Abstract
Computer-Assisted Orthopaedic Surgery (CAOS) has made much progress over the last 10 years. Navigation systems have been recognized as important tools that help surgeons, and various such systems have been developed. A disadvantage of these systems is that they use non-standard formalisms and techniques. As a result, there are no standard concepts for implant and tool management or data formats to store information for use in 3D planning and navigation. We addressed these limitations and developed a practical and generic solution that offers benefits for surgeons, implant manufacturers, and CAS application developers. We developed a virtual implant database containing geometrical as well as calibration information for orthopedic implants and instruments, with a focus on trauma. This database has been successfully tested for various applications in the client/server mode.
The implant information is not static, however, because manufacturers periodically revise their implants, resulting in the deletion of some implants and the introduction of new ones. Tracking these continuous changes and keeping CAS systems up to date is a tedious task if done manually. This leads to additional costs for system development, and some errors are inevitably generated due to the huge amount of information that has to be processed.
To ease management with respect to implant life cycle, we developed a tool to assist end-users (surgeons, hospitals, CAS system providers, and implant manufacturers) in managing their implants. Our system can be used for pre-operative planning and intra-operative navigation, and also for any surgical simulation involving orthopedic implants. Currently, this tool allows addition of new implants, modification of existing ones, deletion of obsolete implants, export of a given implant, and also creation of backups.
Our implant management system has been successfully tested in the laboratory with very promising results. It makes it possible to fill the current gap that exists between the CAS system and implant manufacturers, hospitals, and surgeons.
Introduction
A wide variety of different plates, screws, and nails are used in trauma surgery Citation[1]. However, scaled visualization and tracking of these devices and their corresponding surgical instruments is currently only possible using fluoroscopy Citation[2–5], which requires radiation exposure for the patient and the surgical team. Current CAS systems often simplify the shapes of implants or instruments, but it is likely that more realistic rendering and additional navigation information will improve the functionality of navigation systems Citation[6].
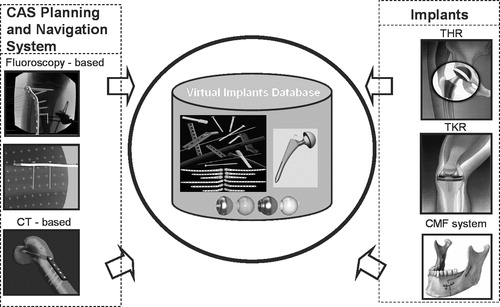
A novel concept has been developed to provide this functionality. The concept centers around a virtual implant database Citation[7] that contains both geometric and calibration information for trauma implants and instruments. This should enable realistic navigation of various implants through a common interface Citation[8], and could be used with any navigation application.
A database has been established containing various virtual representations of osteosynthesis implants and anchoring devices for fracture reduction and fixation, as well as images of various prostheses for total joint replacement (knee and hip). This database can be browsed for details of any stored virtual implant. In its current implementation, the provided interface supports the planning and navigation parameters of LISS and LC-DCP plates (Synthes, Westchester, PA, USA), as well as searching functionalities (allowing search by implant size, manufacturer, bone part, or implant type). The system has been successfully tested for several computer-assisted orthopedic surgery applications Citation[7], Citation[9]. The aim was to evaluate integration issues, network access, speed, and usability. The implant information is not static, however, because manufacturers periodically revise their implants, resulting in the deletion of some implants and the introduction of new ones. Tracking these continuous changes and keeping CAS systems up to date is a tedious task if done manually. This leads to additional costs for system development, and some errors are inevitably generated due to the huge amount of information that has to be processed.
To overcome these limitations and improve the current implant management process in CAS, we designed and developed, on top of our existing Virtual Implant Database, a graphical administration tool which aims to help surgeons, implant manufacturers, and CAS system providers easily administer the implant database. With respect to confidentiality and security issues required for medical data, the tool has been designed with additional security mechanisms and ergonomic considerations. Moreover, no database or Structured Query Language (SQL) knowledge is needed by the end-users. Our initial laboratory tests yielded successful results, and improvements are planned, along with more exhaustive tests involving surgeons, manufacturers, and CAS system providers.
Related work
To our knowledge, there has been no research on providing a virtual implant database as a global and generic rapid application development (RAD) framework. Most of the existing CAS systems are based on proprietary file-based solutions for implant management Citation[10]. Little work has been published dealing with implant selection tools or proprietary implant databases.
Jaramaz and DiGioia Citation[11], in the context of total hip replacement (THR), proposed techniques for choosing the correct implant size. They also showed that correct implant positioning and alignment remains one of the main challenges in orthopedic surgery. Taylor et al. Citation[12] presented the ROBODOC system (Integrated Surgical Systems, Davis, CA, USA) for performing THR. With this device, the surgeon plans the surgery from patient-specific pre-operative data to determine which implant design and size to use and the desired placement of the implant relative to the patient's anatomy. Bächler et al. Citation[13] have presented a system for computer-aided biological fracture plate fixation using minimally invasive surgical techniques. It was proposed to extend this system using a fracture plate database from different manufacturers and for different surgical procedures. In addition, several groups have proposed techniques for finding the best implant based on virtual fluoroscopy. Citation[2], Citation[6],Citation[14–18].
Wu et al. Citation[19] concluded that a CAS procedure usually involves different information from different sources. Therefore, the integration of a CAS, Computer Aided Design (CAD), and Computer Aided Manufacture (CAM) interface enables optimization of pre-operative planning, taking into consideration not only medical but also technical boundary conditions.
The major weaknesses of these systems are data exchange problems, the lack of a standardized implant storage format, security issues (file corruption, simultaneous access problems), and the lack of real-time sharing of implant data. Our graphically based administration tool for implant management and the concept of using XML to standardize orthopedic implants using a database is a novel concept in CAS.
Materials and methods
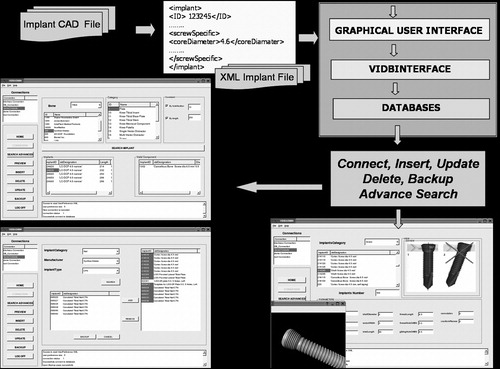
The work presented here is part of the CARIM (Computer Assisted Reduction and Imaging) project Citation[20]. The aim was to establish a virtual implant database containing geometrical as well as calibration information for orthopedic implants and instruments. This should allow different surgical navigation applications to navigate any number of different types of implants from this database ().
Figure 1. Virtual implant database: system overview. Various implant types and CAS systems are supported. (color version available online)
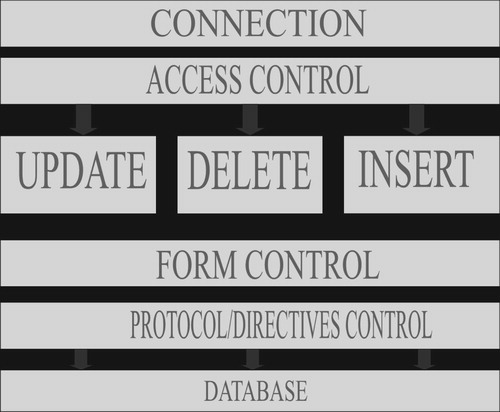
We constrained our method to respect data exchange standard and development formalisms. We then used the Unified Modeling Language (UML) Citation[21] to capture and describe our implant domain specification. We used Qt (Trolltech, Oslo, Norway) Citation[22] for our graphical user interface (GUI) development and Coin3D (Systems in Motion, Oslo, Norway) Citation[23] for the 3D object manipulation. MySql (MySQL AB, Uppsala, Sweden) Citation[24] and Caché database (InterSystems, Cambridge, USA) Citation[25] were used for storage. Our customized Implant XML engine was built on top of the Qt Document Object Model (DOM) library Citation[22]. To achieve the goals mentioned above, we adopted the following methodology ().
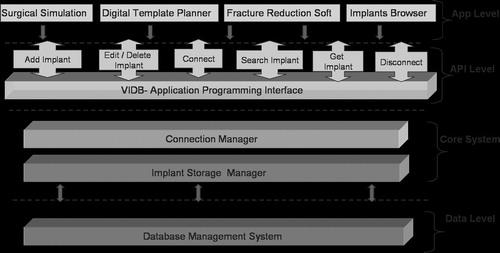
Virtual implant database design. All implants are stored in a database containing tables and their relationships, which handle implant planning and navigation parameters and also various virtual representations of osteosynthesis implants and anchoring devices.
Unified Implant Access Interface. An application programming interface (API) is provided between the database and the client applications and acts as a communication channel Citation[8]. This layer provides main functionalities to connect to the database, search implants, preview implant parameters (including 2D images and 3D models), and insert–, update–, delete and backup implants.
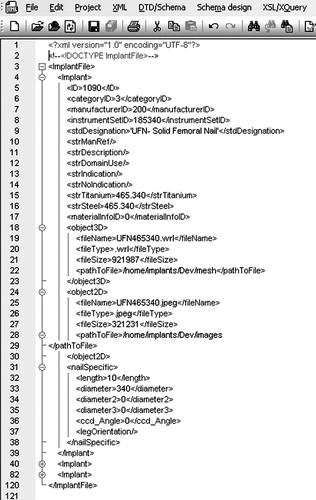
Implant XML file structure. A well-defined CAS-compliant XML implant file is generated from the implant CAD files. The first part of the XML file describes the general parameters common to all implants, whereas the second part describes the specific parameters for that implant type.
Customized implant XML engine. A custom XML engine (XMLImplantReader and XMLImplantWriter) has been developed and helps in loading XML files in the database or exporting implants from the database to a given XML file.
Graphical user interface. An advanced GUI allows the end-users (CAS system providers, hospital, and manufacturers) to manage implants. Our system workflow is organized in three stages: first, the user carries out actions while clicking buttons in the interface. These actions are reformulated in SQL requests in the interface layer. The requests are then sent to the database server, which treats them and returns the results of the requests. Each step will be described in more detail in the following sections.
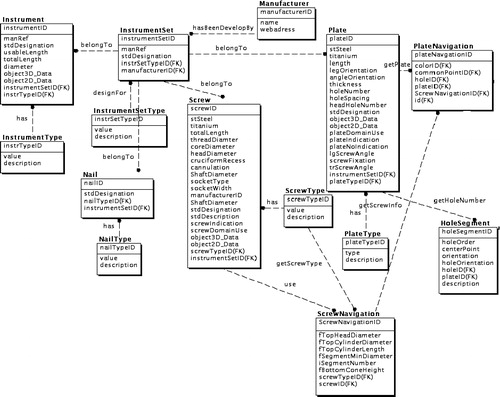
Virtual implant database design
We used the entity–relationship principle Citation[26] (the core principle of relational database systems) to design the tables and relationships that describe our orthopedic implant domain. We first designed the implant category table which handles the various implant categories routinely used by surgeons during orthopedic operations: plates, screws, and nails for trauma surgery; hip and knee components for prosthetic operations.
Each implant table is organized in two parts: the first part contains fields describing the generic parameters common to all implants (e.g., the implant name, description, manufacturer, etc.), whereas the second part describes specific parameters with respect to implant category (). The novelty of our concept is that we created generic objects to handle various implant types. The information required to add implants to our database depends on the implant category and type (e.g., plate, screw, nail, etc.).
The implant manufacturers provided us with the following:
Implant geometry (3D model, shape description, and principal dimensions);
Reference points used for navigation:
○ For implants where holes are important (e.g., plates), we used information such as the center, axis, and orientation of each hole;
○ For spherical implants with a center (e.g., hip cups), we used the geometrical center and geometrical axis;
○ For implants with an alignment plane (e.g., hip stems), we used points defining the alignment plane or alignment axis.
System interface design and implementation
Our implant database system is composed of three main parts: the implant data storage component, the core processing component, and the published interface (). The storage component handles the structure, relationships, and rules between implants (e.g., which plate can be used with which screw). The implementation has been done on top of a well-known database management system (MySQL database system and Caché system). The core processing component manages network, data processing, and security issues. The published interface will allow any CAS application to access implants easily. It acts as a communication channel between the implant database and the CAS applications or end-users. Two actions are necessary to access implants: connection with a valid login and search for the best-fitting implant or insert/update/delete if administration rights have been granted.
XML implant file design
Three-dimensional CAD files do not provide a structured, easy-to-process, and interchangeable standard that can be handled by CAS developers (for implant planning and navigation) without a tedious and manual conversion process. To overcome this problem, we chose to use Virtual Reality Modeling Language (VRML) for 3D implant mesh representation and Autocad DXF format for 2D engineering drawings. To ease inter-operability between CAS systems and to allow exchange of data and expertise among the medical research community, we designed a structured XML implant file with reference to several viewing modalities (2D image, 3D model, etc.). This XML file is currently generated based on information received from implant manufacturers and is dependent on implant type ().
We used specific tools such as VoloView (Autodesk, San Rafael, CA, USA) to extract the relevant planning and navigation information and to provide this as input to our developed tool. XML implant files are then generated and inserted in our database.
Customized implant XML engine
To transfer implant data from XML files to a database, we need to map the XML document schema (DTD, XML Schemas, etc.) to the database schema. The data transfer software is then built on top of this mapping Citation[27]. We first parse and check the validity (syntax checking and well-formed validity) of the given XML implants files using our customized implant reader engine. XMLImplantReader opens XML files and builds in memory the corresponding document tree. The output of our XML reader is a collection of implant objects with their attributes that can be manipulated to insert data in the database.
We also developed a writer component, XML ImplantWriter, which reads data from the database, builds in memory the corresponding implant object, and generates an implant file according to the implant category and type.
GUI for implant management
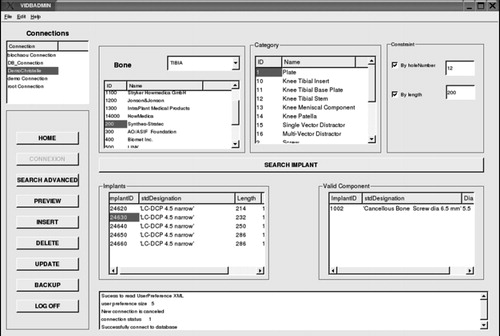
One of the main advantages of our system is that the end-users do not need to know about the underlying design and implementation techniques. SQL knowledge is not required either: users can easily manage their implants without typing SQL requests. The user's interaction with the system can be summarized in three stages ():
The user carries out actions through the graphical interface.
These actions are reformulated into corresponding requests and sent to the core processing component via the communication channel.
The requests are forwarded to the database server, which treats them and returns the results.
Results
We have successfully achieved the initial goals for the implant management tool. We developed a GUI-based application that, in a semi-automatic manner, helps surgeons, implant manufacturers, and CAS system developers to continuously keep their systems up to date for clinical use. In doing this, we also developed a new XML implant standard that eases inter-operability and data sharing and provides a close link between manufacturers, CAS system providers, and surgeons. The main functionalities provided are
Add, Delete, Update implant;
Preview implant parameters;
Backup implants; and
Advanced search.
This article describes the entire development process to support XML file manipulation: load implant files via XMLImplantFileReader and backup implants from the database via XMLImplantFileWriter. All the functionalities of the administration tool are implemented in the GUI.
Load XML implant file and preview. Before performing any of the administration tasks, the user can obtain visual feedback such as a preview of the implants that he/she wants to insert or modify. At this stage, one can load an XML implant file and browse each implant.
New implant insertion. Users can insert implants in the database based on the XML file that they initially prepared. If some of the implants already exist in the database, their attributes will be modified by the new values read from the XML implant file.
Update existing implant in the database. Users have to find in the database the implant that they wish to modify by applying a searching filter such as the implant category, implant manufacturer, or implant type. The user browses the implant list, selects one item, then edits the appropriate parameters.
Implant backup. As describe above, users select from the database the list of implants to be backed up by applying searching filters. The user can then select the implants to be saved and add them to a control list. This step could be repeated several times by changing the filtering criteria until the user is satisfied. Finally, he just has to click on the ‘backup’ button, whereupon an implant XML file containing the selected implant will be created and saved in the specified location.
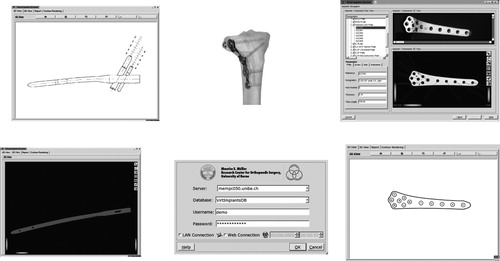
Advanced search. During the planning and navigation of an orthopedic surgical procedure, it is important to find not only the best implant but also the fixation devices that are associated with the selected plate (for trauma surgery). For prosthetic operations, it is also necessary to suggest to surgeons the best available components (hip cup, stem, head, etc.). Our advanced search functionality is intended to provide a filter combination based on existing relationships, constraints, and clinical rules between implants. For the case shown in , the search starts by selecting the anatomy part (e.g., tibia, femur, etc.). As a result, only implants designed for those specific anatomy parts are displayed. We can then apply a precise filter such as implant manufacturer or implant category. Depending on the implant type, we can iteratively continue the filtering process using criteria such as desired implant length, plate hole number, etc. While clicking on a plate in the result list, our system automatically finds the fixation devices (e.g., screws) that can be used with this plate. Two- and three-dimensional views are also provided for visual feedback.
Delete obsolete implant from database. The function delete allows users to remove obsolete implants from the database. The workflow is similar to the backup functionality described above, with the difference that the selected implants will be deleted from the database.
Discussion
We have presented a graphically based implant management tool for use with a computer-assisted orthopedic planning and navigation system. As this tool is built on top of a virtual implant database, we first provided an overview of this new concept and presented our new implant management concept centered around the presented administration tool. After evaluation of existing database management systems, we designed and deployed a multi-platform implant database that addressed the current limitations of existing CAS systems with regard to the way in which implants are managed. Our implant interface provides CAS applications with simultaneous communication and search algorithms for implants. The delivered solution is manufacturer- and CAS-system-independent. Our tests show that our concept enables and facilitates the rapid integration of orthopedic surgical devices into planning and navigation systems Citation[7–9], thanks to the standard communication interface provided between the CAS and the implant management systems. We currently support osteosynthesis plates Citation[9], screws, nails and hip prostheses (stems, cups, and heads). Integration of knee prosthesis components is ongoing. The delivered solution can be used on Linux, Windows, and Solaris operating systems.
Validation tests have been successfully carried out with long-bone fracture-reduction planning software and digital template planning software (both developed at our Institute). The intention of the tests was to evaluate integration issues, network access, speed, and usability of our system within CAS systems (). Moreover, a virtual implant browser system was developed for multi-purpose demonstrations ().
Figure 8. Integration tests with CAS: a 3D implant model (left) or a 2D implant contour image of a LISS plate (right) is selected from our database. [Left: X. Dong and V. Vitanis, 2003; Right: C. Anderegg, 2003.] (color version available online)
![Figure 8. Integration tests with CAS: a 3D implant model (left) or a 2D implant contour image of a LISS plate (right) is selected from our database. [Left: X. Dong and V. Vitanis, 2003; Right: C. Anderegg, 2003.] (color version available online)](/cms/asset/228716d9-1f2a-417c-a4a8-a66bbabd4271/icsu_a_138963_f0008_b.jpg)
During this project, several lessons have been learned from a clinical and software design point of view. This project is still under development, and the following additional features and research topics will be addressed in the near future:
Improving the GUI for routine use by adding additional functionalities, such as ‘undo’, after a delete action.
Processing more implants using our tool and making quantitative performance measurements.
Investigating the fully automatic process by linking our system with CAD tools and directly processing implant data (e.g., by integrating a DXF parser in our design) and storing the implant files in a native XML database.
Validation of surgical efficiency in collaboration with surgeons, manufacturers, and CAS developers.
Improvement of search functionalities, addition of intelligence by exploring rules-based database systems, expert systems, knowledge-based systems, and data mining techniques.
Conclusion
Our proposed solution is a new concept that addresses the limitations of existing CAS systems with regard to orthopedic implant management. Compared with existing solutions, our approach has many advantages: data reusability, security mechanisms, a robust database system, client/server architecture, ease of use, and a framework for RAD which allows CAS application developers to focus more on surgical procedures.
The implant management tool presented here is a new application that addresses the current limitations and fills the gaps between the hospital's available CAS system implants and the implants provided by the manufacturers. Laboratory tests of the system's usability and efficiency have been successful. Some improvements are planned to allow for fully automated implant XML file generation directly from CAD files received from implant manufacturers. However, it is necessary to conduct more exhaustive tests and continue improving the XML implant scheme.
Currently, our application can work locally and with a remote database server via a local network. Planned improvements will enable it to work via secure Internet tunnels.
Thanks to the concept and the tool presented here, we can, in the near future, integrate more clinical rules and ontology into our system. The overall system will be improved to take into account the requirements of surgeons, manufacturers, and CAS system providers.
The proposed implant XML concept and its link with our virtual implant database will improve the inter-operability and integration of implants between CAS systems. New implants can be made available to surgeons rapidly without the need for manual processing.
Acknowledgments
This project is funded by the AO/ASIF Foundation through CARIM (Computer Assisted Reduction and Imaging) project 1. Implant data was provided by Synthes-Stratec.
References
- Suhm N. Long bone trauma. Computer and robotic assisted knee and hip surgery, AM DiGioia, B Jaramaz, F Picard, LP Nolte. Oxford University Press. 2004; 297–306
- Grützner PA, Zheng G, Vock B, Keil C, Nolte LP, Wentzensen A. Computer-assisted osteosynthesis of long bone fractures. Navigation and robotics in total joint and spine surgery, JB Stiehl, WH Konermann, RG Haaker. Springer, Berl 2004; 449–454
- Langlotz F. Potential pitfalls of computer aided orthopedic surgery. Injury Int J Care Injured 2004; 35: S-A17–S-A23
- Langlotz F, Keeve E. Minimally invasive approaches in orthopaedic surgery. Minim Invasive Ther Allied Technol 2003; 12: 19–24
- Sugano N. Computer assisted orthopedic surgery. J Orthop Sci 2003; 8: 442–448
- Zheng G. Advancements of fluoroscopy-based navigation for less invasive orthopaedic interventions. M.E. Müller Institute for Surgical Technology and Biomechanics. University of Bern, BernSwitzerland December, 2002, Ph.D. thesis
- Sagbo S, Zheng G, Langlotz F, Nolte LP. Virtual implants database for computer assisted surgery: a new system to efficiently access orthopedic implants for planning and navigation. Proceedings of 4th Annual Meeting of the International Society for Computer Assisted Orthopaedic Surgery, (CAOS/2004), Chicago, IL, June, 2004, 137–138
- Sagbo S, Zheng G, Vangenot C, Moumni J, Nolte LP. Virtual implants database for computer assisted surgery: a new unified implant access interface for surgical planning, navigation and simulation. Proceedings of MICCAI 2004/DiDaMIC-2004 Workshop on Distributed Databases and Processing in Medical Image Computing, St Malo/RennesFrance, September, 2004, 26–35
- Anderegg C, Langlotz F. The planning of fracture treatment using digital templates. Proceedings of 4th Annual Meeting of the International Society for Computer Assisted Orthopaedic Surgery (CAOS/2004), Chicago, IL, June, 2004, 115–117
- Mohsen AMMA, Sherman KP, Cain TJ, Karpinski MRK, Howell FR, Phillips R, Viant WJ, Griffiths JG, Dyer KDF. End user issues for computer assisted surgical systems. Trans Inst Meas Control 1995; 17(5)265–271
- Jaramaz B, DiGioia A. Total hip replacement navigation technique. Computer and robotic assisted knee and hip surgery, AM DiGioia, B Jaramaz, F Picard, LP Nolte. Oxford University Press. 2004; 97–112
- Taylor RH, Funda J, Joskowicz L, Kalvin AD, Gomory SH, Gueziec AP, Brown LMG. An overview of computer-integrated surgery at IBM Thomas J. Waston Research Center. IBM J Res Dev 1996; 40(2)163–183
- Bächler R, Kowal J, Bourquin Y, Sati M, Nolte L-P. Computer aided biological fracture plate fixation. Proceeding of CAOS-USA, Pittsburgh, PA, June, 1999
- Hofstetter R, Slomczykowski M, Sati M, Nolte L-P. Fluoroscopy as an imaging means for computer-assisted surgical navigation. Comput Aided Surg 1999; 4: 65–76
- Hofstetter R, Slomczykowski M, Krettek C, Köppen G, Sati M, Nolte L-P. Computer-assisted fluoroscopy based reduction of femoral fractures and antetorsion correction. Comput Aided Surg 2000; 5: 311–325
- Slomczykowski MA, Hofstetter R, Sati M, Krettek C, Nolte LP. Novel computer-assisted fluoroscopy system for intraoperative guidance: Feasibility study for distal locking of femoral nails. J Orthop Trauma 2001; 15(2)122–131
- Kahler DM. Image guidance fluoroscopic navigation. Clin Orthop Relat Res 2004, 421: 70–76
- Joskowicz L, Milgrom C, Simkin A, Tockus L, Yaniv Z. FRACAS: a system for computer-aided image-guided long bone fracture surgery. Comput Aided Surg 1998; 3: 271–288
- Wu T, Portheine F, Popovic A, Bast P, Wehmoeller M, Radermacher K (2003) An interface for the data exchange between CAS and CAD/CAM systems. Proceedings of the 17th International Congress and Exhibition (CARS 2003), LondonUK, June, 2003, HU Lemke, MW Vannier, K Inamura, AG Farman, K Doi, JHC Reiber. Elsevier, Amsterdam, 703–709, Computer assisted radiology and surgery
- Schmucki D, Gebhard F, Grützner PA, Hüfner T, Langlotz F, Zheng G. Computer aided reduction and imaging. Injury 2004; 35(Suppl. 1)S-A96–S-A104
- Booch G, Rumbaugh J, Jacobson I. The unified modeling language. User guide. Addison-Wesley. 2001; 3–35
- Dalheimer MK. Programming with Qt. O'Reilly 1999
- Coin3D: http://www.coin3d.org
- Dubois P. MySQL cookbook. O'Reilly 2004
- Kirsten M, Ihringer M, Kühn M, Röhrig B. Object-oriented application development using the caché postrelational database. Springer, Berl 2003
- Date CJ. An introduction to database systems. Addison-Wesley. 2004
- Ambler S. Agile database techniques: effective strategies for the agile software developer. Wiley. 2003