Abstract
A number of navigation systems used for total knee replacement surgery currently require the insertion of a distal femoral reference sensor pin, which is placed anterior to posterior just superior to the level of the knee joint. There is potential for the posterior neurovascular bundle to be damaged during the insertion of this sensor device. The aim of this cadaveric study was to identify the structures at risk during insertion of the distal femoral sensor, and determine whether a safe zone for insertion could be identified.
Sixteen cadaveric lower limbs (8 pairs) were studied. In each knee Steinman pins were passed from anterior to posterior, 5 cm proximal to the level of the femoral articular cartilage, directly AP and angled at 30° passing medially or laterally. All pins that were passed directly from anterior to posterior and from lateral to medial passed within 5 mm of a major neurovascular structure, while 62.5% of pins passing from medial to lateral passed within 5 mm of a major neurovascular structure.
The popliteal vessels and the sciatic nerve are at risk of injury from a navigation pin or drill placed in the distal femur during knee navigation. Caution should be exercised in passing these pins and alternate methods of fixing femoral sensors should be considered.
Introduction
The navigation technology used in total knee arthroplasty is an interactive operative monitoring system designed to improve surgical performance, increase accuracy of bony resections, improve post-operative limb alignment, and improve ligament and soft tissue balancing. In addition, it provides a potential source of medico-legal evidence. The Stryker Navigation System (Stryker Leibinger, Kalamazoo, MI) employs three sensor trackers positioned at the iliac crest, distal femur and proximal tibia. Each tracker is mounted over an anchoring pin consisting of a self-tapping screw design with anti-rotation grip. The pins have a diameter of 4 mm and range in thread length from 25 to 45 mm, in 5-mm increments. The pins may be inserted in a uni- or bi-cortical fashion to ensure rigid fixation and maintenance of position throughout the surgical procedure.
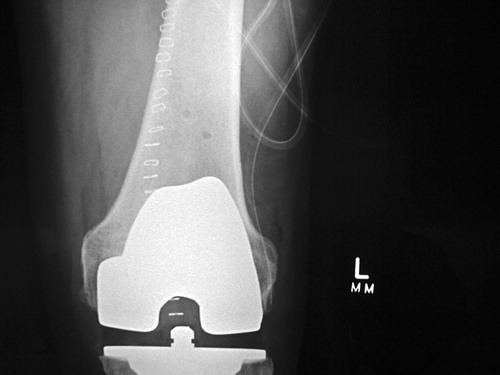
Our clinical experience is that a bicortical fixation technique provides greater stability of the distal femoral sensor pin, and this is the recommended method of fixation (). However, this technique exposes the surgical team to a potential danger in relation to the neurovascular bundle, which at this level is intimately related to the posterior surface of the femur Citation[1].
Figure 1. X-ray showing bicortical penetration of the distal femur from a navigation tracking device.
Damage to major neurovascular structures secondary to pin and screw placement in orthopaedic procedures is a recognized potential complication, and studies have been performed to define this risk in certain instances Citation[2–4]. Furthermore, the potential for damage to neurovascular structures during knee surgery has been identified Citation[5–9]. However, to our knowledge, since the introduction of knee navigation no study has been undertaken to investigate potential neurovascular complications associated with the pre-drilling and insertion of navigation pins.
The aims of this study were to accurately define the anatomical structures that are potentially at risk in distal femoral pin placement; to determine the relative contiguity of the distal thigh neurovascular structures to pins placed in specific locations at the distal femur; and to determine whether a safe zone exists in relation to distal femoral pin placement.
Materials and methods
Sixteen cadaveric lower limbs were selected for study, comprising 8 matched pairs of right and left limbs. A standard longitudinal midline skin incision was performed superior to the patella. The anterior aspect of the femur was reached through a longitudinal quadriceps split.
In each limb three separate exit points were investigated using a pre-drilled 3.2-mm Steinmann pin, drilled from an anterior to posterior direction. The drill holes were placed using a protractor: the first at 90° to the anterior femoral cortex; the second 1 cm lateral and at 30° relative to the anterior pin; and the third 1 cm medial and at 30° relative to the anterior pin.
Consistent with the manufacturer's recommendations, all pins were pre-drilled and inserted at a level located 5 cm proximal to the proximal margin of the anterior femoral condylar articular cartilage. The cadavers were then rolled over and a popliteal fossa soft tissue dissection performed. The tendons of the hamstrings and biceps femoris were identified and reflected. Care was taken not to disturb the position of the neurovascular structures. Pins were passed in 3 directions, as described previously, and all exit paths were recorded in relation to the neurovascular structures. A caliper was used to measure the distance from the exit point to the popliteal artery, vein and sciatic nerve. In cases where the bifurcation of the sciatic nerve was proximal to the exit level, the distance from the exit point to the common peroneal or tibial nerve, whichever was closest, was recorded. All measurements were performed separately for each of the 3 pins.
All neurovascular structures were carefully examined for evidence of damage due to the drilling. To define the consistency of exit-hole placement, we recorded the shortest distance between the pin exit hole and the medial femoral cortex and femoral articular surface.
Results
The results of the 3 groupings of pin placement demonstrated a variable pattern of risk to the neurovascular bundle. For pins passed directly anterior to posterior, 9 of 16 (56.25%) passed directly through the popliteal vein (). The remaining 7 of 16 (43.75 %) pins exited within 5 mm or less of the popliteal vein. These results are summarized in .
Figure 2. Anterior to posterior pin passing through femoral vein (blue), and close to femoral artery (orange) and sciatic (common peroneal) nerve. [Color image is available in online edition.]
![Figure 2. Anterior to posterior pin passing through femoral vein (blue), and close to femoral artery (orange) and sciatic (common peroneal) nerve. [Color image is available in online edition.]](/cms/asset/66d8c7e5-2906-42c8-8311-d545d2a04c19/icsu_a_116337_f0002_b.jpg)
Table I. Summary of results with respect to most significant neurovascular structure threatened by passage of femoral pin.
For anterolateral to posteromedial pins, 6 of 16 (37.5%) passed directly through the popliteal artery. In 9 of 16 cases (56.25%) the pin track passed within 5 mm or less of the artery. In one case (6.25%) the pin passed directly through the vein and was still within 5 mm or less of the artery.
The anteromedial to posterolateral group showed 4 of 16 (25%) pins passing through the common peroneal or sciatic nerve. Six of 16 (37.5%) pins passed within 5 mm or less of one of these nerves, and 5 of 16 (31. 25%) pins within 6–10 mm. One of the 16 pins (6.25%) passed more than 10 mm from these nerves.
Summarizing the results of this series reveals that, when passing the pin directly anterior to posterior, as in the actual surgical procedure, there is a 100% occurrence of being within 5 mm of the popliteal vein. When placing the pin in an anterolateral to posteromedial direction there is a 100% occurrence of being within 5 mm of the popliteal artery. When placed anteromedial to posterolateral, 60% of pins were within 5 mm of the common peroneal or sciatic nerve.
It is important to note that there was an observed difference in the proximity of the vascular and neural structures posterior to the knee. The popliteal artery and vein were noted to be intimately related to the periosteum of the posterior femoral cortex. However, in all cadaveric limbs, the neural structures (the sciatic nerve and its terminal divisions) were observed to be 10 mm or more from the posterior femoral cortex at the studied level.
Discussion
Neurovascular injury posterior to the knee joint is a well-described potential complication of many surgical procedures in this region Citation[5–9]. Such injury may result from over-penetration of a drill, insertion of a reference pin beyond the far cortex of the distal femur, trauma from mechanical saws, or past-pointing of a depth gauge. Significant vessel pseudoaneurysm, or loss of structural integrity, may result from even a single-sided vessel wall trauma. It is therefore essential to have a clear understanding of the relationship between the neurovascular structures posterior to the knee joint when considering any surgery in this area.
Several authors have attempted to accurately define this relationship through the use of imaging studies. Zaidi et al. Citation[9] used ultrasound techniques to study the popliteal artery at a level 1.5 cm below the tibial articular surface. They found that at 90° of flexion the artery lay closer to the posterior tibial surface than in full extension. Shiomi et al. Citation[10] attempted to determine the angle of knee flexion which placed the popliteal artery at the least risk of injury during surgical procedures on the knee. The results of this study showed that, at the level of the joint line, flexion increased the distance between the artery and posterior cortical surface. These studies have limitations in that they were both performed with the subjects in a lateral position that does not accurately reproduce the surgical scenario. Zaidi et al. Citation[9] were also criticized on the grounds that the pressure from the ultrasound probe may have altered the anatomical relationship of the involved structures.
Smith et al. Citation[11] studied the relationship of the popliteal artery at the level of knee replacement resection with the subjects in a supine position. They found that, even including the effect of gravity, knee flexion does not guarantee posterior movement of the neurovascular structures at the level of the knee.
Our series demonstrated an intimate relationship of the popliteal artery and vein with the posterior femoral cortex at the studied level. It can be presumed, on this basis, that this subjects them to significant potential risk during placement of reference pins in navigated knee surgery. It is important to note that this was a cadaveric study and there is thus potential for an altered relationship between the neurovascular structures as compared with more mobile vascularized human tissue. All pins were placed with the cadaveric knees in full extension, which may also confound the normal relationship of these structures to the posterior aspect of the knee, though it is in this position that the pins are usually inserted during knee navigation. We have based our results on the presumption that the above factors do not significantly alter the usual relationship between the distal femur and the neurovascular structures observed in living tissue.
Accepting these potential limitations, we observed the existence of a definite, reproducible risk to the popliteal neurovascular structures when placing a bicortical reference pin. The popliteal artery and vein were observed to be most at risk due to their apparent intimate relationship to the posterior femoral cortex. We recommend the placement of the distal femoral reference pin in a posterolateral direction to minimize the risk of neurovascular injury. We recognize that this can cause a problem in that the mounted tracker may not be as detectable by the infra-red receiver.
Alternative approaches include placing the pin directly anterior to posterior lateral to the midline. This may, however, create a stress riser in the supracondylar region, as there will be two cortical breaches in the distal femoral circumference less than 180° apart. The other obvious alternative is to place the distal femoral reference pin in a unicortical fashion. Loosening of the reference pin intra-operatively and consequent inaccuracies in reference readings are likely outcomes of this alternative. Future directions in design may involve the development of reference guides that allow stable fixation without the need for breach of the posterior femoral cortex.
References
- Boileau J C. Grant's Atlas of Anatomy. Sixth Edition., J C Boileau. Williams & Wilkins, Baltimore 1972; 285–289, Figures
- Wasielewski R C, Lawrence A, Cooperstein M D, et al. Acetabular anatomy and the transacetabular fixation of screws in total hip arthroplasty. J Bone Joint Surg Am 1990; 72(4)501–50
- Keating M, Ritter M A, Faris P M. Structures at risk from medially placed acetabular screws. J Bone Joint Surg Am 1990; 72(4)509–11
- Post W R, King S S. Neurovascular risk of bicortical tibial drilling for screw and spiked washer fixation of soft-tissue anterior cruciate ligament graft. J Arthroscopy 2001; 17(3)244–7
- Berger C, Anzbock W, Lange A, et al. Arterial occlusion after total knee arthroplasty: Successful management of an uncommon complication by percutaneous thrombus aspiration. J Arthroplasty 2002; 17(2)227–9
- Mureebe L, Gahtan V, Kahn M, et al. Popliteal artery injury after total knee arthroplasty. The American Surgeon 1996; 62: 366–8
- Roth J H, Bray R C. Popliteal artery injury during anterior cruciate ligament reconstruction. J Bone Joint Surg Br 1988; 70: 840
- Rush J H, Vidovich J D, Johnson M A. Arterial complications of total knee replacement: The Australian experience. J Bone Joint Surg Br 1987; 69(3)400–2
- Zaidi S H, Cobb A G, Bentley G. Danger to the popliteal artery in high tibial osteotomy. J Bone Joint Surg Br 1995; 77(3)384–6
- Shiomi J, Takahashi T, Imazato S, et al. Flexion of the knee increases the distance between the popliteal artery and the proximal tibia: MRI measurements in 15 volunteers. Acta Orthop Scand 2001; 72(6)626–8
- Smith P N, Gelinas J, Kennedy K, et al. Popliteal vessels in knee surgery: A magnetic resonance imaging study. Clin Orthop 1999; 367: 158–64