Abstract
Objective: To determine the role of clinical background when assessing the learning effect using a virtual-reality (VR) laparoscopy simulator (LapSim®).
Materials and methods: Test subjects were 12 final-year medical students (Group A) and 12 inexperienced residents (Group B) with no previous experience of VR simulators. First, to establish a baseline, both groups performed the “clip application” task twice. They then completed a training program of increasing difficulty (coordination, cutting and clip application), after which both groups were re-tested using a difficult level of the “cutting” task as an endpoint measurement. Time to complete the tasks, as well as trauma and precision parameters, were scored.
Results: Before training, times to complete the baseline task, as well as parameters of trauma and precision, were similar for both groups. After training, Group B (residents) completed the cutting task significantly faster than Group A (students). However, the former group also showed significant improvement in trauma and precision parameter scores in the endpoint measurement.
Conclusion: These results suggest that clinical background and understanding of the clinical value of a training program lead to faster acquisition and improvement of laparoscopic skills as performed on the laparoscopy simulator. Thus, medical students or other personnel not involved in practical surgery may be unsuitable as candidates for assessing the value of a VR training program.
Introduction
Patient safety is an increasingly important concern that can be enhanced by improving surgical technique. Technical skills in surgery have traditionally been taught using the apprenticeship model, but the advent of minimally invasive surgery brought about the use of simulation as a training tool. Such simulations make it possible to offer a wide range of repeatable surgical situations, and thereby conduct assessments based on direct observation of performance Citation[1].
Laparoscopic simulation has proven effective in providing skills that are transferable to the operating room (OR) Citation[2–4]. Computer simulation is free of ethical considerations, but tends to be expensive and is currently incompletely developed Citation[5]. Nevertheless, training in computer-simulated laparoscopic environments has become increasingly popular in recent years, despite the limited evidence for the efficacy of such approaches.
The fact that such training can improve laparoscopic surgical skills has been demonstrated previously. Rosser et al. Citation[6] reported that, after only one series of tasks, the time taken to complete an intracorporal stitch improved significantly, with further significant improvement at the end of 10 repetitions. A similar program using the MIST-VR® simulator demonstrated significant improvement in knot-tying speed after a 5-day training period Citation[7].
The current study was designed to determine the contribution of clinical background to skills training on a virtual reality (VR) laparoscopy simulator (LapSim®). That is, to what extent does the application of clinically significant ex situ training affect performance?
Materials and methods
Simulation model
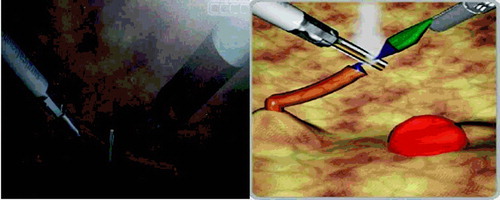
The simulator used in this study (LapSim®, Surgical Science Ltd., Goeteborg, Sweden) creates a virtual laparoscopic system using a computer (Windows XP®), a video monitor and a laparoscopic interface containing two pistol-grip instruments and a diathermy pedal (). The LapSim® software contains the basic modules referred to as Cutting, Clip application and Coordination, in which the level of complexity and difficulty can be adjusted as described previously Citation[1], Citation[5]. The Cutting and Clip application modules represent a surgical maneuver during laparoscopic operations, and the corresponding simulator views are presented in . The simulations involve the use of multiple instruments, as well as increasing levels of risk and stress. When a vessel is over-stretched, it tears and causes bleeding, requiring a prompt response. Likewise, bleeding will occur if clips are not precisely placed and fail to close the vessel. Instruments available in the simulation are a clip instrument, a grasper, scissors and a suction device.
Figure 1. LapSim® device with the Immersion Medical interface and a graphic display of the clip application on the monitor.
Each of the skills may be adjusted to different levels of procedural complexity by increasing the level of difficulty of the task.
For this study, the clip application task was adjusted to a medium level of difficulty as the baseline measurement. This means that the size of the target areas is reduced by half and the vessel has double the stretch sensitivity. When bleeding occurs, the simulated blood flow averages 2 liters/min.
The cutting task was set at a difficult level as the endpoint measurement. This module introduces the user to actual surgical procedures: cutting and using ultrasonic scissors or forceps. Accordingly, this module features a third manipulation device: a foot pedal used to trigger the cutting instrument. The target area is reduced to one third and the vessel has threefold stretch sensitivity. When bleeding occurs, the simulated blood flow averages 3 liters/min.
The training program consisted of the coordination, clip application and cutting tasks with increasing levels of difficulty. For each individual test subject, as well as for the entire group, the following parameters were recorded: Time to complete task (min); blood loss (ml); number of dropped clips; number of badly placed clips; number of incomplete target areas; % stretch damage; incidence of tissue damage; % maximal tissue damage; and % drop failure.
Study groups
These comprised 12 final-year medical students (5 women and 7 men) in Group A, and 12 inexperienced residents (4 women and 8 men) in Group B. Subjects ranged in age from 25 to 34 years. None had any previous experience with a VR simulator. All students received briefly instruction regarding the VR technique of coordination, clip application and cutting. Use of the laparoscopic instruments was demonstrated, and the students were given time to practice until they felt comfortable. Both groups then performed the clip application task at a medium level as a baseline measurement. Each subject completed the training program specified above. At the end of the study, each subject completed the cutting task at a difficult level as the endpoint measurement.
Statistics
The data was imported by the simulator computer directly into an MS Excel® worksheet. With the help of a statistics program (SPSS), the data was analyzed descriptively. Nonparametric analysis (Wilcoxon test) was used to determine the difference between the performance values for each attempt and the values obtained from the entire set of consecutive attempts. The difference in performance between the two groups was analyzed using the Mann-Whitney test. The level for statistical significance was set at p < 0.05.
Results
All 24 subjects completed the study as described in the preceding section.
Baseline performance
For Group A, completion of the clip application task baseline took a median of 154 s (range: 68.3–206.6 s). Median score for the trauma parameter “stretch damage of the vessel” was 100% (range: 66.2–100%). Median value for the precision parameter “badly placed clips” was 0 (range: 0–2).
For Group B, completion of the clip application task baseline took a median of 126.7 s (range: 34.7–206.6 s) (p > 0.05). Median score for the trauma parameter “stretch damage of the vessel” was 100% (range: 64.8–100%). Median value for the precision parameter “badly placed clips” was 0 (range: 0–1).
Endpoint performance
For Group A, completion of the cutting task endpoint took a median of 282 s (range: 148.5–478.3 s). Median score for the trauma parameter “tissue damage” was 8 times (range: 1–58). Median value for the precision parameter “rip failure of the cutting area” was 80% (range: 20–100%).
For Group B, completion of the cutting task endpoint took a median of 206.3 s (range: 87.8–348 s) (p < 0.05). Median score for the trauma parameter “tissue damage” was 1 time (range 0-9). Median value for the precision parameter “rip failure of the cutting area” was 40% (range 0–100%).
Discussion
The learning of psychomotor skills to master laparoscopic procedures requires more than passive observation Citation[8]. For this reason, the traditional means of acquiring skills for minimal invasive surgery by acting as a “camera holder” is inferior to active training. However, the OR is not suited to serve as a classroom, due to factors such as concern for the patient, time constraints and costs. Training outside the OR offers a structured educational opportunity with stress modulation, which reduces the trainees' stress in the OR.
Assessing the learning effect is an essential element of training programs. Ahlberg et al. reported that the virtual laparoscopy simulator (MIST-VR) did not improve the surgical skills of the students during laparoscopic appendectomy in a porcine model Citation[9]. In a study of the value of VR training for ureteroscopy, Ogan et al. concluded that VR training is unable to override the value of clinical training for medical students Citation[10]. If the learning effect of a VR simulator were indeed questionable, it might not be worthwhile to invest in expensive VR training systems.
The aim of this study was, therefore, to establish whether medical students lacking clinical background in surgery are suited to assess the learning effect of a VR simulator. Such information has hitherto been unavailable.
We compared the existing laparoscopic skills of final-year medical students lacking clinical background in surgery with those of young, inexperienced residents. Both groups performed similarly in baseline skills. The training effect of a one-day training course using the Lapsim® showed a significant difference between the groups at the endpoint measurement. Although there was no difference in existing laparoscopic skills between the groups, after the training course the residents performed the cutting task faster and with fewer mistakes than the medical students (p < 0.05).
This finding clearly indicates that medical students' lack of clinical background, along with possible lack of motivation to improve their surgical skills, may cause false-negative results with regard to the training effect of such a system. This result does not come as a surprise. However, and more importantly, it indicates that, when assessing the usefulness of a laparoscopy simulator, participants must be selected carefully.
We now know that VR simulators, if appropriately used, may in fact be closer to real procedures than previously thought. The importance of a clinical background is relevant for surgical education; medical students should receive more theoretical instruction about practical surgery before being given a chance to apply their knowledge in practical settings. It can be expected that such performance-based curricula will significantly enhance the efficiency and efficacy of skill training by means of a VR laparoscopy simulator.
Conclusion
These results suggest that lack of clinical background in surgery may decrease the efficacy of a training setup like the virtual reality laparoscopy simulator. Prior to practical training, didactic sessions may be important as a complementary tool in the context of a curriculum.
References
- Hassan I, Sitter H, Schlosser K, Zielke A, Rothmund M, Gerdes B. A virtual reality simulator for objective assessment of surgeons' laparoscopic skill. Chirurg 2005; 76(2)151–156
- Grantcharov T P, Kristiansen V B, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P. Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 2004; 91(2)146–150
- Seymour N E, Gallagher A G, Roman S A, O'Brien M K, Bansal V K, Andersen D K, Satava R M. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 2002; 236(4)458–463;, discussion 463–464
- Gallagher A G, Cates C U. Virtual reality training for the operating room and cardiac catheterisation laboratory. Lancet 2004; 364(9444)1538–1540
- Hassan I, Koller M, Zielke A, Celik I, Langer P, Lehmann K, Rothmund M, Gerdes B. Improvement of surgical skills after a three-day practical course for laparoscopic surgery. Assessment of skill enhancement with a Virtual Reality Laparoscopy Simulator. SMW, (submitted for review)
- Rosser J C, Rosser L E, Savalgi R S. Skill acquisition and assessment for laparoscopic surgery. Arch Surg 1997; 132: 200–204
- Kothari S N, Kaplan B J, De Maria E J, Broderick T J, Merrell R C. Training in laparoscopic suturing skills using a new computer-based virtual reality simulator (MIST-VR) provides results comparable to those with an established pelvic trainer system. J Laparoendosc Adv Surg Tech A. 2002; 12: 167–173
- Bergamaschi R, Dicko A. Instruction versus passive observation: a randomized research study on laparoscopic suture skills. Surg Laparosc Endosc Perc Tech 2000; 10: 319–322
- Ahlberg G, Heikkinen T, Iselius L, Leijonmarck C E, Rutqvist J, Arvidsson D. Does training in a virtual reality simulator improve surgical performance?. Surg Endosc 2002; 16(1)126–129
- Ogan K, Jacomides L, Shulman M J, Roehrborn C G, Cadeddu J A, Pearle M S. Virtual ureteroscopy predicts ureteroscopic proficiency of medical students on a cadaver. J Urol 2004; 172(2)667–671