Abstract
Objective: The aim of this paper is to assess the accuracy of an algorithm implemented by PRAXIM™ in the SURGETICS™ navigation station for detection of the hip center. This study will assess the robustness and accuracy of the algorithm in various clinical situations such as those involving non-sphericity of the femoral head, motion of the pelvis during hip center detection, and restricted range of motion.
Materials and Methods: The localization of the hip center, based on kinematics, relies on the recording of n successive positions of the femoral rigid body in the localizer reference system during a passive circumduction motion of the hip joint. Therefore, the shape of the clouds of points acquired may vary from one acquisition to the next. To allow a comprehensive study of the consequences of these variations for hip center detection, we developed a simulator to generate numerous clouds of points. Results given subsequently for each test are the values of the difference between the femoral mechanical axis computed with Cc, the computed hip center, and the same axis computed with Co, the reference hip center.
Results: Test 1: Sensitivity to noise. The errors ranged from 3.33 E − 12 (SD 3.29E − 12) for a noise of 0 mm to 8.18E − 1 (SD − 7.05E − 1) for a noise of 15 mm. Test 2: Sensitivity to the shape of the acquisition motion. All trajectories gave an error < 1°. Test 3: Sensitivity to restricted range of motion. No value > 1° was found during this test. Test 4: Sensitivity to the distance between two points of the cloud. No value > 0.5° was found during this test. Test 5: Sensitivity to the number of points included in the cloud. No value > 1° was found during this test.
Conclusions: The Surgetics algorithm is robust to noise, can compensate for pelvic motion, and can be used even in the case of restricted range of motion.
Objective
The main issue in computer-assisted surgery of the lower limb is the definition of an accurate reference system. Therefore, rigid bodies are attached to the bones and used to express the location of several landmarks in the reference systems that they define. On the femoral side, the anatomical landmarks usually used are the center of the hip, the center of the anterior arch, the posterior condyles, the Whiteside line, or the transepicondylar axis Citation[1]. Localizing these points in the femoral reference system helps to define the frontal, sagittal, and coronal planes of the femur. Of these landmarks, the center of the femoral head is the most difficult point to localize accurately in the 3D space. Several approaches can be used to achieve this goal depending on the procedure. In CT-based systems, the center of the hip is located in the data set (on 2D slices or in the 3D volume) through a dedicated graphic user interface (GUI). In non-image-based systems, the center of the hip is localized using a kinematic approach. The aim of this paper is to assess the accuracy of an algorithm implemented by PRAXIM™ in the SURGETICS™ navigation station for detection of the hip center during TKR, THA, and osteotomies Citation[2], Citation[3]. This study will assess the robustness and accuracy of the algorithm in various clinical situations such as those involving non-sphericity of the femoral head, motion of the pelvis during hip center detection, and restricted range of motion.
Background
The localization of the hip center, based on kinematics, relies on the recording of n successive positions of the femoral rigid body in the localizer reference system during a passive circumduction motion of the hip joint. If we lived in a perfect geometrical world, then the center of the hip would be the center of the sphere, which would perfectly match the successive positions of the femoral rigid body. In this case, this point could be clearly identified in the 3D space as a unique fixed point.
However, in vivo, one must take into account the fact that one is not living in a perfect geometrical world and that
(1) The femoral head is not a perfect sphere. This anatomical structure is spheroid in normal cases and can have important deformations in the case of severe osteoarthritis or dysplasia Citation[4]. In these situations, the rotation occurs around a rotating center which moves in the 3D space.
(2) During the circumduction motion of the hip joint, there is always an associated motion of the pelvis. This associated motion will blur the hip center detection Citation[5].
(3) The error of the localizer detection is not equal to zero and must be taken into account even if previous studies have shown good accuracy in such systems Citation[6].
Therefore, the algorithm under study in this paper searches for a point in the 3D space Ch that optimizes some criteria based on the minimum of a functionwhere i is the position of the femur at time t and ci is the corresponding calculated center. The resulting point can be seen as the point in the 3D space attached to the femur with the smallest trajectory during the acquisition motion. From Equation (1), one can see that the detection of the hip center is strongly influenced by the shape of the cloud of points recorded during the circumduction motion of the hip joint. Actually, the successive locations of ci are different from one acquisition to the next depending on the shape of the motion performed by the surgeon Citation[7].
Various clinical and technical parameters can influence the shape of the cloud of points. To allow an exhaustive study of the consequences of these variations on the hip center detection, we developed a simulator to generate numerous clouds of points. The studied parameters are summarized in . The study will quantify the sensitivity of the hip center detection with respect to each of them.
Table I. Parameters that may modify the shape of the cloud of points.
Materials and methods
Description of the simulator
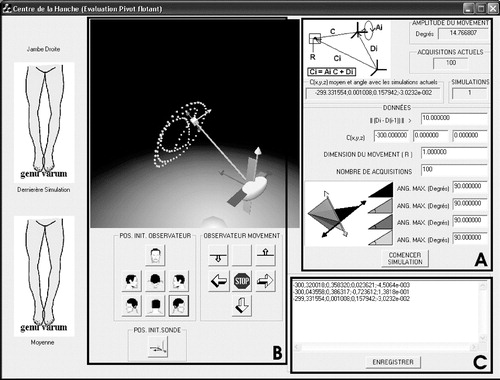
A simulator was specifically developed for this study in Visual C++TM using the VTK™ graphic library. It permits the changing of any feature of the circumduction motion and any technical parameter of the acquisition. The GUI of the simulator is presented in . One can define three areas on this GUI.
Area A: Where the parameters (clinical and technical) of the motion are defined.
Area B: Interactive generation of the clouds of points.
Area C: Results area.
Area A: Any parameters of can be set up interactively in this area.
(a) The minimal distance between two points included in the cloud—In vivo, the localizer is able to record 20 points per second. In the Surgetics algorithm, these points are filtered and the only ones used for the detection are the points with a minimal distance of 10 mm between them. The ||Di − D(i − 1)|| parameter allows study of the consequence of this filtering on the accuracy of the detection. It can be changed from 0 mm to ∞.
(b) The true position of the hip center—The purpose of the simulator is to compare the difference between a computed hip center and a perfectly known hip center. Therefore, the 3D location of this reference point can be set up interactively. For the purpose of this study, the values of C(x,y,z) have been fixed at (−300,0,0), simulating a femur of 300 mm length.
(c) Intensity of noise—The parameter R represents the intensity of the noise. This noise is the sum of the noise induced by the motion of the pelvic bone, the non-sphericity of the femoral head (due to hip dysplasia, for instance), and the inaccuracy of the localizer. As these parameters cannot be dissociated in vivo, they have been grouped under one parameter in the simulator. R can be changed from 0 mm to ∞.
(d) The number of points in the cloud—During the surgery, the acquisition motion is stopped as soon as 100 points have been recorded. In the simulator, one can stop the acquisition and compute the detection with a number of points ranging from as low as two to an infinite number.
(e) The range of motion—The key issue with a kinematic approach is: What will happen if the patient undergoing surgery has a limited range of motion? To answer this question, we defined four angular parameters: parameter 1, adduction; parameter 2, flexion; parameter 3, abduction; and parameter 4, extension. All of them can be changed from 0 to 130°.
Area B: Interactive generation of the clouds of points
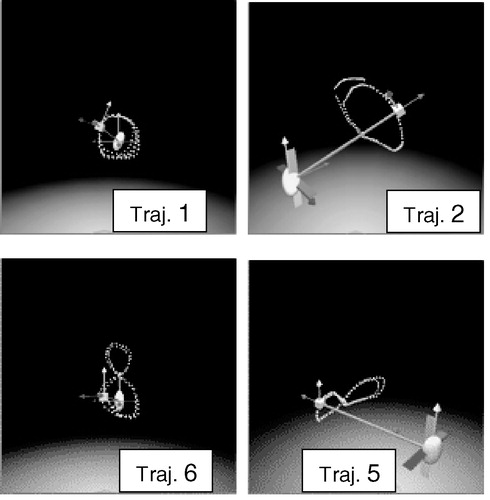
In this part of the GUI, one can interactively define the shape of the cloud of points. The restriction on the nature of the clouds fixed in area A is strictly enforced and the user is not able to go beyond these limits. shows different shapes reflecting different possible acquisition motions.
Area C: Results area
Once the cloud has been created, the 3D location of each point of the cloud is given as input data to the Surgetics algorithm. This algorithm computes Cc, the computed hip center, then the simulator compares the location of Cc to the location of the original known center Co.
The difference between Cc and Co allows the definition of two different femoral mechanical axes. The result given by the simulator is the angle between these two axes in the frontal plane.
Experimental protocol
Five experimental tests were realized in the study. We successively studied the sensitivity of the algorithm to: (1) the intensity of noise, (2) the shape of the acquisition motion, (3) the range of motion, (4) the distance between two points of the cloud, and (5) the number of points in this cloud. Except for test (3), the possible ranges of motion were fixed at: flexion 90°, extension 1°, abduction 45°, and adduction 35°. These are the usual mean values encountered with normal patients. Except for test (1), the value of the noise was fixed at 3 mm.
Test (1): Sensitivity to noise
During this test, the value of R was incremented from 0 to 16 mm in steps of 1 mm. This means that the center of the hip could move during the acquisition motion in a virtual box whose edges were of the size of R. During the whole acquisition motion, the center of the hip was only allowed to move five times in order to avoid any averaging of the error by a fully random displacement. All other parameters of the motion were kept invariant during the test. Their values can be found in .
Table II. Quantitative values of the parameters that may modify the shape of the cloud of points.
Test (2): Sensitivity to the shape of the acquisition motion
During this test, 11 trajectories producing 11 different clouds (in terms of spatial distribution of the points) were defined.
The shapes of these 11 trajectories are listed in . All other parameters were fixed and can be found in .
Table III. Definition of 11 trajectories.
Test (3): Sensitivity to restricted range of motion
To assess the sensitivity of the algorithm to the range of motion of the patient undergoing surgery, we defined six cases.
Cases 1 and 2: Flexion restricted to 60° and 30°, respectively,
Case 3: Abduction restricted to 20°,
Case 4: Adduction restricted to 15°,
Case 5: Cirmcumduction restricted to 15°/1°/45°/25° (Flex, Ext, Abd, and Add),
Case 6: Circumduction restricted to 10°/1°/10°/10° (which simulated a fused hip).
All other parameters were fixed and can be found in .
Test (4): Sensitivity to the distance between two points of the cloud
During this test, the minimum distance between two points || Di − D(i−1) || included in the cloud was incremented from 0 to 50 mm in steps of 10 mm.
All other parameters were fixed and can be found in .
Test (5): Sensitivity to the number of points included in the cloud
During this final test, the clouds given to the Surgetics algorithm as input were composed of an increasing number of points from 50 to 200.
All other parameters were fixed and can be found in .
Results
At this point, we would like to remind the reader that the results given subsequently for each test are the values of the difference between the femoral mechanical axis computed with Cc (computed hip center) and the same axis computed with Co (original hip center). These values are given in degrees and will be named under the generic term of error.
Test (1): Sensitivity to noise
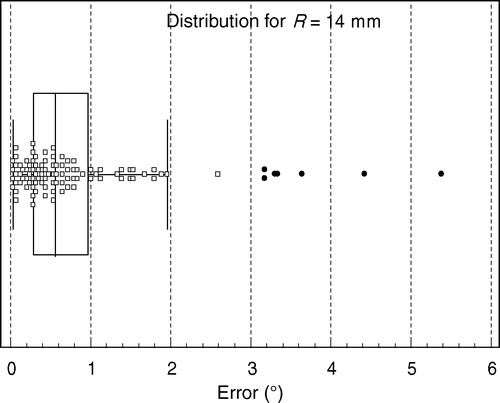
The errors ranged from 3.33E − 12 (SD 3.29E − 12) for a noise of 0 mm to 8.18E − 1 (SD − 7.05E − 1) for a noise of 15 mm. The total results of the test are summarized in .
Figure 3. Results of test 1—consequences of the error in the hip center location as a function of the intensity of noise.
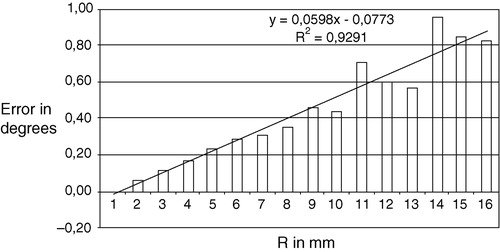
The values reported in show that as soon as R is > 5 mm one can observe errors of up to 1°. describes the 100 values obtained for R = 14 mm. One can see that 24 measurements are over 1°.
Table IV. Results of test 2 for the 11 trajectories.
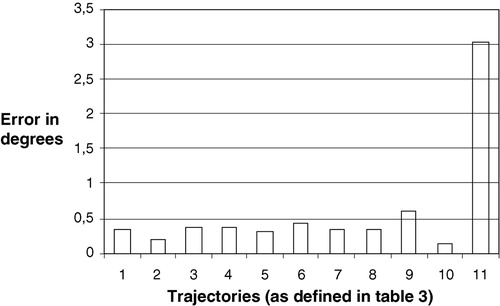
Test (2): Sensitivity to the shape of the acquisition motion
Purely vertical trajectories (number 11) give a mean error of 3°. All other trajectories give an error <1°, as described in . The exhaustive results of this test are summarized in .
Test (3): Sensitivity to restricted range of motion
No value >1° was found during this test, as reported in .
Table V. Results of test 3—consequence of the error in the hip center location with regard to the range of motion.
Test (4): Sensitivity to the distance between two points of the cloud
No value >0.5° was found during this test. The differences between the values are not statistically significant, as reported in . (Student's t-test with α = 0.05).
Table VI. Results of test 4—consequences of the error in the hip center location as a function of the minimum distance between two points in the cloud.
Test (5): Sensitivity to the number of points included in the cloud
No value >1° was found during this test, as reported in . When the number of points increases from 25 to 100 (the value used in the Surgetics platform), the error decreases from 0.86° to 0.14°. This difference is statistically significant (Student's t-test with α = 0.05). The difference between 100 and 75 points is not significant under the same statistical rules.
Table VII. Results of test 5—consequences of the error in the hip center location as a function of the number of points in the cloud.
Discussion
The detection of the hip center using a kinematic approach must rely on robust algorithms. Actually, the literature is very limited on this subject, as companies that are developing navigation software are not likely to publish their algorithms. The authors thank the French Ministry of Industry for the opportunity to have access to the source code of the algorithm implemented by Praxim and to test it under various conditions. Two different approaches can be applied to test such an algorithm: a cadaver approach and a simulator approach. The first one is more clinically oriented and closer to true surgical situations: however, it is a less comprehensive approach. In reality, it is impossible to test cadavers with restricted range of motion in flexion or in abduction or in both. It is almost impossible to reproduce multiple measurements as we did in this study with regard to the cost and time necessary to perform the testing of 9400 hip measurements. Even if it were possible in terms of time and money, who could provide the lab with the calibrated cadavers needed to test the algorithm under various and precise circumstances? For these reasons, we decided to build the simulator described earlier and to perform a study as comprehensive as possible. Over 9400 measurements were done to cover as many clinical situations as possible.
No model of hip displacement was implemented in this simulator, and this point can be discussed. From our point of view, the displacement of the center of rotation during the acquisition motion cannot be modeled. This motion is the result of the shape of the femoral head, which is strictly dependent on the specific patient. The pelvic motion is dependent on the passive motion made by the surgeon and is never the same motion twice. Therefore, trying to develop and implement a model of hip center displacement is not of interest. A random and comprehensive simulation approach is more likely to cover all clinical situations. Regarding the results described earlier, one can make some comments.
As stated in the introduction to this paper, the center of the hip is not unique. There is some laxity in the hip joint and the non-perfect spheroid shape of the femoral head is the source of displacements of the center of rotation during the acquisition motion. Therefore, test (1) was very important. During this test, we confirmed and quantified the influence of noise on the hip center detection. If there is no noise, the detection of the hip center with the Surgetics algorithm is perfect and the error is equal to zero. In the case of noise, there is a linear correlation (Pearson correlation coefficient =0.92) between the intensity of noise and the error as defined earlier. The equation of the linear regression curve is y = 0.06 × X − 0.07, which means that an intensity of noise of 18 mm is necessary to produce an error of 1°. However, one must take into account the uncertainty attached to this regression curve and be careful in the analysis of the results. In fact, as shown in , if R is equal to 14 mm, then 24% of the measurements give an error >1°. Performing redundant measurements during surgery is therefore necessary. Intra-comparison of these measurements will allow compensation for such sensitivity and improvement of the robustness of the hip center location according to the noise.
The trajectory described by the lower limb during the acquisition motion is responsible for various spatial distributions of the points. However, only purely vertical motions give poor results, with a mean error equal to 3°. Therefore, we recommend avoiding this kind of motion, as well as motions with vertical axes such as a vertical rectangle or vertical ellipse. The preferred trajectory to minimize the error is a big circle. Therefore, we recommend that the surgeon perform a passive motion of the lower limb describing a circle as big as permitted by the mobility of the hip.
As surgeons, we were interested in knowing whether patients with restricted range of motion were eligible for such surgery. Therefore, we performed test 3, which was very surprising. As reported in , even with a very restricted ability to move the hip, the mean error was 0.4°, ranging from 0.006° to 1.12°. Patients with a residual mobility as low as 10° in each sector (flexion, abduction, and adduction) are therefore eligible for this surgical approach.
The parameter assessed in test 4 is strictly technical. The localizer can digitize 20 points/s, and only points with 10 mm of distance between them are taken into account. This helps to give a better spatial distribution of the points in the cloud. We observed in this test that the accuracy always matches the clinical need. The value of 10 mm used by the Surgetics algorithm leads to a mean error of 0.14°, ranging from 0.001° to 0.6°. The statistical analysis performed shows no difference between the different distances. Therefore, the speed of the passive acquisition motion is not of interest for the surgeon and this motion can be performed at any speed without decreasing the accuracy of the detection.
One of the key issues for the future success of computer-assisted surgery is providing the surgeon with easy and fast applications. Increasing the number of points to be acquired leads to increased surgical time, which is exactly what we are not looking for. Therefore, we investigated in test 5 whether it was possible to decrease this number of points in order to minimize the surgical time. The results reported in suggest that 50 points are required. If we use only 25 points (which can help to reduce the acquisition time by a factor of 4), then the error may increase up to 3.12°. Over 75 points, there is no significant difference, and increasing the number of points further is unnecessary as it leads to a longer surgical time.
To conclude this discussion, we would like to underline the necessity of implementing algorithms that are able to take the noise into account and to compensate for pelvic motion. All other approaches are not of interest. Even with such algorithms some redundancy of the measurements and controls is recommended to avoid outliers. We would like to recommend circular acquisition motion instead of vertical motion. And finally, it is interesting to know that patients with restricted range of motion are eligible for these approaches, and that with this type of algorithm there is no longer any need for a rigid body on the iliac crest.
Acknowledgement
This work is partially supported by a grant from the French Ministry of Industry.
References
- Jenny J. Y., Boeri C. Low reproducibility of the intra-operative measurement of the transepicondylar axis during total knee replacement. Acta Scand Orthop 2004; 75(1)74–77
- Stindel E., Briard J-L, Merloz P., Plaweski S., Dubranr F., Lefevre C., Troccaz J. Bone morphing: 3D morphological data for total knee arthroplasty. Comp Aided Surg 2002; 7(3)156–168
- Gil Cano J., Stindel E., Hamitouche C., Roux C. CT less based computer assisted navigation system for high tibial osteotomy using an optical tracking system. Surgetica. Sauramps, Grenoble 2002
- Wagner S., Hofstetter W., Chiquet M., Mainil-Varlet P., Staufer E., Ganz R., Siebenrock K. A. Early osteoarthritic changes of human femoral head cartilage subsequent to femoro-acetabular impingement. Osteoarthritis Cartilage 2003; 11(7)508–526
- DiGioia A. M., Plakseychuk A. Y., Jaramaz B. Mini-incision techniques and navigation for total hip. Navigation and Robotics in Total Joint and Spine Surgery, J. B. Stiehl, W. H. Konermann, R. G. Haaker. Springer;, Berlin 2003; 61–69
- Schmerber S., Chassat F. Accuracy evaluation of a CAS system: laboratory protocol and results with 6D localizers, and clinical experiences on otorhinolaryngology. Comp Aided Surg 2001; 6(1)1–13
- Stindel E., Gyl D., Briard J. L., Merloz P., Dubrana F., Lefevre C. Detection of the center of the hip in CT less based system for TKA navigational guidance. An evaluation study of the accuracy and reproducibility of the surgetic's algorithm. CAOS International Symposium., Santa Fe, NM, June 2002