Abstract
Navigation of the acetabular cup in total hip replacement (THR) is used to improve the reproducibility of acetabular component positioning. When the palpation of anatomic landmarks, which is necessary to determine the pelvic coordinate system, is performed epicutaneously, the question as to how uneven soft tissue distribution can influence navigation accuracy arises.
To obtain data, the questionable soft tissue thickness was measured in 72 patients scheduled for THR. In addition, distances between the landmarks were recorded. On the basis of this information, we were able to calculate the expected misinterpretation of the anteversion given by a navigation system for each patient.
The calculations suggest that a navigation system would have underestimated the anteversion on average by 2.8° ± 1.8°. The median of anteversion misinterpretation was 2.4° and its 95% confidence interval was calculated to be 2.2°–3.0°. No correlation with substantial significance between anteversion misinterpretation and the patients' biometrical data could be found.
According to the current knowledge, acetabular cups in THR should be positioned within a range of 30°–50° of inclination and 10°–30° of anteversion. In comparison with these permitted ± 10° windows, the amount of misinterpretation that was found due to uneven soft tissue distribution seems to be acceptable.
Objective
Despite the fact that the vast majority of patients are satisfied after a primary total hip replacement (THR), a small group of patients have disappointing results. The foremost mechanical problems are impingement and dislocation. Publications focusing on dislocation reveal an incidence of 0.4% to ∼6% Citation[1–4]. Lewinnek et al. Citation[5] as well as McCollum and Gray Citation[6] described a correlation between position of the acetabular cup and impingement and dislocation. In addition, it was found that the position of the implant also contributes to its longevity Citation[7].
Hence, outliers concerning component positioning have to be avoided. It was shown that variability of cup position can be reduced by the use of computer-assisted navigation systems Citation[8].
Quantitatively, clinical reliability of navigation systems for the acetabular cup was proven only for CT-based systems. These systems require a preoperative CT of the pelvis, which has to be transferred to the navigations system and then postprocessed by manual effort in order to extract information of the bone surface, which takes half an hour. Intra-operative handling needs some training and adds 10–20 min (depending on the grade of routine) to the standard surgical procedure. Because these additional tasks are not needed in image-free navigation systems, this method has become more popular in orthopedic surgery.
When using an image-free hip cup navigation system, the surgeon has to digitize the frontal pelvic plane of the patient to determine the individual pelvic coordinate system for cup positioning. According to Cunningham, the frontal pelvic plane is defined by both anterior superior iliac spines and both tuberculae pubis Citation[9] (). Rather than digitizing the latter two landmarks individually, the surgeon palpates in common practice only one point that is as close to the symphysis as possible.
Figure 1. Symbolic depiction of geometric (w and o., blue), ultrasonographic measurement (li, r. i., and s. y., red) and geometric calculation (h, green). [Color version available online.]
![Figure 1. Symbolic depiction of geometric (w and o., blue), ultrasonographic measurement (li, r. i., and s. y., red) and geometric calculation (h, green). [Color version available online.]](/cms/asset/3e0f24b0-9a77-44e1-be8a-b034cd5d4b46/icsu_a_122927_f0001_b.jpg)
Currently, the major concern about image-free hip cup navigation is this palpation procedure. Between skin and bone, the latter being the actual target of palpation, lies subcutaneous tissue with unknown thickness. Even though some publications are available giving information about subcutaneous fat distribution around the body, no distinctive information is available concerning its thickness superficial to the mentioned landmarks. The navigation procedure cannot be accurate if the subcutaneous fat in front of the three landmarks is distributed unequally. Therefore, it was the goal of the presented study to provide figures for subcutaneous fat distribution at the landmarks of interest and calculate the resulting misinterpretation of cup anteversion dependent on the amount of overlying soft tissue. To find possible correlations between biometrical parameters and soft tissue distribution was an additional motivation of the study.
Materials and methods
Clinical setting
Data of 72 consecutive patients were prospectively collected. All 72 patients were scheduled for primary THR. Ultrasonographic measurements of pelvic soft tissue and quantification of the pelvic geometry were carried out immediately prior to preparing and draping in the operation theatre. To determine the minimal soft tissue thickness between skin surface and bony landmarks, B-mode ultrasound was used (Siemens SL1, Erlangen, Germany). According to the manufacturer, the ultrasound probe's accuracy in sound wave direction is 0.5 mm.
Using the ultrasound probe, manual pressure was applied in order to achieve minimal soft tissue thickness comparable with the conditions that are used during the palpation procedure in image-free cup navigation. We found that, especially, examination of the symphysis is mostly not only uncomfortable for the patient, but also painful. Therefore, the ultrasound examination was performed under anesthesia, while the patients were already placed on the operation table in supine position awaiting THR surgery.
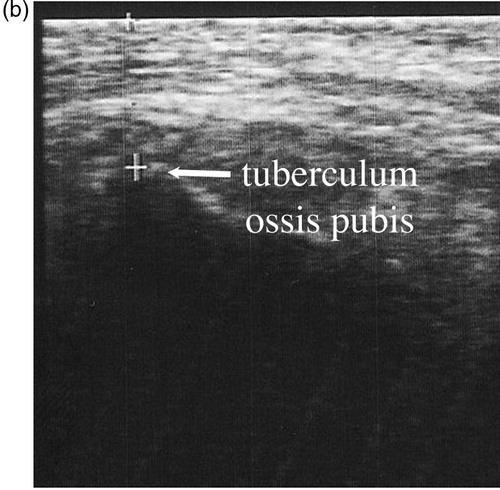
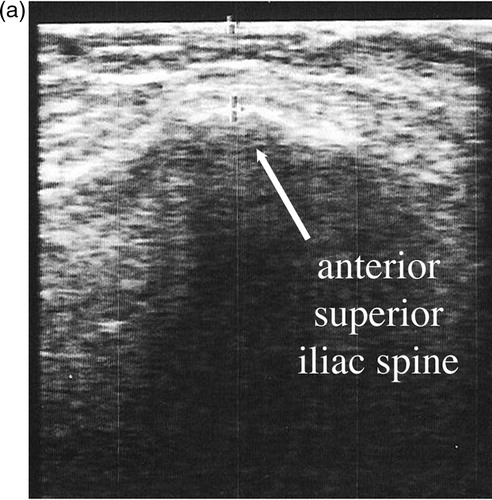
Bony landmarks of interest were the left and right anterior superior iliac spine (ASIS; ) and the most anterior parts of the pubic bone, which were in most patients the tuberculae pubis (). According to the clinical handling of the navigation system, only one symphysic landmark was recorded. To have the best access to the ASIS, the abdominal fat had to be pushed medially. In the case of the symphysic landmark, the presymphyseal fat was pushed cranially. The correct anatomical site was located by manual palpation before the ultrasound examination was performed.
Figure 2. Exemplary depiction of ultrasound examination of one patient. (a) Static, sagittal B-mode image of the anterior superior iliac spine. In this particular case, the distance from skin to bone measured 10 mm. (b) Static, sagittal B-mode image of the symphysic area. Here, the distance from skin to bone measured 17 mm.
In addition, the distances between both ASIS and between ASIS and symphysis were measured using a jig with 0.5 cm increments ().
Data evaluation
Trigonometric calculations were performed to allow an estimation of the angular error in image-free cup navigation as a result of an uneven subcutaneous fat distribution at the three landmarks (). The following equations were used to calculate
the height of the triangle defining the frontal pelvic plane
the difference between soft tissue in front of the symphysis and ASIS
and the anteversion misinterpretation (45° inclination assumed)
Correlation between effective misinterpretation of the anteversion and body weight, body mass index, and pelvic width and height (distance between both ASIS) was tested for male, female, and all patients using Pearson's correlation.
Results
In the examined 47 female and 25 male patients with osteoarthritis of the hip, the average body weight was 78.2 ± 14.8 kg at a height of 167.9 ± 8.1 cm. The body mass index was calculated to average 27.7 ± 4.6 kg/m2. The average distance between left and right ASIS was 25.1 ± 2.2 cm, whereas the distance between the ASIS and the middle of the symphysis averaged 15.3 ± 1.3 cm. On the basis of Equation (1), the height of the triangle defining the fronal pelvic plane was calculated to average 8.6 ± 1.5 cm ().
Table I. Summary of the patients' biometric data, ultrasound measurements, and statistical evaluation referring to misinterpretation of anteversion.
Soft tissue thickness in front of the ASIS was an average of 7.9 mm on either side (±2.4 mm right and ± 3.5 mm left). Averaged absolute difference between left and right ASIS soft tissue thickness was 1.2 ± 1.4 mm. The maximum left-to-right difference was 9 mm in one patient, whose distance between both ASIS was 32 cm, which equals 1.6° misinterpretation of frontal pelvic plane along the body length axis (z-axis).
Soft tissue thickness superficial to the pubic tubercula averaged 13.6 ± 4.1 mm in all 72 patients. With respect to the ASIS measurement, the soft tissue in front of the symphysic landmark was 5.7 ± 3.4 mm thicker. The differences in soft tissue thickness from ASIS to symphysis ranged from − 2.5 to 14.9 mm.
On the basis of 45° cup inclination, which corresponds to a sine of 0.71, these measurements would result in an average underestimation of the anteversion of 2.8° ± 1.8°. The median was 2.4°. The 95% confidence interval of the median of anteversion misinterpretation is 2.2°–3.0°. The extremes range from − 1.2° to 8.0° ().
Overall, a strong correlation between weight, body mass index, and pelvic width and height and misinterpretation of anteversion was not found (; ). In detail, misinterpretation of anteversion correlates with pelvic width in the male patients with low significance. An inverse relationship between misinterpretation of anteversion and pelvic height also with low significance was observed in female patients.
Figure 3. Plots of the individual misinterpretation of anteversion (°) v. s. (a) body weight (kg), (b) body mass index (kg/m2), (c) pelvic width (cm), and (d) height of the triangle defining the frontal pelvic plane (cm). Data of male patients are depicted with black triangles (▴) and female patients with white circles (O).
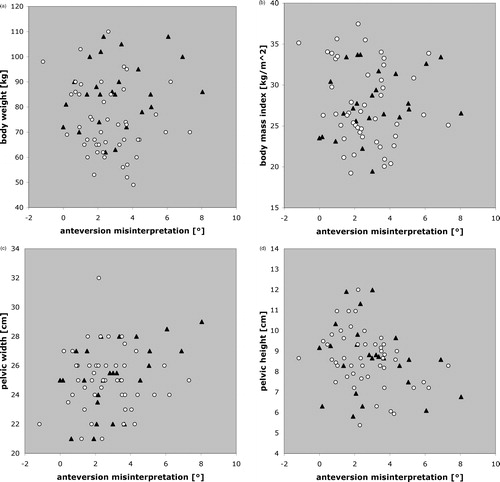
Table II. Data describing the earlier plotted correlations ().
Conclusions
A cup navigation system should support the surgeon in achieving an appropriate cup position to prevent impingement and dislocation within a range of motion needed for activities in the daily life of the individual patient. The strong relation between cup position and free prosthetic range of motion demands accuracy as one of the most important requirements in navigation systems Citation[10].
In the presented study, we analyzed the soft tissue distribution in front of the necessary bony landmarks as the alleged major factor affecting anteversion estimation by image-free cup navigation systems. Using ultrasound measurements, we studied how much the individual soft tissue distribution affects the system's estimation of the cup anteversion. Owing to its size, the ultrasound probe was harder to position and therefore subjectively slightly more distant to the symphysic area than to the ASIS. But it is speculative whether a smaller ultrasound probe with improved positioning would have reduced the methodical measurement error and therefore diminished the calculated average anteversion misinterpretation.
On the basis of the soft tissue distribution in 65 out of 72 patients (90%), a ± 5° accuracy could be reached. All patients were within a range of ± 8°. It is essential to point out that in all patients, except for one, the soft tissue distribution would have led a navigation system to underestimate the actual anteversion. Surgeons using these systems should be aware of this trend. In the next step, one should consider integrating this finding into the navigation system's algorithms as a bias. If + 3° were to be admitted as the new neutral anteversion, all examined patients would have been within a ± 5° interval and 85% of the examined patients within a ± 2.5° interval.
Correlation between individual misinterpretation of anteversion and the patient's biometric data with low significance was found in only two out of the 12 tested parameter subgroups (). Unfortunately, these findings were too weak to establish corrective factors for the individual patient based on body weight, height, or pelvic size.
The question as to how accurate a cup navigation system needs to be to serve clinical purposes arises. THR is a routine procedure and leads to very satisfying results in the vast majority of cases. In a few cases, inadequate positioning of the cup produces significant problems Citation[11]. In the first place, a cup navigation system should prevent these outliers. Lewinnek et al. Citation[5] found that outside a window of 40° ± 10° inclination and 15° ± 10° anteversion, the likelihood of a dislocation was up to four times higher. McCullom and Gray Citation[6] reported comparable findings. On the basis of their population of 441 cases of THR, the recommended range of cup positioning was an inclination of 30°–50° and an anteversion of 20°–40°. In a more recent study, a multivariate analysis was conducted in over two thousand cases of THR Citation[12]. Here, the risk of dislocation rose significantly in cases with inadequate positioning of both implant components (femoral stem and acetabular cup) in the transverse plane. The risk was also highly related to the patient's morbidity. No significant correlation was seen with respect to the seniority of the surgeon.
Besides impingement and luxation, early wear is another aspect of inadequate cup position. Even though the mechanical background of increased polyethylene wear due to higher load per area seems obvious Citation[13], it is controversial whether this effect actually occurs in vivo. Some groups report no increased wear correlated to implant position Citation[14], Citation[15], whereas others do Citation[7], Citation[16]. Yamaguchi et al. Citation[16] described the increased wear also as a result of impingement. Clearly, impingement of the femoral and acetabular component is related to implant positioning Citation[17].
The aforementioned publications recommend anteversion positions within a ± 10° range. A system that provides a ± 5° accuracy should be able to find outliers outside the mentioned range and can work as a digital safety belt. Given proper handling of the system and an appropriate palpation procedure, our findings currently do not suggest the necessity of performing skin and soft tissue to reach the bony landmarks by the use of a sharp-pointed probe, which is also available. However, future studies focusing on other accuracy and reproducibility topics, as well as addition of the shaft navigation and therefore introduction of more potential sources of errors, might require a decrease in the minor known soft-tissue uncertainty and might require usage of a sharp-pointed probe. Finally, it has to be mentioned that navigation of the cup takes care of only one THR component. Particularly, with respect to the impingement problem, additional navigation of the femoral stem component will increase the value of such systems in THR.
References
- Coventry M B, Beckenbaugh R D, Nolan D R, Ilstrup D M. 2,012 total hip arthroplasties. A study of postoperative course and early complications. J Bone Joint Surg A. m. 1974; 56: 273–284
- Woo R Y, Morrey B F. Dislocations after total hip arthroplasty. J Bone Joint Surg Am 1982; 64: 1295–1306
- Kohn D, Ruhmann O, Wirth C J. Die Verrenkung der Hüfttotalendoprothese unter besonderer Beachtung verschiedener Zugangswege. Z Orthop Ihre Grenzgeb 1997; 135: 40–44
- Demos H A, Rorabeck C H, Bourne R B, MacDonald S J, McCalden R W. Instability in primary total hip arthroplasty with the direct lateral approach. Clin Orthop 2001; 393: 168–180
- Lewinnek G E, Lewis J L, Tarr R, Compere C L, Zimmerman J R. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 1978; 60: 217–220
- McCollum D E, Gray W J. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop 1990; 261: 159–170
- Hirakawa K, Mitsugi N, Koshino T, Saito T, Hirasawa Y, Kubo T. Effect of acetabular cup position and orientation in cemented total hip arthroplasty. Clin Orthop 2001; 388: 135–142
- Leenders T, Vandevelde D, Mahieu G, Nuyts R. Reduction in variability of acetabular cup abduction using computer assisted surgery: a prospective and randomized study. Comput Aided Surg 2002; 7: 99–106
- Cunningham P. Cunningham's textbook of anatomy. A Robinson. Henry Frowde and Hodder Stoughton, London 1922, Pelvis
- Jaramaz B, Nikou C, Lattanzi R, DiGioia A M (2003) Accuracy requirements in THR surgical navigation—effect of cup alignment error. Proceedings of Computer Assisted Orthopaedic Surgery, MarbellaSpain, 2003, F Langlotz, B Davies, A Bauer. Steinkopff Verlag, Darmstadt, 158–159
- Fackler C D, Poss R. Dislocation in total hip arthroplasties. Clin Orthop 1980; 151: 169–178
- Jolles B M, Zangger P, Leyvraz P F. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty 2002; 17: 282–288
- Thomas W, Schug M. Über die Bedeutung der Position der Endoprothesenpfanne aus biomechanischer und klinischer Sicht – Vorschlag einer Klassifizierung. Biomed Tech (Berl) 1994; 39: 222–226
- Del Schutte H J r, Lipman A J, Bannar S M, Livermore J T, Ilstrup D, Morrey B F. Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J Arthroplasty 1998; 13: 621–626
- Kligman M, Michael H, Roffman M. The effect of abduction differences between cup and contralateral acetabular angle on polyethylene component wear. 2002; 25: 65–67, Orthopedics
- Yamaguchi M, Hashimoto Y, Akisue T, Bauer T W. Polyethylene wear vector in vivo: a three-dimensional analysis using retrieved acetabular components and radiographs. J Orthop Res 1999; 17: 695–702
- Bader R, Steinhauser E, Gradinger R, Willmann G, Mittelmeier W. Computergestützte Bewegungssimulation an Hüftendoprothesen mit Keramik-Keramik-Gleitpaarung. Analyse der Einflussparameter Implantat-Design und Position. Z Orthop Ihre Grenzgeb 2002; 140: 310–316