Abstract
Minimally invasive osteoid osteoma resection under computer tomography (CT) guidance has yielded good results and has become a viable alternative to open surgical procedures. Limited visualization of the actual drill position under CT guidance can frequently result in inadequate and malpositioned drilling, especially at lesions located in less accessible anatomic regions. With the conventional CT-guided drilling technique, sterility and general operative management poorly correlate with standard operating room conditions, and are at risk of intra- and postoperative complications. The new Iso-C3D® imaging device provides intraoperative multiplanar reconstructions. Adequate image quality and implementation in navigation systems were described for numerous indications. On the basis of multiplanar reconstructions, minimally invasive navigated techniques under three-dimensional surgical tool control become possible, which is not the case under fluoroscopic or CT-based navigation. We report on our first three cases of navigated Iso-C3D® osteoid osteoma resection. A minimally invasive resection of the nidus was possible under permanent multiplanar image control. No complications were encountered and all patients reported successful outcomes. Minimally invasive-based navigation offered an effective and reproducible surgical approach. Dependence on CT imaging for proper positioning and complications associated with use away from the operating room environment can be avoided.
Introduction
The successful surgical treatment of symptomatic osteoid osteomas has gained more support in recent years. The exact visual identification of osteoid osteomas remains technically demanding, and relevant complication rates associated with open surgical procedures are well known Citation[1–3]. Associated reoperations in 30% of cases after en bloc resections were described Citation[4]. Additionally, recurrences appear in ∼9% of reported clinical cases Citation[3–5]. Complex anatomic areas with poor access typically require an extensive surgical approach and are commonly associated with longer hospitalization, increased costs and a higher rate of other associated complications Citation[4].
Alternatively, minimally invasive surgical treatment under computer tomography (CT) guidance became the standard approach in many clinics Citation[1],Citation[6–8]. The percutaneous approach based on intraoperative CT imaging demonstrated good initial results, thus cure rates between 84 and 90% were described Citation[1], Citation[2], Citation[8]. Although the exact positioning of needles and hollow drills is well visualized with this technique, drill failures and incomplete excision of the lesions still commonly occur. Histologically confirmed incomplete excision rates of 55% have been described in previous studies with this technique Citation[2]. It is well understood that the most predictive factor of succesful therapy is the total resection of the nidus. If the resection of the lesion is unsuccessful as a result of inability to accurately visualize the drill-bit location or inadequate visualization of the lesion, spontaneously switching to an open procedure is not possible in the CT suite as it is not a fully equipped operating room (OR). Revision surgery in the OR then becomes necessary, which subjects the patient to secondary anaesthesia and increases the rate of associated complications. Overall complication rates of 24% and 14% reoperation rates were described with the percutaneous technique Citation[4].
Similar to the open approach, difficulties may still be encountered with the modified CT-guided approach. This is especially evident when operating on the more complex anatomical areas such as juxta-articular regions of the femoral neck or vertebral bodies. Additionally, the compromised sterile condition and general environment of the traditional CT suite often does not correlate well with the high level of surgical standards that governs the OR, leading to an increased incidence of iatrogenic infection Citation[1]. In contrast, navigated drilling of osseous lesions has been recently reported and is associated with a higher level of accuracy and reduced radiation time for both surgeons and patients Citation[9], Citation[10].
The studies so far have reported that CT- and fluoroscopy-based navigation techniques for minimally invasive procedures have coincided with several limitations. The approach with fluoroscopic navigation is held back by two-dimensional image visualization. CT-based navigation does not give the crucial real-time three-dimensional reconstructive feedback needed; furthermore, an intraoperative matching procedure is necessary. Consequently no minimal invasive technique is possible.
The use of Iso-C3D®-based imaging is capable of obtaining intraoperative multiplanar image reconstruction and provides good visualization of osseous lesions comparable with conventional CT reconstructions Citation[11], Citation[12]. The implementation of various navigation-based techniques has been previously described for the positioning of pedicle screws, acetabular screw placement and the drilling of osteochondral lesions Citation[9], Citation[10]. We report our initial experience and results of three clinical cases in which the Iso-C3D® navigation system was used in the percutaneous resection of osteoid osteomas. We compared these results retrospectively with previous cases at our institution, which were performed using the traditional method of the CT-guided approach.
Materials and methods
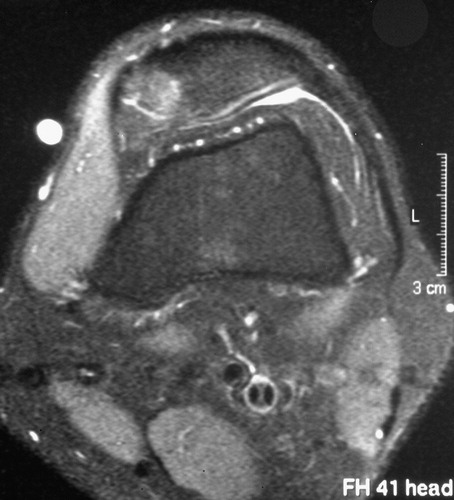
Three patients who originally presented with symptomatic osteoid osteoma lesions were included in this study. One patient had a lesion involving the retropatellar region, whereas the other patients' lesions were located in the proximal and middle third of the tibial shaft ( and ). All patients underwent preoperative diagnostic MRI scans. Conservative therapy yielded little to no improvement in either patient. In light of the failed conservative approach, the surgical alternatives were carefully outlined with all patients, and consent was obtained for the navigation aspect of their operations.
Figure 1. Preoperative diagnostics with an MRI scan of a patient with unspecific knee pain. The osteoid osteoma lesion was located in the postero-medial facet of the patella.
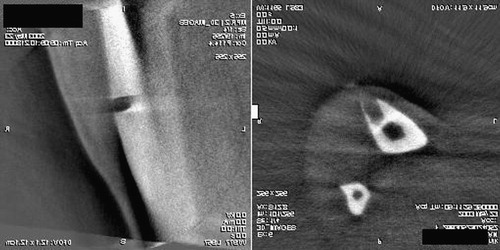
In all cases, the patient was placed in the proper position on a fully radiolucent carbon fiber table (VIWAS; Maquet Inc., Rastatt, Germany). Under general anaesthesia and standard sterile OR technique, an Iso-C3D® scan (Siemens Medical Inc., Erlangen, Germany) of the involved region was performed (). The Iso-C3D® unit was set to its highest level of quality, which calculates three-dimensional data based on 100 separate fluoroscopic images taken via a motorized C-arm that rotates 190° around the region of interest. The standard set-up of navigation system, Iso-C3D®, navigation camera and other related instruments was performed in relation to the specific extremity prior to the start of the operation (). The definition of the iso-center focused on the operated extremity is of utmost importance because the calculating area is limited by a cube of 12 × 12 × 12 cm3. A rotationstable dynamic reference base (DRB) was then fixed with Schanz screws to the patella and to the tibial shaft in the respective cases ( and ). Following the scanning, a secondary sterile draping was done, which covered the entire operative site with the exception of the top of the DRB. Once complete, a data transfer of the multiplanar images to the navigation system (Surgigate, Medivision, Switzerland) was done. The total site was then uncovered again. The osteoid osteoma lesions were visible in all multiplanar image reconstructions during all cases. The lesions were identified in frontal, sagittal and coronar planes. Trajectories in all multiplanar reconstructions were then planned on the navigation system. Using a percutaneous technique and under permanent navigated multiplanar image control, a 3.2-mm drill was placed directly in the nidus along the planned trajectories ( and ). A K-wire was then temporarily used for additional guidance, as a navigated 6.0-mm hollow drill bit was placed into the nidus followed by a final 8.0-mm hollow drill bit. Drilling was guided strictly by navigation. No additional radiological imaging was required during the actual procedures. The extracted bony material was sent to histology for confirmation in all three cases. A second intraoperative Iso-C3D® control scan was performed prior to skin closure to confirm the exact resection of each lesion. All three patients were kept for 24 h observation and were discharged uneventfully the next day. Finally, the details of the operation reports for these cases were carefully reviewed and compared with those for the last 12 conventional CT-based percutaneous drillings performed at our institution. Parameters such as total set-up, operation and radiation times were considered.
Figure 3. Intraoperative Iso-C3D® scan of the region of interest. The site was secondarily draped during the scanning procedure. Navigation tools are placed on an extra table.
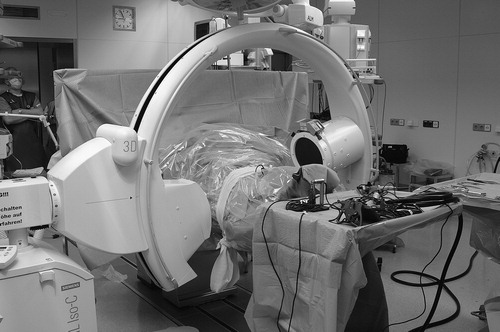
Figure 5. The DRB is fixed with two Schanz screws to the patella to achieve rotation stability during the drilling procedure. A navigated pointer was used to check the initial plausibility of the navigated tools.
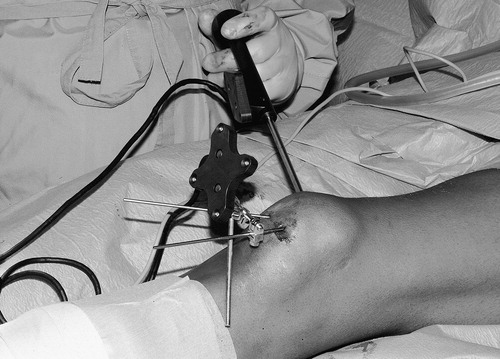
Figure 6. Fixation of the DRB in the proximal third of the tibia and plausibility check with the pointer.

Figure 7. (a) Percutaneous navigated drilling of the proximal tibial lesion with a hollow drill. (b) Intraoperative navigation screen in three multiplanar reconstructions. The actual position of the drill (green) is shown in reference to the good visible lesion on the tibia shaft. An aiming device helps to drill along the planned trajectories (red) and shows the distance from the start point. [Color version available online]
![Figure 7. (a) Percutaneous navigated drilling of the proximal tibial lesion with a hollow drill. (b) Intraoperative navigation screen in three multiplanar reconstructions. The actual position of the drill (green) is shown in reference to the good visible lesion on the tibia shaft. An aiming device helps to drill along the planned trajectories (red) and shows the distance from the start point. [Color version available online]](/cms/asset/20507929-0430-4d3f-ad4a-7235e879f0d4/icsu_a_122969_f0007_b.jpg)
Results
Histology confirmed the diagnosis of osteoid osteoma in all cases. Two patients reported being pain-free immediately following the operation without complication. The third patient was still symptomatic after 5 weeks and it was decided to perform an additional postoperative CT scan. The CT demonstrated evidence of the drill canal in the area consistent with the former nidus of the lesion (). This finding was consistent with the intraoperative Iso-C3D® control scan (). The patient was reported to be pain-free at the seventh postoperative week without further treatment. All patients have remained symptom free at the 7-month follow-up with no evidence of recurrence.
Figure 8. A conventional postoperative CT scan done 5 weeks after surgery on the patient with the distal tibial shaft lesion. The scan is congruent with the direct intraoperative images of the Iso-C3D® control scan ().

Figure 9. Intraoperative Iso-C3D® control scan after navigated resection of the lesion at the distal tibia.
The net radiation time during the Iso-C3D®-based procedure was 40 s in every case. This included the time required for the control scan before skin closure. Results of the last 12 conventional CT-based cases revealed an average of 93 s (range 56–402 s) with the percutaneous-based approach. The average operating time with the use of navigation was noted to be slightly longer, at 78 min, when compared with that of the conventional CT-based procedures, which took an average of 60 min (range 36–140 min).
Discussion
CT-based percutaneous resection of osteoid osteomas has become a widely accepted alternative to open surgical procedures Citation[1], Citation[7], Citation[8]. Good results and high accuracy have been frequently reported with the minimally invasive approach, making it the method of choice in many institutions. Advantages are most evident with proper intraoperative visualization of the lesion in multiplanar radiologic planes. This is especially the case when it comes to operating on less accessible anatomic regions such as the vertebral bodies and the femoral neck. The exact resection of the nidus in these areas is crucial to the success of the procedure and almost always guarantees adequate relief of symptoms and the prevention of recurrences Citation[5], Citation[13]. When compared with the open approach, the overall rate of collateral complications like nerve or vessel injuries or associated fractures is lower.
In light of its success, the minimally invasive technique can still prove to be technically demanding and complications do occur Citation[1], Citation[2]. Perhaps the biggest disadvantage for the surgeon arises from the fact that the necessary operative procedure typically occurs outside the OR in the CT environment, which raises a question of sterility. Although reported infections are relatively low, rates of 5–10% have been described Citation[1], Citation[2]. The technical guidance of hollow drills associated with the conventional CT-based technique is rather demanding where the direct control and proper positioning of the surgical instruments are only possible between the control scans. This may explain the multiple reported drill failures, repeated CT scans and overall complication rates up to 24% associated with this approach Citation[1], Citation[2]. A study by Pfeiffer et al. Citation[4] reported a 34% complication rate with the minimally invasive technique.
The Iso-C3D®-based resection described earlier demonstrates the possible advantages of the navigated approach to minimally invasive surgery. Until now, CT-based navigation was quite limited in its application to minimally invasive procedures because exact anatomic matching or external referencing was necessary. Fluoroscopic-based navigation is also limited, as the visual information is two-dimensional. The use of the Iso-C3D® as an intraoperative diagnostic imaging tool has been reported in previous studies Citation[11], Citation[12], Citation[14]. The combination of the Iso-C3D® with a navigation system, especially in cases in which a high level of accuracy and three-dimensional imaging is helpful, appears to be an up-and-coming addition according to recent literature Citation[9]. Good-to-excellent results with this technique have been observed with minimally invasive approaches to pedicle screw placement and to osteochondral lesions of the talus. The biggest advantage of Iso-C3D®-based navigation is that it allows permanent multiplanar visual control of the surgical tools with a limited approach. An exact visualization of the lesion is possible and imaging quality appears to be comparable with preoperative (conventional) CT scans. Furthermore, stepwise drilling of the lesion is possible with direct control of the anatomical region without additional exposure to radiation. Misplacements involving collateral damage, especially at fracture-related areas, can be prevented. This may help to reduce or prevent the iatrogenic fractures that have been associated with both open surgical and minimally invasive CT-guided techniques Citation[2], Citation[8].
An intra-operative Iso-C3D® control scan may be done at the end of the procedure to confirm the results if necessary. The intraoperative information obtained from the Iso-C3D® was comparable with the postoperative CT study in one of the three reported cases. As the imaging software is refined, the need for postoperative scans may become debatable. The advantages of a reduction in the net radiation exposure time when compared with the CT-guided technique appear to be obvious; however, larger clinical studies comparing the two techniques would be beneficial. Although the quality of the Iso-C3D® imaging is somewhat diminished compared with conventional CT studies, the latter require multiple low-dose control scans in between drilling procedures, which only increases the total exposure to radiation for the patient. Another disadvantage of the conventional method is that disturbance by metallic artifacts may lead to quality reduction of the image. With this in mind, the general intraoperative image quality of the two modalities is fairly comparable in the majority of cases involving the extremities.
Although we observed that the CT guidance technique was more efficient in terms of total operating time, we believe that the operation time with the Iso-C3D® technique is influenced by a learning curve. Once the surgeon becomes experienced with this approach, the total amount of time needed should be equal to that for the conventional method. This approach also reduces the overall dependence on the resources of the radiology department. In conclusion, the use of Iso-C3D® in minimally invasive operating procedures offers new possibilities in the general use of navigation in orthopaedic surgery. Further clinical studies should calculate and compare both the overall costs and the effectiveness of this type of surgery. It should also be noted that one should consider the additional personnel needed for handling of both the navigation system and the Iso-C3D® system. The usage of the Iso-C3D®-based software of the navigation module is technically demanding, and the coordination of the special surgical instruments in various multiplanar reconstructions requires extra training.
References
- Buhler M., Binkert C., Exner G. U. Osteoid osteoma: technique of computed tomography-controlled percutaneous resection using standard equipment available in most orthopaedic operating rooms. Arch Orthop Trauma Surg 2001;; 121: 458–461
- Sans N., Galy-Fourcade D., Assoun J., Jarlaud T., Chiavassa H, Bonnevialle P., Railhac N., Giron J., Morera-Maupome H., Railhac J. J. Osteoid osteoma: CT-guided percutaneous resection and follow-up in 38 patients. Radiology 1999;; 212: 687–692
- Worland R. L., Ryder C. T., Johnston A. D. Recurrent osteoid-osteoma. Report of a case. J Bone Joint Surg Am 1975;; 57: 277–278
- Pfeiffer M., Sluga M., Windhager R., Dominkus M., Kotz R. Surgical treatment of osteoid osteoma of the extremities. Z Orthop Ihre Grenzgeb 2003;; 141: 345–348
- Shereff M. J., Cullivan W. T., Johnson K. A. Osteoid-osteoma of the foot. J Bone Joint Surg Am 1983;; 65: 638–641
- Rosenthal D. I., Hornicek F. J., Torriani M., Gebhardt M. C., Mankin H. J. Osteoid osteoma: percutaneous treatment with radiofrequency energy. Radiology 2003;; 229: 171–175
- Berning W., Freyschmidt J., Ostertag H. Percutaneous bone biopsy, techniques and indications. Eur Radiol 1996;; 6: 875–881
- Berning W., Freyschmidt J., Wiens J. Percutaneous therapy of osteoid osteoma. Unfallchirurg 1997;; 100: 536–540
- Wendl K., Von Recum J., Wentzensen A., Grutzner P. A. Iso-C 3D-assisted navigated implantation of pedicle screws in the thoracic and lumbar spine. Unfallchirurg 2003;; 106: 907–913
- Kendoff D., Geerling J., Mahlke L., Citak M., Kfuri M., Hüfner T., Krettek C. Navigated Iso-C 3D based drilling of an oestochondral lesion of the talus. Unfallchirurg 2003;; 106(11)963–967
- Kotsianos D., Rock C., Euler E., Wirth S., Linsenmaier U., Brandl R., Mutschler W., Pfeifer K. J. 3-D imaging with a mobile surgical image enhancement equipment (ISO-C-3D). Initial examples of fracture diagnosis of peripheral joints in comparison with spiral CT and conventional radiography. Unfallchirurg 2001;; 104: 834–838
- Rock C., Kotsianos D., Linsenmaier U., Fischer T., Brandl R., Vill F., Wirth S., Kaltschmidt R., Euler E., Pfeifer K. J., Reiser M. Studies on image quality, high contrast resolution and dose for the axial skeleton and limbs with a new, dedicated CT system (ISO-C-3D). Rofo Fortschr Geb Röntgenstr Neuen Bildgeb Verfahr 2002;; 174: 170–176
- Woertler K., Vestring T., Boettner F., Winkelmann W., Heindel W., Lindner N. Osteoid osteoma: CT-guided percutaneous radiofrequency ablation and follow-up in 47 patients. J Vasc Interv Radiol 2001;; 12: 717–722
- Rock C., Linsenmaier U., Brandl R., Kotsianos D., Wirth S., Kaltschmidt R., Euler E., Mutschler W., Pfeifer K. J. Introduction of a new mobile C-arm/CT combination equipment (ISO-C-3D). Initial results of 3-D sectional imaging. Unfallchirurg 2001;; 104: 827–833

