Abstract
Using a total of 30 cadaveric hips, the accuracy of a fluoroscopy-based computer navigation system for cup placement in total hip arthroplasty (THA) was investigated and an error analysis was carried out. The accuracy of placing the acetabular component within a predefined safe zone using computer guidance was compared to the precision that could be achieved with a freehand approach. Accurate control measurements of the implanted cup were obtained using fiducial-based matching to a pre-operative CT scan with respect to the anterior pelvic plane. A significantly higher number of cups were placed in the safe zone with the help of the navigation system. The variability of cup placement could be reduced for cup abduction but not substantially for cup version. An error analysis of inaccurate landmark reconstruction revealed that the registration of the mid-pubic point with fluoroscopy was a potential source of error. Keeping this pitfall in mind, fluoroscopy-based navigation in THA is a useful tool for registration of the pelvic coordinate system, particularly those points that cannot be reached by direct pointer digitization with the patient in the lateral decubitus position.
Introduction
Proper component positioning in total hip arthroplasty (THA) is essential to prevent complications and achieve satisfactory long-term results. The acetabular component is particularly prone to malpositioning, which is correlated with a significantly increased risk of prosthetic impingement dislocation Citation[1], early revision surgery for cup reorientation Citation[2], increased wear Citation[3], and increased aseptic loosening rates. Although there is no uniform guideline concerning optimal cup orientation and there may be a need for individual adjustment, there is general agreement about the ‘safe range’: accurate placement of the cup within 40 ± 10° of cup abduction and 15 ± 10° of version decreases the risk of dislocation by 25% Citation[1]. Despite the availability of numerous mechanical positioning guides and ample surgeon experience, up to 75% of conventionally implanted cups are positioned outside these secure limits Citation[4–6].
Recently, computer-assisted methods have been introduced for intra-operative navigation to improve the precision of acetabular cup placement in THA. These can be categorized in three modalities. CT-based modules require time-consuming pre-operative planning and complex intra-operative matching procedures that are subject to a considerable learning curve. Moreover, they are usually associated with increased costs and radiation. Completely image-free techniques refer their angular feedback to percutaneously digitized anatomical landmarks, which can be difficult to obtain, particularly in patients that are obese or in the lateral decubitus position Citation[7]. Virtual fluoroscopy could provide both visual and angular feedback without pre-operative planning, as proved for other applications Citation[8].
Therefore, the accuracy of a fluoroscopy-based navigation system for acetabular cup positioning was evaluated in a cadaver setup and potential pitfalls of this method were analyzed. It was hypothesized that such a hip navigation system improves the probability of implanting the cup within the safe range and reduces the variability of cup orientation in comparison to freehand positioning by the surgeon.
Materials and methods
Fourteen cadaveric hips (from seven specimens: four male, three female) were included in the first part of the study. Cadavers were prepared with a special saline-based fixation technique Citation[9] to keep the soft tissues and joint mobile and as natural as possible. Prior to surgery, to ensure high accuracy of registration post-operatively, six custom-made fiducial marker screws were inserted into the pelvic ring: one on each iliac crest, one in each inferior iliac spine, and one on each superior pubic ramus. These screws were made of titanium and had a spherical head to minimize metal artifacts and give a well-defined signal in the subsequent CT scan. A standard pelvic CT scan with a slice distance of 2 mm and thickness of 3 mm was obtained for each cadaver. The data were loaded into a CT-based navigation system (SurgiGATE®; Praxim-Medivision AG, Bern, Switzerland) for image-guided cup placement Citation[10] and used to create an individual 3D model. The following three landmarks defining the anterior pelvic plane (APP) were identified in the CT by the surgeon (KAS) and used to establish the unambiguous pelvic reference coordinate system Citation[11]: both anterior superior iliac spines and the mid-point between the pubic tubercles.
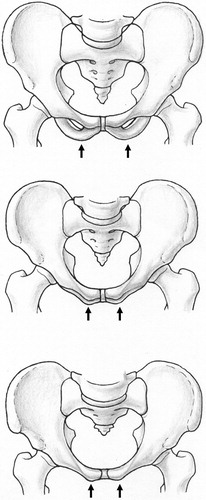
Prior to surgery, the cadaver was placed in a supine position. A dynamic reference base (DRB) that accounts for possible movement between the pelvis and the operating table was attached to the upper pelvic crest through a small skin incision. Using a tracked fluoroscope (Siremobil Iso-C, Siemens Medical Solutions, Erlangen, Germany), two images were acquired of each of the osseous landmarks of the APP ( and ). Each landmark to be reconstructed was then marked in the two corresponding fluoroscopic images and its 3D location was calculated by a back-projection algorithm Citation[12]. To ensure the reported accuracy of 1 mm Citation[13], a minimum spatial angle of 50° is necessary between the two fluoroscopic images.
Figure 1. Inlet and outlet views of the pelvis were used to define the mid-pubic point. The inlet view is characterized by overlying superior and inferior pubic rami.
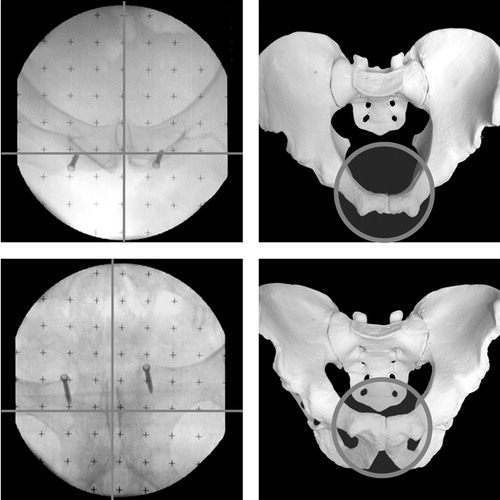
Figure 2. The two fluoroscopic views used to define the anterior superior iliac spines. A frontal view allows definition of the midpoint between the visceral and parietal compacta. A lateral view reveals the most prominent point of the spine.
Once all the reference points were defined, the image intensifier was removed. The cadaver was then repositioned in a lateral decubitus position and the surgical procedure was performed using a transgluteal approach. Exposure of the hip joint and resection of the femoral head were done in a standard manner. Reaming of the acetabulum and cup implantation were carried out with navigational feedback enabled. In an initial step, the surgeon was blinded to the computer screen and oriented the cup according to his intra-operative experience and visual judgment. The goal was to place the cup within the safe range of 15 ± 10° of radiographic Citation[14] version and 40 ± 10° of radiographic abduction Citation[1]. The angles representing the orientation that was deemed optimal by the surgeon were recorded by the navigation system. In a second step, the cup was finally placed under interactive real-time guidance by the computer, aiming at 40° of cup abduction and 15° of cup version. The time required for the additional fluoroscopy-based registration was recorded. Subsequently, the CT-based software was started and paired-points matching was performed using the fiducial marker screws. The fiducial-based matching has a reported accuracy of 1.3 mm Citation[15]. The orientation of the cup was recorded with a sharp pointer digitizing four pre-operatively drilled marker holes representing the opening plane of the hemispherical cup. Cup orientation was expressed relative to the pre-operatively defined CT-based reference, which was considered to be the gold standard. Successful placement of the cup within the safe zone was verified for both the freehand and navigated cup orientations. The accuracy of fluoroscopy-based reference-point reconstruction was calculated in terms of the Euclidean distance of the points from the corresponding locations defined in the CT.
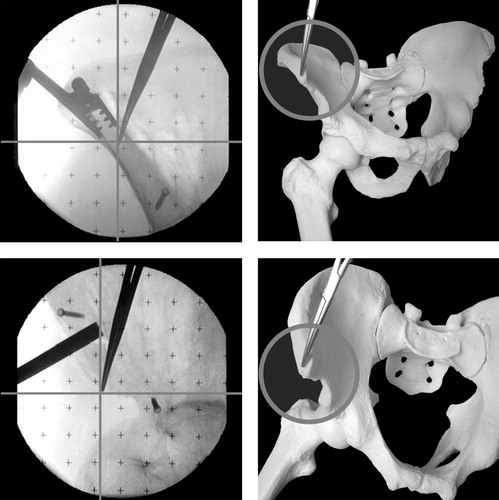
The second part of the study analyzed the influence of inaccurate landmark definition on the calculation of cup abduction and version. Sixteen dry cadaveric hips (eight specimens: four male, four female) were investigated. Using a spirit level, the APP of each pelvic specimen was aligned horizontal to the operating table and fixed in place with a vacuum mattress to simulate a more or less physiological pelvic position. The mid-pubic point was marked with a metal sphere. Following the procedure of the first cadaver series, two standardized fluoroscopic projections were used to define the pubic reference: (1) an outlet view with the tip of the coccyx pointing to the superior symphyseal border; and (2) an inlet view with overlapping inferior and superior pubic rami. The anterior superior iliac spines were digitized directly with a tracked pointer. A tracked cup impactor was then oriented with 40° of cup abduction and 15° of cup version and fixed rigidly to the operating table (). Defined variations of the ideal landmark definitions were investigated, and their effects on the calculated angulation of the impactor were displayed by the navigation system. For the superior iliac spines, these variations included points along the four edges forming the trapezoid shape of the ipsilateral and contralateral spine (points 1–8). For the pubic symphysis, three points at the cranial–caudal and anteroposterior extension of the symphyseal gap, as well as their mid-points, were chosen (points 9–14) as variations.
Figure 3. The setup for the error analysis is shown. The cadaveric pelvis is fixed on a vacuum mattress with the APP in horizontal orientation. A tracked cup impactor is rigidly fixed to the table in a position of 15° of version and 40° of cup abduction relative to the APP. Different predefined scenarios for maldefinition of the iliac spines and the mid-pubic point were rehearsed, and the resulting cup orientation angles were displayed by the navigation system.

Statistical analysis
Differences between freehand and computer-assisted placement of the cups within the safe range were analyzed using the McNemar test. Differences in standard deviation for abduction and version between the surgeon and navigation system were calculated with the F-test. Comparison of the Euclidean distances of the three pelvic reference points was done with the Mann–Whitney U-test. The significance level was set at a probability of less than 0.05.
Results
One hip had to be excluded from part 1 of this study due to a shift of the DRB during repositioning of the pelvis, leaving 13 hips for the evaluation of the system.
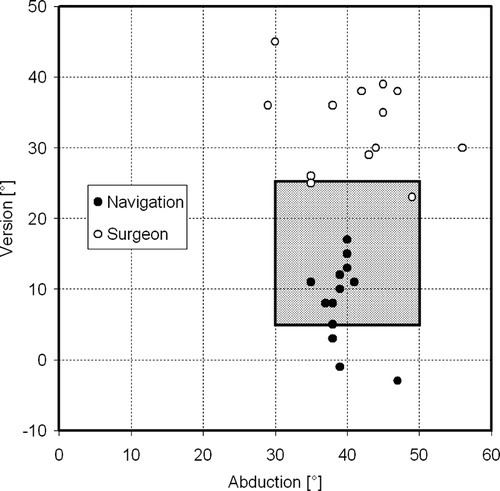
The surgeon placed significantly fewer cups (2 of 13, 15.3%) within the safe zone when compared with the navigation system (10 of 13 cups, 76.9%, p = 0.019) (). The mean cup abduction achieved by the surgeon was 41.4 ± 7.7° (range: 29–56°), whereas the mean cup abduction with the navigation system was 39.3 ± 2.8° (range: 35–47°). The mean freehand cup version was 33.3 ± 6.4° (range: 23–45°), whereas the mean navigated cup version was 8.4 ± 6.0° (range:−3 to 17°). The variability of cup placement could thus be reduced significantly for cup abduction (p = 0.001) but not for cup version (p = 0.79).
Figure 4. With the help of the fluoroscopy-based navigation system, a significantly higher number of cups were placed within the safe zone of 15 ± 10° of version and 40 ± 10° of abduction.
The mean additional time for intra-operative fluoroscopy-based registration was 14.1 ± 3.8 min (range: 9–22 min). There was no relevant learning curve apparent.
The spinae could be reconstructed using the image intensifier with a higher accuracy than the pubis point (p = 0.003) (). The mean spatial distance from the intra-operatively reconstructed point to the real CT-based landmark was 8.2 ± 3.8 mm (range: 3.2–16.6 mm) for the ipsilateral iliac spine, 8.9 ± 6.3 mm (range: 1.4–23.6 mm) for the contralateral spine, and 14.1 ± 5.5 mm (range: 4.1–26.5 mm) for the pubis. The distances of the two sets of spine points did not differ (p = 0.95).
Figure 5. The anterior superior iliac spines could be registered with greater accuracy than the midpoint between the pubic tubercles.
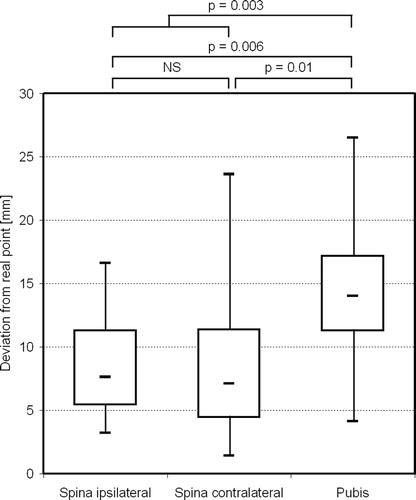
All three navigated cups placed outside the safe range failed for cup version (). A significantly higher reconstruction error was found for the corresponding pubis points in comparison to the group within the safe range (p = 0.04). All three pubis points were defined anterocranially from the real intertubercle point. In this group of malpositioned cups, no significant reconstruction error was found for either the ipsilateral (0.30) or contralateral (p = 0.23) superior iliac spine, as compared with the correctly placed cups.
The influence of inaccurate definition of the iliac spines on cup angle is negligible ( and ). None of the instances of inaccurate landmark reconstruction led to a mean abduction of the cup outside the safe range. A maximal deviation of 4° for cup abduction was found for all the defined points (point 14).
Figure 6. The influence of malregistration of the pelvic reference coordinate system is shown. The white spots represent the real bony landmarks (the anterior superior iliac spines and the pubic tubercles) of the APP. The resulting mean angle of a maldefined point is shown in the scatter diagrams, e.g., defining the pubis point too posteriorly (point 9) would lead to a more anteverted cup.
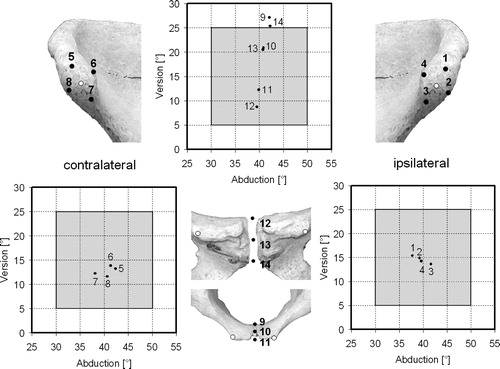
Table I. Resulting cup abduction and version angles with low landmark definition (starting orientation: 40° abduction, 15° version).
Inaccurate definition of the pubis point particularly affected cup version (). Cup version decreases when the pubis point is defined anteriocranially from the real intertubercle point (points 11 and 12), and increases when the pubis point is defined posteriocaudally (points 9 and 14). For two of these points (9 and 14), the mean version was outside the safe zone, whereas the maximal deviation for cup version was 17° for these same points.
Discussion
Different computer-assisted navigation systems have been developed to improve the accuracy of cup placement in THA. Fluoroscopy-based navigation can provide contact-less intra-operative landmark registration without the need for pre-operative planning and intra-operative matching, even for landmarks that cannot be reached with digitizing probes intra-operatively. This is the first study combining an accuracy evaluation with an error analysis of pure fluoroscopy-based surgical landmark reconstruction. With the help of the computer-assisted system, a significantly higher percentage of cups were placed within a pre-operatively defined safe range than when using freehand positioning.
In THA, incorrect cup version is the key factor leading to dislocation Citation[16], Citation[17]. Version is more difficult to judge intra-operatively, particularly in the lateral decubitus position Citation[18]. However, the navigation system could only substantially reduce variability in cup abduction, as compared with the surgeon's freehand performance. We showed that the accuracy in terms of cup version strongly depends on the accurate definition of the pubis point. Although the two images used to define the mid-pubis point were standardized (outlet and inlet views of the pelvis), this technique involves a certain risk. The overlying inferior pubic ramus can be misidentified as the pubic tubercle and subsequently lead to a more anteriorly defined pubis point, resulting in decreased cup version (). A correct superposition of both rami is not always possible: in an obese patient, for example, contact between the voluminous abdomen and the fluoroscope can impede a correct projection angle. In such situations, a different matching method might be more accurate. Keeping this source of inaccuracy in mind, cup version variation can potentially be further reduced, but this will have to be proven in future experiments.
Figure 7. The inferior pubic ramus can simulate the pubic tubercle if the superior and inferior pubic rami are not correctly overlaid.
There are reports in the literature showing that simple mechanical inclinometers can also reduce the variability of cup placement in terms of abduction Citation[19]. However, to the authors’ knowledge, there is no published anatomical-based study proving that mechanical guides can significantly reduce the variability of cup version in a manner comparable to a computer navigation system.
In the present study, the experienced hip surgeon constantly placed the cups in a more anteverted orientation, but the ranges of version did not differ markedly for the surgeon's freehand positioning and the computer navigation system. One reason for this might be that experienced surgeons place cups more reproducibly than their less-trained colleagues Citation[20]. The consistent error is a well-known finding Citation[20], Citation[21] which could be corrected for considerably by intra-operative visual and angular feedback from a computer navigation system Citation[21].
A number of accuracy studies have been performed on computer-assisted cup placement that are characterized by their heterogeneity in terms of post-operative control measurements and presentation of results (). In general, cup abduction can be measured reliably on an anteroposterior pelvic radiograph by taking anatomical reference lines into account, e.g., the ischial tuberosity or the interteardrop line Citation[21]. In contrast, cup version measurements on pelvic radiographs are inaccurate, mainly due to individual variations in pelvic tilt leading to different apparent positions of the cup Citation[11]. Therefore, control measurements of cup version must refer to the APP, e.g., by means of post-operative CT measurements or intra-operative digitizing techniques. Taking these limitations of post-operative measurements into account, our results match well with the findings of previous studies. However, owing to the lack of a uniform standard for post-operative cup measurements, an objective comparison to some of the studies is difficult.
Table II. Reported accuracies of different navigation systems for THA.
An important goal in navigated THA is the prevention of outliers. Although no significant outliers were found in this small series, larger clinical studies with anatomically based control measurements, particularly of anteversion, are necessary.
The present study demonstrates that fluoroscopy-based computer-assisted THA can improve the accuracy and reduce the variability of cup placement using carefully defined reference points. The registration of the mid-pubic point is crucial for accurate determination of cup version Citation[31] and is not always possible in obese patients. Misidentification of this point with the inferior pubis ramus on a pelvic inlet view can compromise the accuracy of the results. Definition of the iliac spines can easily be achieved in an accurate manner and can potentially be used with hybrid registration methods in the lateral decubitus position, where direct digitization with a pointer cannot be performed.
Acknowledgments
This study was funded by a grant from the Synos-Foundation for the Advancement of Orthopaedic Surgery.
References
- Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip replacement arthroplasties. J Bone Joint Surg 1978; 60A: 217–220
- Mahoney CR, Pellicci PM. Complications in primary total hip arthroplasty: avoidance and management of dislocations. Instr Course Lect 2003; 52: 247–255
- Patil S, Bergula A, Chen PC, Colwell CW, Jr., D'Lima DD. Polyethylene wear and acetabular component orientation. J Bone Joint Surg 2003; 85A(Suppl. 4)56–63
- Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grützner PA, Steffen R, Von Knoch M, Holland-Letz T, Bernsmann K. Cup placement in hip replacement surgery: a comparison of free-hand and computer assisted cup placement in total hip arthroplasty — a multi-center study. Z Orthop Ihre Grenzgeb 2004; 142: 286–291
- Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grützner PA, Steffen R, Von Knoch M, Holland-Letz T, Bernsmann K. The accuracy of free-hand cup positioning—a CT-based measurement of cup placement in 105 total hip arthroplasties. Int Orthop 2004; 28: 198–201
- Hassan DM, Johnston GH, Dust WN, Watson G, Dolovich AT. Accuracy of intra-operative assessment of acetabular prosthesis placement. J Arthroplasty 1998; 13: 80–84
- Nogler M, Kessler O, Prassl A, Donnelly B, Streicher R, Sledge JB, Krismer M. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin Orthop Rel Res 2004; 426: 159–163
- Foley T, Simon DA, Rampersaud YR. Virtual fluoroscopy: computer-assisted fluoroscopic navigation. Spine 2001; 26: 347–351
- Thiel W. The preservation of the whole corpse with natural color. Anat Anz 2001; 174: 185–195
- Langlotz U, Lawrence J, Hu W, Langlotz F, Nolte LP. Image guided cup placement. Computer Assisted Radiology and Surgery (CARS '99), HU Lemke, MW Vannier, K Inamura, AG Farman. Amsterdam, Elsevier 1999; 717–721
- Tannast M, Langlotz U, Siebenrock KA, Wiese M, Bernsmann K, Langlotz F. Anatomic referencing of cup orientation in total hip arthroplasty. Clin Orthop 2005; 426: 144–150
- Hofstetter R, Slomczykowski M, Sati M, Nolte LP. Fluoroscopy as an imaging means for computer-assisted surgical navigation. Comput Aided Surg 1999; 4: 65–76
- Schep NW, Van Walsum T, De Graaf JS, Broeders IA, Van der Werken C. Validation of fluoroscopy-based navigation in the hip region: What you see is what you get?. Comput Aided Surg 2002; 7: 279–283
- Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg 1993; 75B: 228–232
- Schlaier J, Warnat J, Brawanski A. Registration accuracy and practicability of laser-directed surface matching. Comput Aided Surg 2002; 7: 284–290
- Nishii T, Sugano N, Miki Hidenobu, Koyama T, Takao M, Yoshikawa H. Influence of component positions on dislocation. J Arthroplasty 2004; 19: 162–166
- Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty. J Arthroplasty 2002; 17: 282–288
- Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg 1982; 64A: 1295–1306
- Vendittoli PA, Duval N, Stitson DJ, Masse B. Vertical acetabular positioning with an inclinometer in total hip arthroplasty. J Arthroplasty 2002; 17: 936–941
- Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop 2004; 426: 174–179
- Leenders T, Vandevelde D, Mahieu G, Nuyts R. Reduction in variability of acetabular cup abduction using computer assisted surgery: a prospective and randomized study. Comput Aided Surg 2002; 7: 99–106
- Murphy SB. Alumina ceramic-ceramic total hip arthroplasty using computer assisted surgical navigation and a new minimally invasive technique. Bioceramics in Joint Arthroplasty, JY Lazennec, M Dietrich. Steinkopff, Darmstadt 2004; 61–69
- Haaker R, Tiedjen K, Rubenthaler F, Stockheim M. Computer-assisted navigated cup placement in primary and secondary dysplastic hips. Z Orthop Ihre Grenzgeb 2003; 141: 105–111
- Hube R, Birke A, Hein W, Klima S. CT-based and fluoroscopy-based navigation for cup implantation in total hip arthroplasty (THA). Surg Technol Int 2003; 11: 275–280
- Ito M, Tokunaga K, Kitahara H, Ito T, Endo E, Takano R, Endo N. CT-based evaluation of the 3-dimensional cup position after navigation-assisted THA. Proceeding of the 4th Annual Meeting of CAOS-International, Chicago, IL, June, 2004, F Langlotz, BL Davies, SD Stulberg. 317–318, Computer Assisted Orthopaedic Surgery
- Leenders T, Vandevelde D, Mahieu G, Nuyts R. Reduction in variability of acetabular cup abduction using computer assisted surgery: a prospective and randomized study. Comput Aided Surg 2002; 7: 99–106
- Murphy SB. Experience with fluoroscopic and CT-based navigation for total hip arthroplasty. Presentation at the Annual Meeting of the European Hip Society, InnsbruckAustria, June, 2004
- Grützner PA, Zheng G, Langlotz U, von Recum J, Nolte LP, Wentzensen A, Widmer KH, Wendl K. C-arm based navigation in total hip arthroplasty—background and clinical experience. Injury 2004; 35(Suppl. 1)S-A90–S-A95
- Mattes T, Puhl W (2003) Free navigation for total hip replacement (THR)—method and first clinical results of a new image free system. Proceedings of the 3rd Annual Meeting of CAOS-International, MarbellaSpain, June, 2003, F Langlotz, BL Davies, A Bauer. Darmstadt, Steinkopff, 228–229, Computer Assisted Orthopaedic Surgery
- Amiot LP, Dorr L, Babisch J, Yun A, Fontaine I, Odermatt D, Lanigan M, Jansen H. Clinical evaluation of a CT-free total hip application. Proceedings of 4th Annual Meeting of CAOS-International, Chicago, IL, June, 2004, F Langlotz, BL Davies, SD Stulberg. 157–158, Computer Assisted Orthopaedic Surgery
- Makhsous M, Lin A, Hendrix R, Nam D, MacDonald M, Wixson R. Anatomical landmarking identification in THA and effects on component alignment. Transactions of the 51st Annual Meeting of the Orthopaedic Research Society, Washington, DC, February, 2005, Poster no. 0313