Abstract
Objective: Imageless computer assisted total knee surgical systems have commonly relied on determination of the functional rotational center of the femoral head as a landmark for determining the lower extremity mechanical axis. This has been accomplished through range of motion and center of rotation calculations for the femur with respect to the pelvis as the lower extremity is taken through a range of motion. Our study evaluated the use of this algorithm with and without a pelvic tracker attached to the iliac crest.
Materials and Methods: The functional center of the hip joint was also compared to the true radiographic center as determined by spiral CT data. Evaluating the different methods on six lower extremities from three whole-body cadavers revealed significant differences in the location of the calculated hip joint center, but little difference in the resulting lower extremity mechanical axis determination. The functional hip joint centers measured with and without a pelvic tracker differed from one another and from the CT-determined hip center.
Results: No differences were found in the coronal plane measurements, but statistically significant differences were found in the sagittal plane measurements.
Conclusion: Algorithms that reduce the noise generated by pelvic movement should be devised to eliminate the need for a pelvic tracker.
Introduction
An accurate determination of the hip joint center (HJC) is required in order to determine the mechanical axis and proper orientation of the femoral component during Total Knee Arthroplasty (TKA) Citation[1]. Intraoperative anatomical landmarks including the intramedullary femoral canal and the anterior superior iliac spine (ASIS) have been used to approximate the location of the HJC Citation[2]. Insertion of a straight rod through the intramedullary canal can be used to reflect the anatomical axis of the femur in order to approximate the mechanical axis. However, this approach may increase the risk of pulmonary embolism, postoperative hematoma, and even death Citation[3–6].
Computer navigation provides an alternative approach for identifying mechanical axis alignment during TKA Citation[7–10]. The HJC can be located using a functional method in which a sphere is best fitted to the motion path traced by passive movement of the femur. Accuracy of the functional method could be compromised by noise generated by pelvic movement as the femur is taken through the range of motion. This error may be minimized by insertion of a pelvic tracker into the iliac crest, thus subtracting any pelvic motion from the path traced by the femur. Using Roentgen stereophotogrammetric analysis (RSA) as a standard, the accuracy of the functional method employing markers applied to the thigh and using motion to approximate the HJC has been reported to be within 13 mm RMS value Citation[11]. Accuracy of HJC determination could be further increased by ranging the hip through an arc of at least 30° in the coronal and sagittal planes Citation[9]. Although this functional method is fairly accurate, the insertion of a pin into the iliac crest may increase surgical morbidity through infection, pain, and cutaneous nerve injury.
This study investigated whether the use of instantaneous center of hip motion data to determine the radiographic HJC had a significant effect on the determined lower extremity mechanical axis. The study also investigated whether eliminating the pelvic tracker in the iliac crest had a significant effect on hip center determination.
Materials and methods
Three fresh whole-body cadavers were used to determine the radiographic and functional HJC in six lower extremity limbs. To establish a common coordinate system between the CT scan and the navigation system, three pelvic, five femoral, three tibial and three ankle metallic fiducials were embedded in the cadaveric specimen for digitization and comparison with the computer navigation system (Stryker Navigation System, Stryker, Inc., Kalamazoo, MI). Pelvic markers were placed on the pubic tubercle, the anterior superior iliac spine (ASIS) and the ischial tuberosity. For the femur, markers were placed in the greater and lesser trochanter, and in the medial, lateral and anterior distal femoral metaphysis. The proximal tibial metaphysis had markers placed in the medial and lateral aspects, as well as on the tibial tubercle. The ankle had fiducial markers placed in the medial and lateral malleoli and the anterior aspect of the distal metaphysis of the tibia.
A spiral CT scan was then performed on each cadaveric specimen. Scan parameters included looking at the fiducial markers with 1.5mm slices and central digitization of the fiducials on custom-based CT-scan software (Stryker, Inc., Kalamazoo MI). The cadavers were then placed supine on an operating room table and an infrared pelvic tracker was firmly attached to the iliac crest using a 4.0mm threaded pin. A second infrared marker was firmly attached to the distal femur using a self-locking 4.0mm Steinman pin. A safety belt was placed over the lower torso of each cadaver to prevent excessive movement of the pelvis during hip range of motion data collection. The lower extremity was taken through the maximum arc of motion as allowed by soft tissue constraints and without violating the potential sterile field. The lower extremity was not raised above the level of the surgeon's shoulder or lowered below the level of the operating table. The arc of motion was never more than 45° in any clinical rotation. The HJC was calculated as the center of the arc that best fitted the path created by motion of the femoral tracker after 200 data points had been collected. Each lower extremity was ranged three times by six independent observers, and the HJC was recorded for each trial and then averaged for all trials. The six observers comprised three joint reconstructive attendings, one fellow, a PGY-2 resident and a PGY-1 resident. The pelvic tracker was then removed and the testing was repeated in an identical manner, with the pelvic tracker resting on a fixed table in the operating room.
Following laboratory testing, the spiral CT scan with fine cuts through the femoral head was analysed. A best-fit circle was digitized to fit the femoral head slice with the greatest diameter. The embedded fiducials in the pelvis and femur were digitized using the navigation system during the anatomic testing. These coordinates were then used to compare the CT scan and navigation system data in order to compare the true radiographic hip center to the functional HJC. The differences in HJC (x, y, z coordinates) using the functional algorithms with and without an attached pelvic tracker were compared to the CT data for each lower extremity. A scalar distance from the HJC was calculated by taking the square root of the x, y, z coordinate squares. The scalar distance from the calculated HJC to the true HJC as determined by CT was compared for pin-based and pinless algorithms. Changes in the anatomical alignment in the coronal and sagittal planes were determined for the functional algorithms with and without an attached pelvic tracker by registering the landmarks of the distal femur, proximal tibia, and ankle, as outlined by the manufacturer, and once again compared with the CT data.
A paired analysis of variance (ANOVA) was used to determine differences in the HJC and alignment for the algorithms with and without an attached pelvic tracker. Statistical significance was set at less than 0.05.
Results
Imageless computer assisted navigation determination of the HJC using the pelvic tracker algorithm resulted in mean x, y and z values that were close to the radiographic center determined with CT (). When the average differences between the centers determined with computer navigation using a pelvic tracker were compared to those determined from the CT scan, the x, y and z differences were calculated as − 0.81 ± 2.23 mm, − 0.11 ± 1.04 mm, and 0.73 ± 2.76 mm, respectively (). This resulted in a mean scalar distance of 3.31 ± 1.95 mm from the true HJC using the pelvic tracker algorithm (). When the pelvic tracker was not used, localization of the HJC increased the mean x, y and z differences to − 1.08 ± 2.64 mm, − 2.37 ± 2.55 mm, and 2.62 ± 7.40 mm, respectively. One should note that the z-axis is in the anteroposterior direction, thus affecting flexion and extension the most. The mean scalar distance from the true HJC was 7.5 ± 5.00 mm using the algorithm without a pelvic tracker. The mean scalar error for the location of the center of the femoral head without a pelvic tracker was greater (p < 0.01) than that for the algorithm with a tracker attached.
Figure 1. Scatter plots showing the resultant scalar distances from the true hip joint center with (a) and without (b) a pelvic tracker. Note the tighter grouping of data points and fewer outliers in the pelvic tracker plot (all axes are marked in mm).
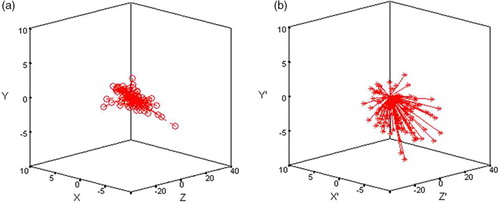
Table 1. Errors in the x-, y-, and z-directions associated with pin-based and pinless computer assisted HJC localization. δ is the scalar distance from the calculated HJC to the true center as determined by CT.
We found no inter-observer variation in measuring the HJC with either the pin-based or pinless methods. On average, there was less than 0.4° difference in alignment between observers for the algorithm with attached pelvic tracker.
Using the pelvic tracker algorithm, the observed error in HJC location would have resulted in a sagittal plane change in alignment of the mechanical axis by a mean 0.01° ± 0.15° in extension and a coronal plane change in alignment of 0.11° ± 0.32° in valgus. The associated sagittal change in alignment of the mechanical axis without use of the pelvic tracker was 0.33° ± 0.35° in extension, and the coronal plane change in alignment was 0.15° ± 0.35° in valgus (). The mean sagittal plane change alignment was greater (p < 0.0001) for the algorithm without a pelvic tracker than for the algorithm including the tracker. We found no differences in coronal plane alignment for the two algorithms tested.
Discussion
Infrared-based tracking systems provide accurate spatial measurements through the use of rigid-body transformations with errors reported on the order of 0.5° and 0.5 mm, depending on the clinical task Citation[12–15]. Although the infrared technology is accurate, intraoperative determination of lower extremity alignment relies on a multitude of calculations in an environment that is not always consistent or standardized. A large body habitus, hip joint incongruency secondary to osteoarthritis, dysplasia, or other pathology could introduce errors into an otherwise very accurate position tracking system. Pelvic motion during HJC localization is another source of potential error during computer assisted TKA. There have been other algorithms reported that lower the effects of motion when determining the center of the hip through range of motion data that can be used to minimize the effect on the resulting calculated joint center Citation[16], Citation[17]. Our current study demonstrated that insertion of a pelvic tracker improves the ability to determine the radiographic center of the hip, as determined by CT-scan measurements, by approximately 4 mm. However, these differences resulted in sagittal malalignment of the mechanical axis by only 0.3° in extension, with no statistically significant difference in the coronal plane alignment. Although the differences in sagittal alignment demonstrated statistical significance, the changes in component positioning that may result are difficult to determine.
The largest variations were found for the z-axis coordinate in the algorithm without the use of a pelvic tracker in the first cadaver tested. This cadaver was found to have the largest variation in the z-axis for each observer. This could represent a very small learning curve, since care was taken not to allow the pelvis to move during these trials. However, even with the belt around the torso of each specimen, motion of the pelvis could have occurred and therefore may have skewed the data. These results may indicate that when the system detects large variations or translation between data points, the hip center determination from range of motion data should be repeated. The current Stryker Navigation system would not allow an average HJC calculation to be used if significant motion or RMS value for the hip joint center was determined, and would ask the user to repeat the calculation.
Many arguments have arisen concerning the necessity for computer-based alignment techniques in TKA. One point of contention is whether the sagittal plane alignment correctly correlates with clinical terms. Using the center of the femoral head and the center of the distal femur as the neutral flexion axis may not be appropriate due to variations in the bow of the femur and anteversion of the femoral neck. The use of computer navigation in TKA has proven to decrease the outliers in the coronal plane Citation[18–20]. Intramedullary femoral and tibial alignment has also been shown to exhibit significant variation in the coronal and sagittal planes Citation[9], Citation[21]. While the long-term effects of significantly decreasing the number of outliers in alignment may not be determined for years to come, it is difficult to argue that this is a bad goal.
Our results proved to compare favorably with a report on HJC localization that used a similar functional method algorithm with reflective skin markers attached to the thigh and compared the results to RSA Citation[11]. The larger errors observed in the RSA study could be attributed to decreased accuracy of the RSA technique, as compared with CT, in determining the true HJC. One recent report suggests that accuracy of HJC localization could be improved through ranging the lower extremity in a multi-planar circumduction pattern with at least a 45° arc of motion and by calculating when translation of the rotation segment occurs Citation[9], Citation[17]. In our cadaver study and in clinical practice, we found that 45° of sagittal and coronal motion was within the tolerance of the hip soft tissue constraints, and could be performed without bringing the extremity outside the sterile field. Although the pin-based algorithm resulted in statistically improved accuracy and fewer outliers in the sagittal plane when compared with the pinless algorithm, these differences were small on average. The larger outliers in the location of the hip joint center without the use of a pelvic tracker are most likely attributable to pelvic motion. The data does prove, however, that center of rotation schemes for determining the HJC from range of motion data need a built-in “red flag” to be conveyed to the surgeon when large standard deviations or motion of the rigid body are detected. This study has shown that determination of the HJC using the functional center of hip rotation method may be achieved without the use of an attached pelvic tracker with these safeguards built in. Although the position of the HJC was determined to be significantly different, the coronal alignment change was not significantly affected. Surgeons should be aware of these possible differences and inquire about accuracy effects with whichever system they employ. It is important that surgeons are aware of the algorithms and subroutines of their system: as with any computer, if one is not aware of the appropriate inputs, the output data may be substantially affected.
Disclosure
Drs. Mihalko, Phillips and Krackow are consultants of Stryker Orthopaedics, Inc., and their institution has received funding from Stryker.
References
- Krackow K A. Total knee arthroplasty: technical planning and surgical aspects. Instr Course Lect 1986; 35: 272–282
- Seidel G K, Marchinda D M, Dijkers M, Soutas-Little R W. Hip joint center location from palpable bony landmarks - a cadaver study. J Biomech 1995; 28(8)995–998
- Bisla R S, Inglis A E, Lewis R J. Fat embolism following bilateral total knee replacement with the Guepar prosthesis. A case report. Clin Orthop 1976, 115: 195–198
- Caillouette J T, Anzel S H. Fat embolism syndrome following the intramedullary alignment guide in total knee arthroplasty. Clin Orthop 1990, 251: 198–199
- Dorr L D, Merkel C, Mellman M F, Klein I. Fat emboli in bilateral total knee arthroplasty. Predictive factors for neurologic manifestations. Clin Orthop 1989, 248: 112–118;, discussion 118–119
- Morawa L G, Manley M T, Edidin A A, Reilly D T. Transesophageal echocardiographic monitored events during total knee arthroplasty. Clin Orthop 1996, 331: 192–198
- Krackow K A, Phillips M J, Bayers-Thering M, Serpe L, Mihalko W. Computer-assisted total knee arthroplasty: navigation in TKA. Orthopedics 2003; 26(10)1017–1023
- Krackow K A, Bayers-Thering M, Phillips M J, Bayers-Thering M, Mihalko W M. A new technique for determining proper mechanical axis alignment during total knee arthroplasty: progress toward computer-assisted TKA. Orthopedics 1999; 22(7)698–702
- Piazza S J, Okita N, Cavanagh P R. Accuracy of the functional method of hip joint center location: effects of limited motion and varied implementation. J Biomech 2001; 34(7)967–973
- Stulberg S D, Loan P, Sarin V. Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am 2002; 84-(A(Suppl 2))90–98
- Leardini A, Cappozzo A, Catani F, Toksvig-Larsen S, Petitto A, Sforza V, Cassanelli G, Giannini S. Validation of a functional method for the estimation of hip joint centre location. J Biomech 1999; 32(1)99–103
- Casap N, Wexler A, Persky N, Schneider A, Lustmann J. Navigation surgery for dental implants: assessment of accuracy of the image guided implantology system. J Oral Maxillofac Surg 2004; 62(9 Suppl 2)116–119
- Hoffmann J, Westendorff C, Schneider M, Reinert S. Accuracy assessment of image-guided implant surgery: an experimental study. Int J Oral Maxillofac Implants 2005; 20(3)382–386
- Kothe R, Strauss J M, Deuretzbacher G, Hemmi T, Lorenzen M, Wiesner L. Computer navigation of parapedicular screw fixation in the thoracic spine: a cadaver study. Spine 2001; 26(21)E496–E501
- Krempien R, Hassfeld S, Kozak J, Tuemmler H P, Dauber S, Treiber M, Debus J, Harms W. Frameless image guidance improves accuracy in three-dimensional interstitial brachytherapy needle placement. Int J Radiat Oncol Biol Phys 2004; 60(5)1645–1651
- Marin F, Mannel H, Claes L, Dürselen L. Accurate determination of a joint rotation center based on the minimal amplitude point method. Comput Aided Surg 2003; 8(1)30–34
- Schwartz M H, Rozumalski A. A new method for estimating joint parameters from motion data. J Biomech 2005; 38(1)107–116
- Rauh M, Mihalko W M, Krackow K A. Optimizing alignment (chapter 22). Total Knee Arthroplasty – A Guide to Get Better Performance, J Bellemans, M D Ries, J Victor. Springer Medizin Verlag;, Berlin 2005
- Stockl B, Nogler M, Rosiek R, Fischer M, Krismer M, Kessler O. Navigation improves accuracy of rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 2004, 426: 180–186
- Mihalko W M, Clark L, Boyle J, Krackow K A. Differences in femoral intramedullary starting points for femoral component placement during TKA and comparison to computer aided surgery techniques. J Arthroplasty 2005; 20(1)25–28
- Mihalko W M, Krackow K A. Variability of intramedullary, extramedullary and computer navigation tibial alignment techniques for TKA. J Knee Surg 2006; 19(1)33–36