Abstract
Automated methods are presented for the planning of correction osteotomies and osteosynthesis on lower extremities. Intraoperative calibrated X-ray images and kinematic measurements using optical tracking systems are the basis for the identification of the individual anatomy of the patient. The correction input of the surgeon, together with optimization algorithms, allows the calculation of the position and orientation of the osteotomies and the repositioning of the bone fragments. A navigation module supports the surgeon during the execution of osteotomies and repositioning, as well as osteosynthesis. So far, the approach has been evaluated in laboratory trials and ex vivo tests.
Introduction
Correction osteotomies can be considered as an alternative to total joint arthroplasties in the cases of biomechanical deficits of the extremities Citation[1]. In clinical routine, however, it is problematic to identify the correct spatial individual deformities, to determine the optimal cutting planes and the amount of repositioning (translation and rotation of n fragments) necessary and to transfer the planning results into the operative site. Thus, the results of osteotomies strongly depend on the experience and manual skills of the operating surgeon Citation[2]. In general, corrections of multidimensional deformities are nowadays performed using the corticospongeous wedge osteotomy. However, owing to the complex spatial relationships involved, it has been rarely used to date Citation[3].
Some computer-assisted planning systems have already been used in clinical practice for the planning of correction osteotomies Citation[4]. Paley and Pfeil Citation[5] introduced a system based on conventional X-ray projections, using the nomenclature defined by Paley for the planning of osteotomies. However, the system does not permit spatial planning and calculation of the osteotomy plane and does not provide support during the actual execution. A three-dimensional (3D) system was introduced by Ellis et al. Citation[6] for preoperative planning, simulation and intraoperative monitoring of osteomies on the proximal tibia high tibial osteotomy (HTO). Application of this CT-based concept is limited to the knee and it disregards antetorsion. Lin et al. Citation[7] presented a radiograph-based system for planning and execution of osteotomies of the lower extremities that is computer aided, maintaining the mechanical axis and allowing the simulation to perform up to three osteotomies. The system calculates the parameter for the Ilizarov method using non-correlated X-ray images. A 3D CT-based simulation software for HTO, which considers the entire geometry of the leg, has been introduced by Kawakami et al. Citation[8]. The rotational component is identified by comparing the position of the patella in an AAP radiograph. For the 3D planning of corrective osteotomy with complex dislocated positions, a CT-based system was developed by Hesser et al. Citation[9]. In contrast to the systems mentioned earlier, this CT-based system determines the guidance of the cut through optimization, on the basis of the cutting height defined by the surgeon. Prasch Citation[10] proposed a computer-integrated principle for the planning and robotic execution of correction osteotomies. Optimization algorithms are used for 2D–3D registration, but not for determination of the osteotomy plane.
A mathematically more evolved development for optimized 3D planning of single-cut osteotomies on the proximal femur has been presented by Eck Citation[11]. However, this approach is also CT-based and does not consider the leg-length variation during the optimization step. Burgkart et al. Citation[12] presented a planning system that permits the determination of the anatomical axis from intraoperative radiographs. Only the variation of the rotational component is determined. The intraoperative execution is supported by a tracking system. A further contribution to the computer-aided execution of tibial osteotomies in proximity to the knee joint comes from Menetrey et al. Citation[13], who have presented a radiograph-based planning system that computes the size and position of the wedge osteotomy. The only objective of this approach is correction of the leg axis, although all other parameters will be calculated but not optimized.
The identification of the individual antetorsion angle represents a major challenge for information acquisition. Without consideration of these parameters, the single-cut osteotomy is certainly not recommended. The other types of osteotomy procedures are conditionally feasible without definition of the antetorsion. From a functional point of view, the orientation of the kinematic axis of the knee with respect to the femoral neck defines the antetorsion angle. The estimate of the knee axis is accomplished by spotting the epicondyles or the dorsal condyles directly on the CT image or on the patient. The measurement of the epicondyles is subject to high inter- and intra-rater variablility Citation[14]. Tomczak et al. Citation[15] presented a similar procedure for MR tomography. This approach enables a clear display of the cartilage without radiation, but the accuracy and the reproducibility of the results are limited. An alternative to this approach, based on preoperative radiographs, was presented by Rippstein Citation[17], but the procedure turned out to be quite complex for an intraoperative investigation. Investigations with sonography are described in ref. 16 and show standard variations similar to those in CT investigations. In conclusion, our review of the related literature revealed the following challenges.
Information acquisition
So far, CT seems to be mandatory for the identification of the individual anatomy. However, owing to costs and radiation aspects, CT imaging is rarely used in clinical routine for repositioning osteotomies of the lower extremities. Moreover, although CT imaging allows the identification of the epicondyles, the validity of the transepicondylar line for the identification of the knee axis remains a topic of controversy.
Conventional radiographs cannot completely provide the information necessary, because of the projection errors and the missing spatial correlation of multiplanar projections.
Calibrated intraoperative radiographs have been presented as an alternative. However, owing to the limited field of view, the complete determination of the anatomical parameters is not yet satisfactorily solved. In particular, the definition of the knee reference coordinate system remains a critical issue for all the approaches presented so far.
The classical anatomical parameters, derived from conventional radiography, are insufficient to describe the complex spatial deformation in many cases. A different approach using a new description method is essential to obtain a mathematically accurate description of the spatial relationships. However, to enable the surgeon to evaluate and perform the calculated cuts and positionings, the parameters must be transferred back to the conventional radiographic system parameters (as well as to the intraoperative reference system of the operating site by means of navigation).
Optimization
The planning of osteotomies and the subsequent adjustments of bone fragments require a high degree of spatial imagination and represent a complex multidimensional optimization problem. Based on awareness of the individual anatomy of the patient, the following parameters have to be defined: the position of the cut on the anatomical axis (one degree of freedom), the tilt of the cutting plane (two degrees of freedom), and the translation (two degrees of freedom), as well as the rotation (one degree of freedom) on the cutting plane of the second bone fragment. In the case of a wedge osteotomy, the translation of the wedge on the first cutting plane has to be considered (two degrees of freedom), as well as the position (one degree of freedom) and inclination (two degrees of freedom) of the second cut. Hence, the surgeon has to optimize six to 11 degrees of freedom to achieve the goal of the procedure, which includes the weighted correction of the angulation, the antetorsion as well as the translation, and the length of the leg. In addition, medical constraints (listed as a–e below) are to be considered apart from the primary goals (listed as 1–4 below).
Intraoperative implementation
The transfer of the planning into the operative site depends on a couple of internal (individual) and external performance-shaping parameters (such as the ability to think spatially and the manual dexterity of the surgeon, as well as actual stress factors). The surgeon can be supported by a navigation system providing the link between the actual instrument position and the plan. However, the use of navigation systems itself implies additional constraints.
The use of rigid bodies should be limited to minimize the additional risk of infection as well as trauma.
The repositioning and refixation of the bone fragments has to be accurate and time-efficient with sufficient anchorage of the screws.
In most cases, additional devices restrict the movement of the surgeon as well as creating new challenges concerning the human/machine interface.
Methods
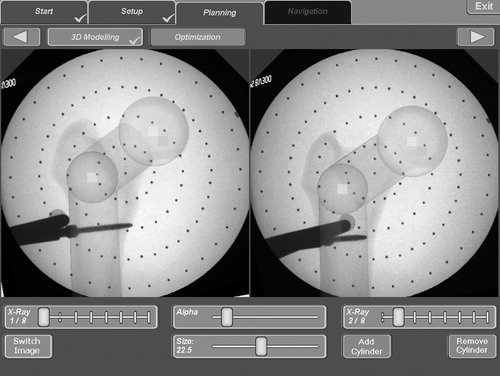
A planning system in combination with an optical tracking system based on intraoperative calibrated radiographs and kinematic data acquisition serves as a starting point for the computation of the osteotomies. The main problem in the determination of spatial deformities (especially for a single-cut osteotomy) is the identification of the antetorsion angle. Therefore, an anatomical model is introduced and adapted on the basis of intraoperative knee motion analysis and correlating radiographs of the femoral neck (). This model supplies an individual and reproducible description of false positions in a mathematically descriptive form Citation[18].
The computation of the cutting planes for the osteotomy depends on the individualized anatomical model of the patient, as well as on the following correction parameters (primary goals):
leg length,
translation,
antetorsion,
angulation.
Apart from these four optimization goals, a set of constraints are considered to ensure a successful operational implementation and avoid potential complications.
(a) A fast rehabilitation also depends on the area of contact of the bone segments within the osteotomy planes Citation[5], Citation[9]. Coverage of at least 67% is desired Citation[11].
(b) The slope of the osteotomy is limited by the maximal length of the cut as well as by mechanical considerations concerning the resulting shear stresses.
(c) The rotation of the bone fragments with respect to one another is likewise limited. Unrealistic solutions must be avoided.
(d) For the two-cut or wedge osteotomy, an additional condition concerns the avoidance of a (mathematically possible) penetration of the bone fragments, which of course requires a solution that is possible in reality.
(e) The range of motion of the hip joint must be taken into consideration to avoid impingement.
(i) the inclination of the osteotomy planes,
(ii) the extent and direction of the rotation of the bone segments,
(iii) the shifting vector in the osteotomy planes,
(iv) the height of the osteotomy along the bone axis within the defined range.
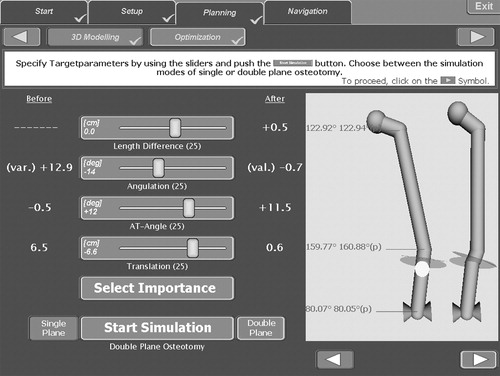
Figure 2. Optimization interface with preoperative (left column), target (center column) and calculated (diagram at right) parameters for leg-length variation, angulation, antetorsion and translation.
For the evaluation of the optimization process and the correction osteotomies calculated by the system, a virtual bone model was ‘deformed’ by defined osteotomies. The parameters of these virtual osteotomies and the subsequent osteosynthesis of the bone fragments were then stored. The deformed bone model was then used as an input to the optimization algorithm. Hence, the system should calculate an inverse solution resulting in the undeformed original bone model.
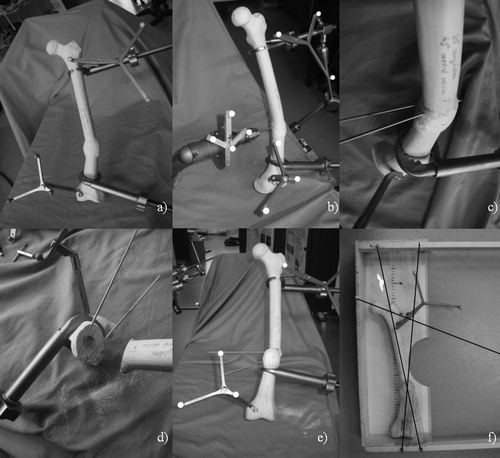
In a second study, deformed plastic bones (Sawbones Europe AB) were corrected by the planning system (). The investigations were repeated by three individuals with related medical expertise using six different bone models. The preoperative deformity was determined using the planning system as well as an anatomical measuring board (). An ‘intraoperative’ calibrated C-arm system was used for X-ray image acquisition. The investigation table was used as an auxiliary plateau of the tibia, in order to determine the kinematic axis of the knee. For all four optimization criteria (listed earlier as 1–4), the same priorities were defined. The osteotomy areas were selected above and below the CORA. The osteotomy planes were transferred to the operative site by two navigated k-wires for each plane. Subsequently, the bone was osteotomized with an oscillating saw in accordance with the results of the optimization process. After the navigated osteosynthesis, the postoperative values were measured again with the help of the planning system and the measuring board.
Figure 3. Worksteps of the second study: (a) preoperative deformed bone with fixed distal and proximal reference bases; (b) navigated drilling with k-wires; (c) marked osteotomy plane; (d) after manual osteotomy; (e) navigated osteosynthesis; and (f) measurement using a standard measurement board for anatomical investigations.
Results
The results of the first attempt at validating the selected optimization procedure are represented in . The optimization algorithms found the correct solution in 100% of cases with high accuracy. However, the upper limit of the accepted intraoperative computing time of 1 min was exceeded. The significantly shorter results in were reached after modification and improvement of the procedure and repeated testing.
Table I. Results of first attempt at validating the selected optimization procedure.
Moreover, the second investigation on plastic bones showed an average postoperative error of angulation of 0.6° (valgus), a remaining antetorsion error of 12.4°, a remaining translation deficiency of 1 cm, and a mismatch of leg length of 0.2 cm for a single-cut osteotomy. The execution as a single-cut osteotomy explains the high remaining rotational error. The standard deviations amounted to 1.4° for the angulation, 1.1° for the rotation and 6 mm for the translation, and for the leg-length variation values of 2 mm could be determined. The evaluation of the wedge osteotomy planning module is the subject of current investigations. Initial results show a higher potential to correct larger deformities. Initial qualitative investigations within the framework of an ongoing ex vivo study have confirmed the results of the laboratory trials ().
Discussion
Repositioning osteotomies represent a major challenge for orthopedic surgeons, because several degrees of freedom in the structures as well as the functional consequences for support and locomotion have to be optimized. The problems of executing the planning and navigation of the osteotomy consist of the identification of the individual anatomy, the positioning of cutting directions, and spatial adjustment of the bone fragments, taking into account partially contrary biomechanical and medical constraints and optimization criteria. With the realization of this planning system, a proposed solution for these problems is presented. A platform was created for the planning and navigation of different osteotomy procedures.
The combination of intraoperative calibrated X-ray images and kinematic methods allows an exact identification of individual bone morphology. In particular, the intraoperative determination of the antetorsion can be accomplished effectively. The definition of an interface between the mathematical parameter optimization and the conventional concept of the medical user is crucial. Therefore, an anatomical model was introduced to identify conventional parameters. After identification of the individual anatomical model and determination of the correction parameters for a wedge osteotomy, an 11-dimensional optimization problem still remained for the definition of the cuts and the adjustment of the bone fragments. Hence, different optimization algorithms have been applied and evaluated. Angulation, antetorsion, the change of leg length and translation have been defined as optimization goals. The demand for a less traumatic intraoperative implementation with a lower complication rate and fast rehabilitation time is again reflected in the optimization constraints (angle of the cut, maximal rotation and minimum bone contact area). However, soft tissue has not been taken into account for biomechanical optimization. This aspect is one topic of our ongoing research. The intraoperative execution of osteotomy and osteosynthesis is supported by a tracking system. Postoperative results under laboratory conditions show a good match between the virtual planning model as the goal and the real bone structure as the result.
References
- Pauwels F. Atlas zur Biomechanik der gesunden und kranken Hüfte. Springer, Berlin 1973
- Nagel A, Insall JN, Scuderi GR. Proximal tibial osteotomy. J Bone Joint Surg 1996; 78A(9)1353–1357
- Gürke L, Strecker W, Martinoli S. Korrektur mehrdimensionaler Deformationen durch eine einzige Osteotomie—Graphische Analyse und Operationstechnik. Der Unfallchirurg 1999; 102: 684–690
- Gladbach B, Pfeil J, Heijens E. Computerassistierte Planung und Simulation von Korrekturosteotomien an der unteren Extremität. Sonderdruck Orthopädische Praxis 2001; 37: 11–18
- Paley D, Pfeil J. Prinzipien der kniegelenknahen Deformitätenkorrektur. Orthopäde 2000; 29(1)18–38
- Ellis RE, Tso CY, Rudan JF, Harrison MM. A surgical planning and guidance system for high tibial osteotomy. Comput Aided Surg 1999; 4(5)264–274
- Lin H, Birch JG, Samchukow ML, Ashman RB. Computer-assisted surgery planning for lower extremity deformity correction by the Ilizarov method. J Image Guided Surg 1995; 1: 103–108
- Kawakami H, Sugano N, Nagaoka T, Hagio K (2002) 3D analysis of the alignment of the lower extremity in high tibial osteotomy. Proceedings of the 5th International Conference on Medical Image Computing and Computer-Assisted Intervention (MICCAI 2002), TokyoJapan, September, 2002, T Dohi, R Kikinis. Springer, Berlin, 261–267, Lecture Notes in Computer Science Vol. 2489
- Hesser J, Krivonos O, Manner R, Keppler P, Gebhard F, Kinzl L. Operation planning of correction osteotomies in 3D. Biomed Tech (Berl) 2002; 47(Suppl. 1, Pt 1)90–92
- Prasch J. Computerunterstützte Planung von chirurgischen Eingriffen in der Orthopädie. Springer, Berlin 1990
- Eck M. Three-dimensional determination of an oblique osteotomy in the hip by mathematical optimization fulfilling some anatomical demands. J Biomechan 1990; 23(10)1061–1067
- Burgkart R, Gottschling H, Roth M, Schweikard A, Regenfelder F (2003) Intraoperative planning and computer assisted navigation of complex multi-planar correction osteotomies at the proximal femur using a standard C-arm fluoroscopy. Proceedings of 3rd Annual Meeting of the International Society for Computer Assisted Orthopaedic Surgery (CAOS-International), MarbellaSpain, June, 2003. Steinkopff, Darmstadt
- Menetrey J, Paul M. Möglichkeiten der computergestützten Navigation bei kniegelenknahen Osteotomien. Orthopäde 2003; 33: 224–228
- Jenny JY, Boeri C. Low reproducibility of the intra-operative measurement of the transepicondylar axis during total knee replacement. Acta Orthop Scand 2004; 75(1)74–77
- Tomczak R, Günther K, Pfeifer T, Häberle HJ, Rieber A, Danz B, Rilinger N, Friedrich JM, Brambs HJ. Messung des femoralen Torsionswinkels von Kindern durch Magnetresonanztomographie im Vergleich zu CT und Ultraschall. RöFO 1995; 162: 224
- Keppler P, Strecker W, Kinzl L. Analyse der Beingeometrie— Standardtechniken und Normwerte. Chirurg 1998; 69(11)1141–1152
- Rippstein J. Zur Bestimmung der Antetorsion des Schenkelhalses mittels zweier Röntgenaufnahmen. Zeitschrift für Orthopädie und ihre Grenzgebiete 1955; 86: 345–360
- Schkommodau E. Modellbasierte Multiparameteroptimierung für die Plaung und Durchführung gelenkerhaltender Umstellungsosteotomien. Shaker, Aachen 2005
- Spelucci T. Numerische Verfahren der nichtlinearen Optimierung. Birkhäuser, Berlin 1993