Abstract
Objective: Modern computer assisted surgery (CAS) systems allow accurate positioning of the implants in navigated Total Knee Arthroplasty (TKA). However, when an operation is performed with a navigation system, it is important to know if the anatomical situation of the knee is reflected equally in both the preoperative image (e.g., CT) and the intraoperative navigation setup. In this study, we compared the preoperative anatomical situation to the virtual intraoperative situation of the navigation setup.
Material and Methods: We analyzed 24 navigated operations. Intraoperatively, the condylar twist angle (CTA) was documented with the navigation system by measuring the angle between the transepicondylar axis (TEA) and posterior condyle axis (PCA). This data was compared with the preoperative data from the CT scan.
Results: Statistical analysis revealed that there was no correlation between the pre- and intraoperative data (r = 0.095).Conclusions: Statistically, there is no possibility of collecting the same angles and axes when using the two different methods (CT and navigation) on the same knee. It is not possible to copy the preoperative anatomical situation exactly with the virtual intraoperative data. Reasons for this include systematic errors, as well as inter- and intraobserver errors in both methods.
Objective
Since the introduction of computer assisted surgery (CAS) in clinical medicine during the 1990s, CAS and navigation have become increasingly popular, especially in central Europe. In Germany, for example, there are apparently over 500 hospitals using CAS applications in orthopaedic surgery, and the number of navigated operations is constantly increasing, particularly in total hip replacement (THR) and total knee arthroplasty (TKA).
Several studies on navigated versus freehand TKA have shown that the mechanical alignment after TKA can be improved by using a navigation system Citation[1–6]. However, there are several hints as to possible sources of error during navigated TKA, especially during the registration process when essential landmarks for the positioning of the prosthesis are defined. For example, Jerosch et al. Citation[7] reported a very high variation in the reproducibility of landmarks and axes of the human knee. They measured a variation of up to 23° for inter-individual definition of the transepicondylar axis (TEA) at the cadaveric knee.
It is essential to know that the overall error during a navigated operation is based primarily on deviation and lack of precision during the registration process. A recently published study on the accuracy of palpation from orientation points in navigated TKA showed a maximum of 14.6° of interobserver deviation during palpation of landmarks. The maximum intraobserver deviation was 16.0 mm. The mean deviations at the femur were 2.9 mm (interobserver) and 4.0 mm (intraobserver) Citation[8]. Therefore, precise and reproducible assessment of landmarks by the surgeon is one of the keys to success in every navigated operation.
Other sources of inaccuracy, not just for navigated implantations but for all total knee procedures, are observer errors in the analysis of preoperative radiological images. In 1994, Mantas et al. Citation[9] investigated the angular difference between the posterior condyle axis (PCA) and the TEA on 38 human femora. They found the TEA to be externally rotated by approximately 5° with no statistical difference between the left and right femur (the respective standard deviations were ± 2.1° and ± 2.3°). However, the authors did not distinguish between the clinical TEA and the surgical TEA. The latter connects the most prominent point at the lateral condyle to the sulcus of the medial condyle. The angle between the surgical TEA and the PCA is defined as the posterior condyle angle. The clinical TEA connects the two most prominent points at both the medial and lateral condyles. The angle between the clinical TEA and the PCA is called the condylar twist angle. The average difference between the posterior condyle angle and the condylar twist angle is 3.0–3.2°. However, an intraobserver error of 1.1 ± 0.6° has to be taken into account as a result of difficulties in defining the landmarks in severely deformed osteoarthritic knees Citation[10].
The possible inaccuracies in preoperative (CT-based) and intraoperative (landmark-based) assessment lead one to anticipate another question that must be taken in account during navigated TKA: Is the anatomy (landmarks) of a knee reflected equally in both the preoperative radiological image (CT scan) and the intraoperative navigation setup? However, a search of the MEDLINE database using the mesh terms “navigation”, “correlation”, “landmarks” and “TKA” found no studies that focused on this question exclusively, especially with reference to the TKA procedure.
Our present study focuses on a regression and correlation analysis of axes assessed preoperatively on a CT scan and intraoperatively during navigated implantation of a TKA prosthesis.
Material and methods
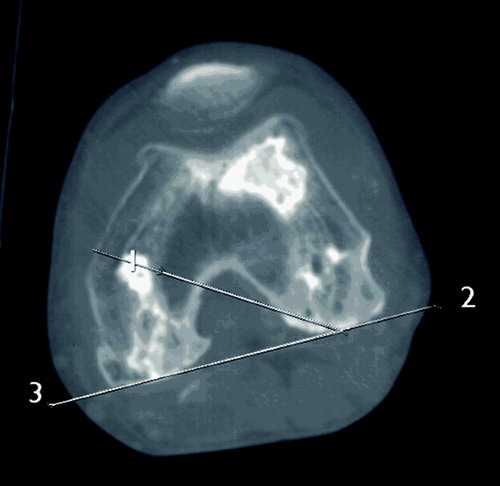
For the CONVERNA study (CONventional VERsus NAvigated TKA; study protocol accepted by the local institutional review board), all patients admitted to the clinic of the senior author for primary TKA were studied prospectively. Apart from the usual clinical and anamnestic data, all patients underwent a pre- and post-operative CT scan of the operated leg (using a General Electric LightSpeed Plus CT scanner) to document the rotation of the distal femur preoperatively and the rotation of the femoral component postoperatively. The assessment of rotation of the distal femur was performed according to the technique described by Waidelich et al. Citation[11], with three CT scans being taken of the examined leg (center of femoral head/center of greater trochanter/distal femur at level of TEA). According to the axial CT image of the distal femur, the PCA and TEA were defined by the radiologist: The most prominent points of the medial and lateral condyles were connected to the TEA, while the PCA was defined as the tangent at the posterior condyles. The angle between theses two axes was then measured ().
During the randomized trial, every second operation was performed with intra-operative use of a navigation system (VectorVision2, BrainLAB AG, Heimstetten, Germany; Software 1.1, CT-free). The implant used for all knees was the LCS complete prosthesis with a mobile bearing inlay (DePuy Orthopaedics, Inc.). In all cases, the components were cemented and the patella was replaced. The preoperative status of the patients in the two groups (navigated versus freehand) was not significantly different with regard to general aspects (age, weight, sex, etc.) or local parameters (knee function, long leg axis, etc.).
During the navigated operations, the surgeon defined both the medial and lateral epicondyles at the distal femur. The software then connected these two points to the TEA. For definition of the PCA, the medial and lateral condyles were palpated with the pointer, collecting a cloud of surface points representing the condyles. The system then connected the two most dorsal points of the cloud of points to the PCA. shows an intraoperative screenshot during the navigation with both axes and the calculated angle displayed.
Figure 2. Screenshot during the navigation process: calculation of the angle (in this case 3.2°) between the TEA (yellow line) and PCA (blue line).“Ext.Rot. from Post.Line” refers to the rotation of the femoral component in relation to the PCA. By definition, the femoral component of the prosthesis is always positioned parallel to the TEA. Therefore, the number of degrees by which the prosthesis is rotated in relation to the PCA is equivalent to the condylar twist angle. [Color version available online]
![Figure 2. Screenshot during the navigation process: calculation of the angle (in this case 3.2°) between the TEA (yellow line) and PCA (blue line).“Ext.Rot. from Post.Line” refers to the rotation of the femoral component in relation to the PCA. By definition, the femoral component of the prosthesis is always positioned parallel to the TEA. Therefore, the number of degrees by which the prosthesis is rotated in relation to the PCA is equivalent to the condylar twist angle. [Color version available online]](/cms/asset/8cde48e7-eb1d-42ba-9283-76f92f5a73d3/icsu_a_163248_f0002_b.jpg)
For statistical analysis of the data we performed a regression and correlation analysis according to the method of Passing and Bablock Citation[12] with EVAPAK® for Windows, Version 3.0.1 (Roche Diagnostics, Mannheim, Germany).
Results
In the period from March 2003 to December 2003, 48 patients were included in the study, giving a total of 24 navigated implantations. No technical problems occurred during preoperative CT or intraoperative navigation. The average preoperative angle between the TEA and PCA on the CT scan was 3.8 ± 2.3°. During the operations, the average angle measured by the surgeon with the navigation system was 3.2 ± 2.8°. Statistical analysis according to Passing and Bablock Citation[12] revealed no correlation between the pre- and intraoperative data (correlation coefficient r = 0.095 and tau = 0.072; ).
Discussion
Every form of radiological assessment is associated with either intra- and interobserver errors or systematic errors in the system used. In X-ray diagnostics, for example, rotation and flexion of the knee is very important. Internal rotation leads to valgus malassessment, and external rotation to varus malassessment. With an angle of 10° rotation or flexion while the X-ray is being taken, the deviation of the axis is 0–2°. However, with an angle of 10–20° the deficiency for the tibio-femoral axis can be as high as 7.4° Citation[13], Citation[14]. Intra- and interobserver mistakes are reported to be up to 1.9° in assessment of X-rays Citation[15], Citation[16].
CT-based measurement of angles and axes
The problem of rotation of the distal femur during CT analysis by use of the clinical and surgical TEAs has already been pointed out. In our study, the surgical TEA was used during pre- and intraoperative assessment. The condylar twist angle was found to be 3.8 ± 2.3°, which is within the range of 3.5 ± 6.8° mentioned in the literature Citation[17], Citation[18]. While measuring these angles, the positioning of the single axial CT scan in which the angles are defined is very important. The most prominent points at the medial and lateral condyles are usually not positioned at the same level as the distal femur and cannot be found in a single CT image. Hence, in the majority of cases, the most prominent point can be either above or below the CT level chosen for measurement. Of course, the same applies to the definition of the PCA. Therefore, relying on only a single CT level of the distal femur means that the risk of incorrectly assessing the real anatomical situation of the knee is very high.
Navigation-based measurement of angles and axes
As already mentioned in the introduction, there are reports of very high variation in the reproducibility of landmarks and axes Citation[7]. As in another study Citation[9], we were unable to confirm these high rates in our investigation. During intraoperative definition of the landmarks, the standard deviation was only ± 2.8° (range: 0.1° to 9.3°). However, it should be pointed out that 23 of 24 knees in our study were operated by the first author (M.O.). Therefore, our results represent an intraobserver deviation and not an interobserver deviation, as in the report of Jerosch et al. Citation[7].
Once the registration process is complete, a very high reproducibility of intra-operative measurement can be achieved during a navigated procedure (mean intra-observer variation of the coronal mechanical femoro-tibial angle = 0.1 ± 0.7°) Citation[19].
Apart from the intra- and interobserver error, there are also system-immanent errors depending on the navigation system used. This overall navigation error can be attributed to software, hardware or human error, and can appear pre- or intraoperatively Citation[20].
The hardware components of a modern navigation system are highly developed. For example, the deviation of the camera (Polaris, Northern Digital, Inc.) of the BrainLAB system is reportedly only 0.35 mm (R. Schmid, BrainLAB, personal communication, 2004). In the literature, the overall deviation of the modern system is known to be approximately 1–2 mm or less than 1° Citation[20], Citation[21]. The overall error arises mainly from deviation and lack of precision during the registration process.
The correct and reproducible assessment of landmarks by the surgeon is a very important step in every navigated operation. The shorter the axis calculated by the navigation system according to the landmarks defined by the surgeon, the greater the influence of a deviation. Changing the end-point of a short axis will lead to a considerable change in the calculated angle, whereas changing the end-point of a long axis will hardly influence the overall angle. Therefore, in the study by Fuiko et al. Citation[8] mentioned above, the mean deviation of the mechanical femoral and tibial axis was low (0.1°/0.2°), but a greater deviation was found in the TEA (1.3°) and Whiteside's line (2.3°), with a range of up to 7.6°.
Conclusion
Analysis of the presented data shows that the average condylar twist angle measured preoperatively using a CT scan is not different from the average condylar twist angle measured intraoperatively with a navigation system. However, there was no correlation in regression and correlation analysis of the data. Statistically, there is no possibility of collecting the same angles and axes when using the two different methods (CT versus navigation) on the same knee. With the setup presented, it is not possible to copy the preoperative anatomical situation exactly with the virtual intraoperative data.
The reason for this is firstly inter- and intraobserver error during assessment of the landmarks intraoperatively. Secondly, a standardized method for measuring and performing the preoperative CT scan is very hard to achieve. Therefore, the preoperative data collected during the CT scan cannot be compared with the intraoperative data collected with the navigation system. When planning a navigated TKA, the surgeon should always keep these facts in mind. The anatomical situation one is expecting based on the preoperative image (CT) cannot be copied exactly by the virtual navigation setup.
To obtain a standardized and reproducible preoperative measurement of the o.m. angles and axes, a 3D reconstruction of the distal femur is necessary. Only with a 3D model of the complete distal femur will the axes and angles be assessed correctly. Therefore, for future measurement and assessment, a 3D reconstruction is essential and should be performed routinely. However, a 3D CT of the distal femur necessitates much greater radiation exposure for the patient than a single CT scan, and on ethical grounds it might be difficult to acquire sufficient data for a valid statistical analysis. In the current study, the local ethics committee (IRB) found the study protocol acceptable as it used the technique of Waidelich et al. Citation[11], which requires only three CT scans of the examined leg to assess rotation and the axes and angles mentioned above. As valid data on the preoperative status of a knee with regard to the axes and angles is currently unobtainable using the usual preoperative radiological methods, we recommend individual assessment of the anatomical situation and the rotation of the components for every operation. For navigated operations, the preoperative radiological status of a knee can be neglected, because there is no correlation to the intraoperative situation. During the registration process, a complete virtual picture of the knee is created anyway, and this can be used for assessment of the “preoperative” status while performing the operation. To reduce inter-observer error during the assessment of landmarks, navigated operations should not be performed by multiple surgeons, especially when the data is to be analyzed for study purposes.
References
- Clemens U, Miehlke R K, Kohler S, . Computer assisted navigation with the OrthoPilot-System and the Search-Evolution-Knee prosthesis. Results of a multicenter study. W Konermann, R Haaker, et al. Springer, Berlin 2003; 207–216, Navigation und Robotik in der Gelenk- und Wirbelsäulenchirurgie
- Jenny J Y, Boeri C. Computer assisted implantation of a total knee arthroplasty: a case-controlled study in comparison with classical instrumentation. Rev Chir Orthop Reparative Appar Mot 2001; 87(7)645–652
- Oberst M, Bertsch C, Wuerstlin S, Holz U. CT-analysis of leg alignment after free hand and navigated TKA: Preliminary results of a controlled, prospective and randomised study. Unfallchir 2003; 106: 941–948
- Perlick L, Bäthis H, Tingart M, Perlick C, Grifka J. Navigation in total-knee arthroplasty: CT-based implantation compared with the conventional technique. Acta Orthop Scand 2004; 75(4)464–470
- Saragaglia D, Picard F, Chaussard C. Computer-assisted knee arthroplasty: Comparison with a conventional procedure. Results of 50 cases in a prospective randomised study. Rev Chir Orthop Repatrice Appar Mot 2001; 87(1)18–28
- Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A. Positioning of total knee arthroplasty with and without navigation support. A prospective randomised study. J Bone Joint Surg Br 2003; 85(6)830–835
- Jerosch J, Peuker E, Philipps B, Filler T. Interindividual reproducibility in perioperative rotational alignment of femoral components in knee prosthetic surgery using the transepicondylar axis. Knee Surg Sports Traumatol Arthrosc 2002; 10: 194–197
- Fuiko R, Kotten B, Zettl R, Ritschl P. The accuracy of palpation from orientation points for the navigated implantation of knee prostheses. Orthopäde 2004; 33: 338–343
- Mantas J P, Bloebaum R D, Skedros J G, Hofmann A A. Implications of reference axes used for rotational alignment of the femoral component in primary and revision knee arthroplasty. J Arthroplasty 1992; 7(4)531–535
- Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y. Computer tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty 2001; 16(4)493–497
- Waidelich H-A, Strecker W, Schneider E. Computed tomographic torsion-angle and length measurement of the lower extremity. The methods, normal values and radiation load. Fortschr RoFo 1992; 157(3)245–251
- Passing H, Bablok W. A new biometrical procedure for testing the equality of measurements from two different analytical methods. Application of linear regression procedures for method comparison studies in clinical chemistry, Part 1. Clin Chem Clin Biochem 1983; 21: 709–720
- Krackow K A, Pepe C L, Galloway E J. A mathematical analysis of the effect of flexion and rotation on apparent varus/valgus alignment at the knee. Orthopedics 1990; 13(8)861–868
- Swanson K E, Stocks G W, Warren P D, Hazel M R, Janssen H F. Does axial limb rotation affect the alignment measurements in deformed limbs?. Clin Orthop 2000; 371: 246–252
- Cuoll R, Bankes MJK, Rossouw D J. Evaluation of tibial component angles in 79 consecutive total knee arthroplasties. Knee 1999; 6: 235–237
- Petersen T L, Engh G A. Radiographic assessment of knee alignment after total knee arthroplasty. J Arthroplasty 1988; 3(1)67–72
- Akagi M, Matsusue Y, Mata T, et al. Effect of rotational alignment on patella tracking in total knee arthroplasty. Clin Orthop 1999; 366: 155–163
- Poilvache P L, Insall J N, Scuderi G R. Font-Rodriguez, D.E. Rotational landmark and sizing of the distal femur in total knee arthroplasty using the epicondylar axis. Clin Orthop 1996; 331: 35–46
- Jenny J Y, Boeri C, Picard F, Leitner F. Reproducibility of intra-operative measurement of the mechanical axes of the lower limb during total knee replacement with a non- image-based navigation system. Comput Aided Surg 2004; 9(4)161–165
- Hauser R. Computer-aided 3D-navigation systems. A plea for an error model. HNO 2000; 2: 71–74
- Picard F, Leitner F, Raoult O, Saragaglia D. Computer assisted total knee arthroplasty. Rechnergestütze Verfahren in Orthopädie und Unfallchirurgie, J Jerosch, K Nicol, K Peikenkamp. Steinkopff, Darmstadt 1999; S 461–471