusion on the lactose surface at high relative humidities (RHs; above 32%) may form grains in the new phase, which can affect the drug delivery (Bevard et al., Citation2002). Moreover, lactose cannot be used for drug delivery to diabetic and intolerant patients due to clinical considerations. Therefore, finding alternative excipients with similar beneficial properties but decreased hygroscopicity is reasonable to expand the storage conditions to a wider range of areas and people.
Air-jet milling is a commonly used method for preparing inhalable powders. However, micronization using air-jet milling is extremely inefficient (Donovan et al., Citation2011). The micronization process forms small, irregularly shaped, flat particles and extensive flat surfaces yield large contact areas that increase particle adhesion. In this study, we used spray drying to form micron-sized particles. Spray-drying was developed as an alternative to micronization in the early 1990s. Spray drying, a single-step process with great control over the particle characteristics (Stahl et al., Citation2002; Asada et al., Citation2004; Chan et al., Citation2004; Cook et al., Citation2005), was used for powder preparations. Compared to milling, spray-drying produces more particles with lower contact areas and smaller, more homogeneous particle-size distributions that increase the respirable fraction relative to mechanically micronized drugs (Steckel & Brandes, Citation2004).
This study focused on selecting suitable excipients to overcome the drawbacks of Relenza®. Then, the subsequent optimizations were aiming to obtain the best formulation, named as zanamivir DPI, which followed with evaluations and characterizations. Powders were first prepared via spray drying using excipients such as lactose and mannitol that are approved by the Food and Drug Administration for inhalation and used in drug formulations for DPI insulin delivery (Exubera®, Pfizer), materials such as trehalose that seems suitable for DPI (Bosquillon et al., Citation2001; Cline & Dalby, Citation2002; Ogain et al., Citation2011), and amino acids such as leucine and glycine that may improve the powder dispersibility and hydrophobicity. Second, we optimized the formulations of the selected excipients via the response surface methodology using a 53 central composite design. In addition to the physicochemical characteristics, the in vitro powder deposition was also investigated. An analytical method based on liquid chromatography–mass spectrometry (LC–MS/MS) was developed to simultaneously determine zanamivir in the in vivo samples. Finally, fluorescence imaging was used to visualize and evaluate the pulmonary delivery of the powder in rats.
Materials and methods
Materials
Zanamivir (purity: 99.11%) and zanamivir A (used as internal standard, Hubei Haoxin Pharmaceutical Company, Ezhou, China), mannitol (Tianjin Bodi Chemical Reagent Company, Tianjin, China), trehalose (Hayashibara Co., Ltd., Okayama, Japan), lactose (Beijing Fengli Jingqiu Commerce and Trade Co., Ltd., Beijing, China), glycine (Shanghai Bo’ao Biological Technology Co., Ltd., Shanghai, China) and leucine (Shanghai Kangda Amino acids Factory, Shanghai, China) were obtained from the indicated suppliers. Poloxamer 188 (Lutroly F68) was purchased from BASF (Shanghai, China). Cy7 (Cy7 acid, mono-NHS ester, Beijing Fanbo Biochemicals Co., Ltd., Beijing, China) was used as an imaging agent for the dry powder delivery to the lungs. All other materials or solvents were of analytical or chromatographic grade and were used as obtained.
Preparation of zanamivir powders for inhalation
The quantity of zanamivir and excipients shown in were weighed and added to the volume of distilled water required obtaining identical concentrations before stirring continuously until a clear solution formed. The filtrates obtained after passing through a 0.45-μm water membrane filter were used as the liquid samples. The prepared formulations were spray-dried using an SD-06AG spray dryer (Lab-Plant, North Yorkshire, UK) under the following conditions: inlet temperature, 150°°C; atomization pressure, 140 kPa; feed rate, 1.67 ml/min; aspirator setting, 30 m3/h. The resultant dry powders were collected in bottles and saved in a vacuum dryer.
Table 1. Formulation of zanamivir dry powder with different excipients.
Experimental design
A 53 factorial design was used to determine the formulations. This study involved 20 experiments conducted as a single block. Three variables were considered: mannitol (X1), leucine (X2) and F68 (X3). All formulations were prepared from solutions with the same zanamivir content (20%) and total material concentration following the same procedure and spray-drying conditions. The responses considered were the response angle (Y1), geometric standard diameter (GSD, Y2), fine particle fraction (FPF, Y3) and mass media aerodynamic diameter (MMAD, Y4) of the dry powder. Data modeling and statistical analyses were performed using the Design Expert, 8.0.6 (Stat-Ease Inc., Minneapolis, MN).
Statistical data analysis and optimization model validation
Central composite design (CCD) was used to optimize the effective factors and effectively described the process responses. Fitting a multiple linear regression model to a 53 factorial design yields a predictor equation that incorporates interactive and polynomial terms to evaluate the responses. The polynomial equation was as follows:
(1)
This model aims to evaluate the effect of the linear, xi; quadratic, and the interactive, xixj, independent variable terms had on the dependent variable. Y was the measured response associated with each factor combination; b0 is an intercept representing the arithmetic average for all quantitative outcomes of the nine runs; bi (b1, b2, b3, b12, b23, b13, b11, b22 and b33) are regression coefficients computed from the observed experimental Y values. The five levels for each variable were −1.68, −1, 0, +1, +1.68 and lists the actual values corresponding to each variable. x1, x2 and x3 are the coded independent variable levels. The main effects (x1, x2 and x3) are the average result after changing one factor at a time. The interaction terms show the response when two factors were changed simultaneously. The optimum dependent variables were calculated for the desired response using a numerical optimization tool via the desirability approach.
Table 2. Variables in the central composite experimental design.
HPLC analysis of zanamivir
The zanamivir concentration was determined using a high performance liquid chromatography (HPLC 1200, Agilent Technologies, Santna Clara, CA) with a Luna SCX HPLC column (250 mm × 4.6 mm, 5 μm, Phenomenex, Torrance, CA) operating at room temperature. The mobile phase was an acetonitrile–0.02 mol/l acetate (60:40 v/v) buffer containing 0.2% acetic acid (pH 3.7) with a 1 mL/min flow rate, and the detection was performed at 233 nm. The calibration curve for each formulation was generated via a linear regression over the range from 0.05 to 0.90 mg/mL for five concentrations. The regression coefficient (r2) values were greater than 0.999 for all formulations, which indicates satisfactory linearity.
Spray-dried powder characterization
Moisture absorption
Weighed samples spread uniformly in open Petri dishes were placed in a climatic cabinet (CLMACELL 222t, MMM Medcenter Einrichtungen GmbH, Planegg, Germany) with varying RHs(between 33% and 85%) for 24 h at 30 °C before removing and weighing again. The moisture absorption profile was expressed as the percent increase in weight at different RHs.
Powder flowability
The repose angle for the spray-dried powders with various formulations was measured using a Powder Flow Tester (Copley Scientific, Nottingham, UK).
Particle size analysis
The geometric particle size distribution for spray-dried powders with various formulations was determined using a light-scattering particle size analyzer (LS800, OMC Corp., Zhuhai, China). The samples were suspended in methyl tert-butyl ether (MTBE) and dichloromethane solutions (MTBE–dichloromethane = 3:1).
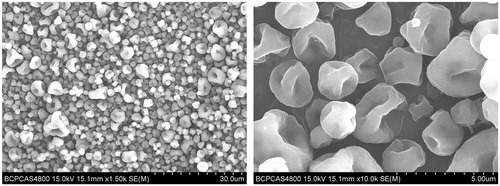
Particle morphologies
The zanamivir DPI was observed and photographed via scanning election microscopy (S-4800, Hitachi, Tokyo, Japan) after coating a powder sample on an aluminum stub with palladium–gold.
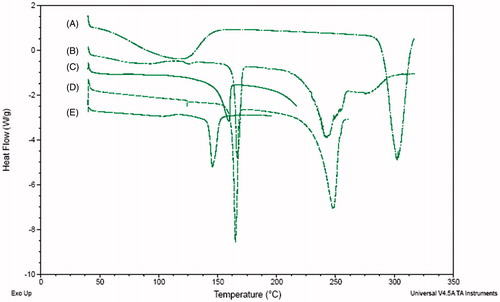
Differential scanning calorimetry
The thermal properties of the zanamivir DPI and Relenza® were analyzed using a differential scanning calorimeter (DSC TA Q500 Q2000, TA Instruments-Waters LLC, New Castle, DE). The powder samples were crimp-sealed in DSC sample pans with pinhole lids and exposed to a 5 °C/min temperature ramp between 30 and 350 °C.
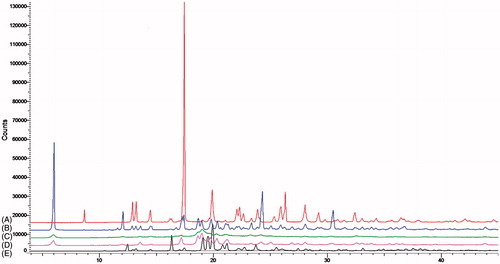
X-ray powder diffraction
The crystal structures for the zanamivir DPI and Relenza® were characterized via X-ray powder diffraction (XRPD; Bruker, D8 Advance, Karlsruhe, Germany). The settings were a 5–45° 2θ range, 0.04° 2θ step size, 1 s step time and 25°°C temperature.
Moisture content
The water content for the spray-dried powders was analytically quantified using a KF coulometric titrator (Metrohm 870 KF Titrino plus, Herisau, Switzerland). The reaction cell was filled with Hydranal-Composite 5K. Approximately 50 mg of a powder sample was weighed and injected into anhydrous methanol. The sample solution was then reacted with the KF reagent. The dry powder moisture was then calculated. All experiments were performed in triplicate (n = 3).
In vitro powder deposition
The in vitro dispersions for spray-dried powders with various formulations were investigated using a Next Generation Impactor (NGI) (Copley Scientific, Nottingham, UK) with a flow rate of 60 l /min and actuated in 4-s intervals. Before using, the impaction cups for each of the seven stages were coated with Silicone Release Spray (Dow Corning Corporation, Midland, MI) and allowed to dry. The surface coating prevented any particle to “bounce” between stages. Size 3 gelatin capsules filled with 25 mg of the powders were placed into a Turbospin (AstraZeneca, London, UK) dry powder inhaler. Ten capsules were discharged into the NGI. After running, the inhaler, adaptor mouthpiece, throat and NGI stages were washed with a suitable volume of the mobile phase, which was assayed for the solute concentration via HPLC as described above.
The FPF (ratio of drug below 5 μm) and MMAD (diameter at 50% of the cumulative undersize weight) data were calculated using Copley Inhaler Testing Data Analysis Software (Copley Scientific, Nottingham, UK).
In vivo studies
Pulmonary pharmacokinetics
All animal experiments were approved and performed in accordance with the guidelines of the Institutional Animal Care and Use of Beijing Pharmaceutical University. Twelve male Wister rats weighing between 200 ± 20 g were divided into two groups with six in the control and the others in the experimental group. Before the endotracheal administration of testing drugs, all of the rats were anesthetized with a 1% sodium pentobarbital solution (40 mg/kg body weight) by intraperitoneal injection. The control and experimental groups were administered Relenza® and zanamivir DPI, respectively, via an endotracheal administration. Aerosol particles generated from the DP-4 powder insufflators (Penn-Century Inc., Philadelphia, PA) (Duret et al., Citation2012). The endotracheal administration used a dry powder insufflator model adapted for rat endotracheal powder insufflations. A precisely weighed quantity (8.4 mg/kg body weight) of the dry powder was introduced to the DP-4 sample chamber. The delivery tube was introduced to the rat trachea just before the carina (the first trachea bifurcation) as described by Bivas-Benita et al. (Citation2005). The dry powder insufflation involved connecting the DP-4 to a 5-ml air syringe with a plunger from a 2-ml air syringe. After this administration, orbital venous blood was collected in heparinized tubes at different times (5 min, 15 min, 30 min, 1 h, 2 h, 4 h, 6 h and 8 h). The total blood was centrifuged at 3000 rpm for 8 min. Plasma was collected and stored at −70 °C until analysis.
Chromatographic quantification methods
A HPLC method was used for the separation as described in the HPLC analysis of zanamivir section. The mass spectrometer source (Agilent 6410 Triple Quad LC/MS, USA) was operated in the positive ion mode. The scanner used the multiple reaction monitoring mode. The detection ions were 276.2 → 216.2 (zanamivir) and 325.2 → 109.1 (zanamivir A). All plasma samples (50 μl) were extracted via protein precipitation by adding MeOH to 50 μl (46 g/l) zanamivir A and vortexing for 3 min. Then, samples were centrifuged at 3000 rpm for 15 min before injecting 10 μl of the supernatant into the LC–MS/MS system.
Pharmacokinetic and statistical analysis
The zanamivir serums were presented as the mean ± standard deviation (n = 6) for each time point. The two data were compared by using the Kruskal–Wallis tests. Then, the results were processed the Dunn’s post hoc analysis with WinNonlin software (WinNonlin, Mountain View, CA) for the 0.05 significance. The zanamivir pharmacokinetic profile was characterized using the maximum concentration (Cmax), time to Cmax (Tmax), elimination rate constant (Kel), half-life (T1/2) and area under the curve (AUC0–8h) between 0 and 8 h. The Cmax and Tmax were determined from the raw data; the elimination rate constant (Kel) was obtained from the in concentration–time profiles; T1/2 was 0.693/Kel; AUC0–8h was calculated via the trapezoidal calculation method.
In vivo fluorescence detection
The dry powder formulation containing the Cy7 fluorophore and the zanamivir DPI as a negative control were endotracheally administered as described in the pulmonary pharmacokinetics to rats section. The rats were measured at different time intervals (0.25, 0.5, 1, 1.5, 2 h). Subsequently, tissues (heart, lung, liver and kidney) were dissected, washed with normal saline, made free from adhering tissues. The fluorescence for rats and tissues was detected using an in vivo imaging system (IVIS Lumina, Caliper, Newton MA).
Results and discussion
Zanamivir dry powder preparation
Five zanamivir dry powders with different excipients were prepared via the spray-drying method and the corresponding moisture absorptions for 33%, 43%, 66%, 75% and 85% RH are presented in . Moisture increases powder agglomeration via inter-particulate capillary forces, which reduces the dry powder dispersibility. In these formulations, the mannitol and leucine carriers can effectively reduce the moisture absorption. Mannitol exhibited good anti-hygroscopic properties for zanamivir dry inhalation powders because powders with mannitol are less sensitive to moisture at high RHs. Amino acids can enhance the aerosol behavior for spray-dried powders by reducing moisture sorption and surface tension (Batycky et al., Citation2004; Seville et al., Citation2007; Lechuga-Ballesteros et al., Citation2008). Amino acids may improve the powder dispersibility. Powders containing leucine exhibited lower moisture absorption than those containing glycine. Moreover, leucine exhibited the strongest effect due to its surfactant-like properties (Gliniski et al., Citation2000; Seville et al., Citation2007). Leucine, a dispersion enhancing excipient, was incorporated into the formulations to promote particle deaggregation (Raula et al., Citation2008, Citation2010). Thus, mannitol and leucine were selected to optimize the formulation. In addition to mannitol and leucine, poloxamer 188 (F68) was used to control the micronized particle surface properties and prevent their agglomeration and becoming highly charged.
Formulation optimization
The optimization study was conducted by response surface methodology. The outcomes are presented in with an overview of the experimental designs and corresponding responses. The generated responses from the experimental design were fit to polynomial models, and an analysis of variance (ANOVA) test was applied to these polynomial models to estimate their significance. The results of this analysis indicated that Y1, Y2, Y3 and Y4 best fit a first-order, two-factor interaction and quadratic model. The ANOVA performed to estimate the significance of the model and term is shown in . Items with a p value above 0.05 were ignored because only smaller p values indicated that the corresponding coefficient was significant, and the model was development further using significant items (Khodadoust & Hadjmohammadi, Citation2011). The following models were established from the CCD runs:
(2)
(3)
(4)
(5)
Table 3. Observed responses for the central composite rotatable design.
Table 4. Summary of results of ANOVA for measured responses.
The polynomial equations contained coefficient for the intercept, first-order main effect, interaction terms and higher order effects. The results for the factor effects and associated response p values for Y1, Y2, Y3 and Y4 are presented in . The sign and magnitude of the main effect indicated the relative influence for each response factor. Furthermore, a positive sign signified a synergistic effect, whereas a negative sign indicated an antagonistic effect.
portrays the 3-D response surface plot generated via the response surface methodology. The third factor was held at level zero for all pictures except . In this figure, the first factor was held at level zero. This figure depicts the response surface plot for X2 and X3 on the angle of repose, which was linear. The powder angle of repose (θ) is an important parameter that determines the flow. The factor for X2 had higher “F” values than X3 (), which indicated that the X2 factor affected the response variable more than X3. As shown in , the angle of repose decreased with increasing leucine content, and changed slightly as the F68 content increased. The leucine and F68 reduced the powder angle of repose as shown by the negative coefficients for X2 and X3, respectively (Equation 2).
Figure 2. Response surface plots for the mannitol (X1), l-leucine (X2) and F68 (X3) on the repose angle (Y1) – A, the GSD (Y2) – B, FPF (Y3) – C, and MMAD (Y4) – D.
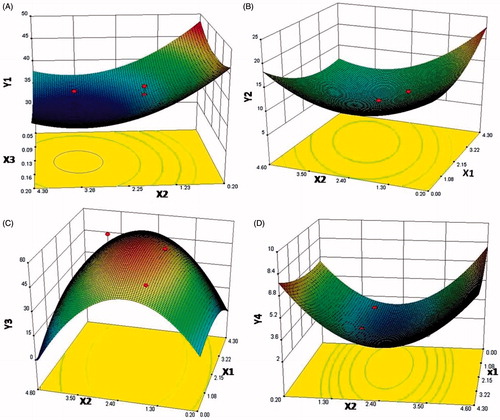
shows the response surface plot for the mannitol concentration (X1) and leucine concentration (X2) for FPF (Y3). The response surfaces indicated that the factor of X2 exhibited higher “F” values than X1 (), which indicated that X2 more significantly affected the response variable than X1. The presence of leucine yielded positive X2 coefficients (Equation 4), whereas mannitol was negative. Mannitol increased the FPF for dry powders despite a large amount of mannitol decreasing the aerosolization performance. Increasing the leucine fraction improved the powder flowability and dispersion because leucine exhibited hydrophobic and surfactant-like properties due to its essential branched chains. Leucine molecules on the droplet surface form such that an amide group (hydrophilic) is facing the aqueous phase and an isobutyl group (hydrophobic) is facing the air phase to form a film that collapses when water evaporates (Raula et al., Citation2007). First, the wrinkle formation shown in decreased the contact surface between particles, which improves the powder dispersion. Second, leucine is a surface-active molecule that can enrich at the air–water surface of droplets. This enriching at the surface decreases the surface tension and droplet size (Peskin & Raco, Citation1963). Third, leucine may be a useful anti-adherent to keep powder particles separated and reduce adhesion (Chougule et al., Citation2007). In addition, F68 containing leucine can produce large, light, respirable powders that improve the dry powder flowability (Padhi et al., Citation2006).
shows that the combined effect the mannitol and leucine concentrations had on the GSD (Y2). shows the response surface plot for the effect of X1 and X2 on MMAD (Y4). Both response surfaces indicated that the X2 factor was higher for “F” than X1 (), which indicated that X2 more significantly affected the response variable than X1. shows leucine had a positive effect, whereas mannitol had a negative effect. The presence of leucine and mannitol in combination can maximize the powder yields (Yu et al., Citation2010). Mannitol acts as an effective non-reducing sugar stabilizing agent to protect proteins in many studies (Maa et al., Citation2004; Schule et al., Citation2008). The aerodynamic properties of the powder formulation were attributed to a combination of the formulation excipients (mainly leucine), submicrometer particle size and DPI dispersion mechanism used to aerosolize the powder.
In vitro characterization of zanamivir DPIs
The optimum formulation was selected based on minimizing the angle of repose (Y1), mass median diameter (Y2) and MMAD (Y4), while maximizing the FPF(Y3). An overall desirability (OD) function based on all of the investigated formulation variables was used to predict the range of variables with the optimum formulation (Seville et al., Citation2007). The optimum formulation procedure was automatically conducted using Design Expert 8.0.6 (Stat-Ease Inc., Minneapolis, MN). To confirm the validity of the calculated optimal factors and predicated responses, a new zanamivir DPI batch was prepared using the optimum formulation, and the responses were observed ().
Table 5. The observed and predicted response values for the zanamivir DPIs.
The OD was 0.942, which is close to 1, and the validity of the prediction model was 101.76%, 95.9%, 100.89% and 103.85% for the response angle, GSD, FPF and MMAD, respectively. These results suggest that the optimized formulation is desirable.
Scanning electron microscopy
As evidenced by the scanning electron dry powder image shown in , the optimized powder was a hollow spherical particle with an extremely wrinkled surface. This structure can be explained by the presence of leucine. The leucine is a weak surfactant with a hydrophobic nature, which causes it to accumulate at the air/liquid interface. Pure spray-dried leucine forms hollow particles with low densities (Lucas et al., Citation1999; Najafabadi et al., Citation2004), which demonstrates it can form a shell and has the potential to encapsulate when the particles are correctly designed. Leucine has the low molecular weight of 131.17 g/mol and low solubility in water of 22 mg/ml. Therefore, leucine is expected to quickly become supersaturated during the drying process assuming a sufficient initial saturation. Leucine may encapsulate other molecules and form a shell. A corrugated surface further assists in the dispersibility by minimizing the contact area, which yields a better in vitro deposition.
DSC and XRPD
The thermograms and diffraction patterns are shown in and . The thermogram for raw zanamivir exhibited a peak temperature of 290.23 °C which signified melting with degradation. The raw drug was mainly amorphous; however, some crystalline diffraction peaks were observed and certified by XRPD. The raw drug and excipients in a physical blending, spray-dried excipients powder, the zanamivir DPI powders and Relenza® exhibited one endothermic phase transitions at 164.83, 148.89, 162.39, 145.83 °C, respectively. X-ray powder diffraction is a powerful tool widely used to evaluate the crystalline state. The diffraction patterns indicated that the powders were all crystalline. The characteristic diffraction peaks for raw zanamivir appeared at a 2θ angle of 17.456° and the characteristic diffraction peaks for the spray-dried excipients appeared at 2θ angles of 5.967° and 19.017°. The characteristic diffraction peaks of raw zanamivir and spray-dried excipients in the zanamivir DPI powder were entirely appeared; however, the degree of crystallinity decreased, which implies the crystallinity was lost and became amorphous. This decreased crystallinity may be due to the decreased particle size relative to the raw zanamivir powder. The X-ray diffraction peak height is affected by the crystal size and particle crystallinity (Lee et al., Citation2006). The characteristic diffraction peak of raw zanamivir also appeared in Relenza®, but the degree of crystallinity decreased more than the zanamivir DPI due to the preparation technology. Milling seemed to have more influence on the crystallinity of zanamivir than spray drying.
Moisture content
The water contents for raw zanamivir, mannitol, leucine and F68 before spray drying were 1.36 ± 0.25%, 0.89 ± .09%, 0.72 ± 0.04% and 0.96 ± 0.12%, respectively. After spray drying, the residual water content of the remaining dry powder decreased to 0.51 ± 0.04%. Moisture within the dry powder can influence the aerosol performance due to capillary forces acting at the solid–solid particle interfaces (Hickey et al., Citation2007). The low water content is required for respirable dry powders.
Moisture absorption
The moisture absorption profiles corresponding to the optimized formation and Relenza® are shown in . Compared to Relenza®, the zanamivir DPIs are less sensitive to moisture at high RHs. Relenza® absorbed a significant amount of water at 66%, 75% and 85% RH (weight change of approximately 1.38%, 2.18% and 3.72%, respectively). In contrast, the weight change for the zanamivir DPIs was negligible upon increasing the RH to 66%. The zanamivir DPIs exhibited better anti-hygroscopic properties than Relenza®.
Pharmacokinetic study
The obtained concentration–time profiles are shown in , and the pharmacokinetic data are shown in . The Cmax was 1435.93 ± 218.5 and 1730.75 ± 264.3 ng/mL for Relenza® and zanamivir DPIs, respectively, with a Tmax of 0.083 h. As shown in , the relative bioavailability of the zanamivir DPIs was 116%. These results imply that the zanamivir DPIs were effectively delivered to the lungs with a similar pharmacokinetic performance to Relenza®.
Figure 7. Mean concentration–time profile (n = 6) for zanamivir DPIs and Relenza® after endotracheal administration.
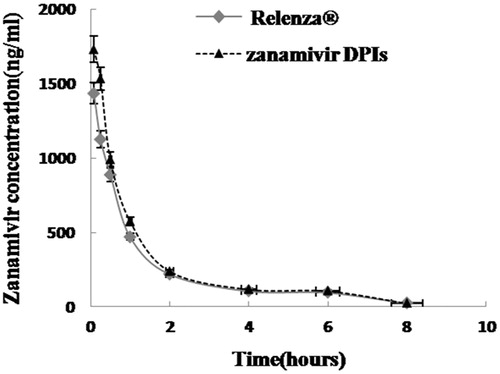
Table 6. Pulmonary pharmacokinetic parameters of zanamivir DPI and Relenza®.
Monitoring the pulmonary delivery via fluorescent imaging
To visualize and evaluate the pulmonary delivery of the powders in rats, the fluorescence of their whole body was measured immediately after administering dry powders to the lungs. The dry powder formulation containing Cy7 and the in vitro characterization are shown in . The fluorescence could be detected in rats following the pulmonary administration of the dry powder (). The dry powders successfully reached the lungs after administration, which might be due to the dissolution of Cy7. The fluorescence strength in the lungs reached a maximum at 1.5 h and then decreased with time. The fluorescence in the liver was observed at approximately 2 h and increased gradually.
Figure 8. Live in vivo imaging of the zanamivir DPI (A), the dry powder formulation containing Cy7 (B) and organs after endotracheal administration.
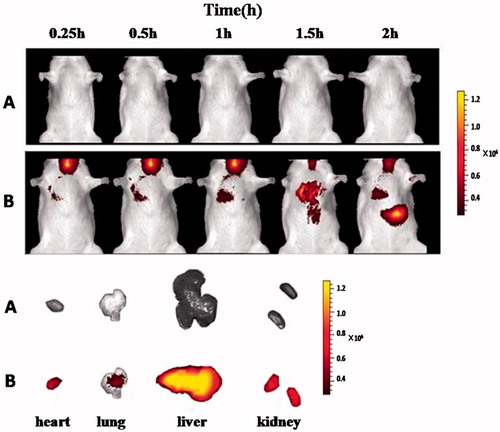
Table 7. The dry powder formulation containing Cy7 and its in vitro characterization.
Conclusions
Powders were prepared via spray drying using excipients such as trehalose, lactose, mannitol, leucine and glycine. Mannitol and leucine were selected to reduce the hygroscopicity. The zanamivir dry powder formulations were optimized via a central composite design considering mannitol, leucine and poloxamer 188 as the independent variables. The optimized zanamivir dry powder formulation was further characterized for via surface morphology, DSC, XPRD and water content studies to demonstrate its suitability as a dry powder for inhalation. A promising in vitro aerosol performance observed for the zanamivir DPIs suggests a high deep lung deposition of the drug. In addition, the zanamivir DPIs were less hygroscopic than Relenza®. The in vivo study data indicated that zanamivir DPI was effectively delivered to the lungs after endotracheal administration using penn-century powder insufflators and exhibited similar in vivo pharmacokinetic performance to Relenza®. The results from this study show the potential of spray-dried zanamivir DPI for delivering drugs to the deep lung.
Declaration of interest
We are grateful for the financial support from the National Natural Science Foundation of China (Grant No. 81202466) and the Important National Science & Technology Specific Projects (Grant No. 2012ZX09301003-001-009) of China.
References
- Asada M, Takahashi H, Okamoto H, et al. (2004). Theophlline particle design using chitosan by the spray drying. Int J Pharm 270:167–74
- Batycky RP, Lipp MM, Niven RW. (2004). Use of simple amino acids to form porous particles. US patent 7:252,840
- Bevard V, Lesniewska E, Andres C, et al. (2002). Dry powder inhaler: influence of humidity on topology and adhesion studied by AFM. Int J Pharm 232:213–24
- Bivas-Benita M, Zwier R, Junginger HE, Borchard G. (2005). Non-invasive pulmonary aerosol delivery in mice by the endotracheal route. Eur J Pharm Biopharm 61:214–18
- Bosquillon C, Lombry C, Préat V, Vanbever R. (2001). Influence of formulation excipients and physical characteristics of inhalation dry powders on their aerosolisation performance. J Control Release 70:329–39
- Chan HK, Clark AR, Feeley JC, et al. (2004). Physical stability of salmone calcitonin spray-dried powders for inhalation. J Pharm Sci 93:792–804
- Chougule MB, Padhi BK, Jinturkar KA, Misra A. (2007). Development of dry powder inhalers. Recent Pat Drug Deliv Formul 1:11–21
- Cline D, Dalby R. (2002). Predicting the quality of powders for inhalation from surface energy and area. Pharm Res 19:1274–7
- Cook RO, Pannu RK, Kellaway IW. (2005). Novel sustained release microsphere for pulmonary drug delivery. J Control Release 104:79–90
- Cox RJ, Mykkeltvedt E, Sjursen H, Haaheim LR. (2001). The effect of Zanamivir treatment on the early immune response to influenza vaccination. Vaccine 19:4743–9
- Donovan MJ, Gibbons A, Herpin MJ, et al. (2011). Novel dry powder inhaler particle-dispersion systems. Ther Deliv 2:1295–311
- Duret C, Wauthoz N, Merlos R, et al. (2012). In vitro and in vivo evaluation of a dry powder endotracheal insufflator device for use in dose-dependent preclinical studies in mice. Eur J Pharm Biopharm 81:627–34
- Gliniski J, Chavepeyer G, Platten JK. (2000). Surface properties of aqueous solutions of l-leucine. Biophys Chem 84:99–103
- Hickey AJ, Mansour HM, Martin JT, et al. (2007). Physical characterization of component particles included in dry powder inhalers. I. Strategy review and static characteristics. J Pharm Sci 96:1282–301
- Khodadoust S, Hadjmohammadi M. (2011). Determination of N-methylcarbamateinsecticides in water samples using dispersive liquid–liquid microextraction and HPLC with the aid of experimental design and desirability function. Anal Chim Acta 699:113–19
- Lechuga-Ballesteros D, Charan C, Stults CLM, et al. (2008). Trileucine improves aerosol performance and stability of spray-dried powders for inhalation. J Pharm Sci 97:287–302
- Lee HK, Kwon JH, Park SH, Kim CW. (2006). Insulin microcrystals prepared by the seed zone method. J Cryst Growth 293:447–51
- Lucas P, Anderson K, Potter UJ, Staniforth JN. (1999). Enhancement of small particle size dry powder aerosol formulations using an ultra low density additive. Pharm Res 16:1643–7
- Maa YF, Ameri M, Shu C, et al. (2004). Influenza vaccine powder formulation development: spray-freeze-drying and stability evaluation. J Pharm Sci 93:1912–23
- Najafabadi AR, Gilani K, Barghi M, Rafiee-Tehrani M. (2004). The effect of vehicle on physical properties and aerosolisation behaviour of disodium cromoglycate microparticles spray dried alone or with l-leucine. Int J Pharm 285:97–108
- Ogain ON, Li J, Taiber L, et al. (2011). Particle engineering of materials for oral inhalation by dry powder inhalers. I. Particles of sugar excipients (trehalose and raffinose) for protein delivery. Int J Pharm 405:23–35
- Padhi B, Chougule M, Misra A. (2006). Optimization of formulation and characterization of large respirable powders containing high therapeutic payload. Pharm Dev Technol 11:465–75
- Peskin RL, Raco RJ. (1963). Ultrasonic atomization of liquids. J Acoust Soc Am 35:1378–81
- Raula J, Kurkela JA, Brown DP, Kauppinen EI. (2007). Study of the dispersion behavior of l-leucine containing microparticles synthesized with an aerosol flow reactor method. Powder Technol 177:125–32
- Raula J, Laehde A, Kauppinen EI. (2008). A novel gas phase method for the combined synthesis and coating of pharmaceutical particles. Pharm Res 25:242–5
- Raula J, Thielmann F, Naderi M, et al. (2010). Investigations on particle surface characteristics vs. dispersion behaviour of l-leucine coated carrier-free inhalable powders. Int J Pharm 385:79–85
- Schule S, Schulz-Fademrecht T, Garidel P, et al. (2008). Stabilization of IgG1 in spray-dried powders for inhalation. Eur J Pharm Biopharm 69:793–807
- Seville PC, Learoyd TP, Li HY, et al. (2007). Amino acid modified spray dried powders with enhanced aerosolisation properties for pulmonary drug delivery. Powder Technol 178:40–50
- Stahl K, Claesson M, Lilliehorn P, et al. (2002). The effect of process variables on the degradation and physical properties of spray dried insulin intended for inhalation. Int J Pharm 233:227–37
- Steckel H, Brandes HG. (2004). A novel spray-drying technique to produce low density particles for pulmonary delivery. Int J Pharm 278:187–95
- Steckel H, Bolzen N. (2004). Alternative sugars as potential carriers for dry powder inhalations. Int J Pharm 270:297–306
- Yang Y, Yang ZW, Ren YF, et al. (2014). Effects of formulation and operating variables on Zanamivir dry powder inhalation characteristics and aerosolization performance. Drug Deliv 21:480–6
- Yu Z, Xiaoli W, Xia L, et al. (2010). High azithromycin loading powders for inhalation and their in vivo evaluation in rats. Int J Pharm 395:205–14