Abstract
The relationship between coronal knee laxity and the restraining properties of the collateral ligaments remains unknown. This study investigated correlations between the structural properties of the collateral ligaments and stress angles used in computer-assisted total knee arthroplasty (TKA), measured with an optically based navigation system. Ten fresh-frozen cadaveric knees (mean age: 81 ± 11 years) were dissected to leave the menisci, cruciate ligaments, posterior joint capsule and collateral ligaments. The resected femur and tibia were rigidly secured within a test system which permitted kinematic registration of the knee using a commercially available image-free navigation system. Frontal plane knee alignment and varus-valgus stress angles were acquired. The force applied during varus-valgus testing was quantified. Medial and lateral bone-collateral ligament-bone specimens were then prepared, mounted within a uni-axial materials testing machine, and extended to failure. Force and displacement data were used to calculate the principal structural properties of the ligaments. The mean varus laxity was 4 ± 1° and the mean valgus laxity was 4 ± 2°. The corresponding mean manual force applied was 10 ± 3 N and 11 ± 4 N, respectively. While measures of knee laxity were independent of the ultimate tensile strength and stiffness of the collateral ligaments, there was a significant correlation between the force applied during stress testing and the instantaneous stiffness of the medial (r = 0.91, p = 0.001) and lateral (r = 0.68, p = 0.04) collateral ligaments. These findings suggest that clinicians may perceive a rate of change of ligament stiffness as the end-point during assessment of collateral knee laxity.
Introduction
Total Knee Arthroplasty (TKA) has become the standard procedure for the management of degenerative joint disease, providing pain relief, correction of deformity, and restoration of function. However, its success depends on several factors, including patient selection, appropriate implant design, effective peri-operative care, and correct surgical technique [Citation1].
In particular, the importance of post-operative coronal alignment of the knee with regard to clinical outcomes has been well documented [Citation2–4]. More recently, however, it has been reported that alignment alone may not be an accurate predictor of implant function and longevity, but rather that a combination of accurate alignment and soft tissue balancing is required to optimize the clinical outcome [Citation5, Citation6].
In knees with large varus and valgus deformities, the soft tissue structures have often contracted, meaning that it is not possible to achieve a neutral alignment through bone cuts alone [Citation7]. Functionally, the medial collateral ligament (MCL), particularly its superficial portion, acts as the primary restraint to valgus angulation, and the lateral collateral ligament (LCL) serves as the primary restraint to varus angulation [Citation8, Citation9]. Therefore, the collateral ligaments may be moderately or extensively released in order to achieve a well-balanced joint [Citation10]. Soft tissues should be balanced in both flexion and extension and tensioned sufficiently to produce stability, but without limiting the range of movement [Citation6]. Conventionally, the technique has involved a subjective assessment of laxity [Citation11], but with increasing patient expectations and greater mechanical demands being placed on the prostheses [Citation12], quantitative assessment may be required.
Computer navigation systems have been introduced into TKA surgery [Citation13–15], and the use of computer-assisted surgery has been associated with better clinical outcomes when compared to conventional techniques [Citation16–21]. Several studies have demonstrated independently that these systems improve the accuracy of both component placement and alignment [Citation22–27]. However, they are also particularly useful for the intra-operative measurement of passive kinematic joint characteristics, as they can provide accurate assessment of coronal knee laxity [Citation28], and can be used to ensure that the quantified joint laxity is acceptable [Citation29].
Navigation-based measures of varus and valgus stress angles have been used to define a number of algorithms for management of soft tissue in TKA [Citation29–33]. This provides an objective assessment of laxity which, in turn, will allow for more precise soft tissue balancing. However, the extent to which such navigation-derived stress angles reflect the restraining properties of the collateral ligaments of the knee remains unknown. The aim of this study was to assess the relationship between traditional measures of the structural properties of the collateral ligaments of cadaver knees and the stress angles measured with an optically based navigation system. It would be expected that these ligaments, as major stabilizing structures of the knee, would have a significant role in resisting the moments applied in measuring stress angles. Therefore, the hypothesis was that a relationship would exist between the structural properties of the collateral ligaments and the coronal laxity of the knee.
Materials and methods
Specimens
This study received Institutional Review Board approval. Dissections were performed on 10 fresh-frozen human cadaver knees (nine left and one right) obtained from five male and five female donors of mean age 81 years (range: 62–92 years). All knees were free of gross musculoskeletal trauma and pathology and had been resected approximately 10 cm either side of the joint line. The dissection technique was developed using methods described previously [Citation34]. The collateral ligaments, cruciate ligaments, menisci and posterior capsule were retained in order to retain structural stability of the knee. All other remaining soft tissues of the femur, tibia and fibula were removed.
Assessment of knee laxity using computer navigation system
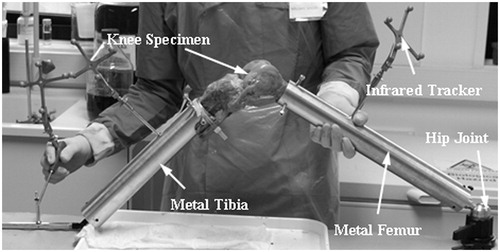
As the specimens were resected 10 cm proximal and distal to the knee joint line, a custom-made aluminum replica of the lower limb was manufactured. The dimensions of the femoral and tibiofibular-foot components were based on average segment lengths reported in the literature [Citation35]. The resected femoral and tibial shafts were rigidly secured within the femoral and tibiofibular components, respectively (). The model allowed kinematic registration of the knee using the standard workflow of a commercially available image-free navigation system [Citation15, Citation36]. Data were collected using the OrthoPilot® CT-free navigation system (Aesculap/B. Braun, Tuttlingen, Germany), which in this study was used solely as a measuring device. Two passive infrared trackers were affixed, one to the femoral component and one to the tibiofibular component, and the workflow was followed until the monitor screen displayed the coronal and sagittal femorotibial angle (FTA). The knee was placed in extension and the coronal mechanical FTA recorded using the navigation system. A varus and valgus stress force was then applied at the ankle with the knee joint held at 3° flexion. Force was applied manually at the distal end of the tibiofibular component using the right hand of the principle investigator, while the left hand was used to stabilize the knee joint. The force applied was a subjective evaluation of the force required to reach a perceived “end-point”. The maximum coronal FTA attained during varus and valgus stress testing was recorded, and the magnitude of the force was quantified with a dynamometer attached to the distal tibial shaft. Varus and valgus stress testing was repeated three times. Knee laxity was calculated as the average peak angle, in degrees, by which the knee deviated from its initial coronal plane alignment during application of varus and valgus stress force.
Mechanical testing of collateral ligaments
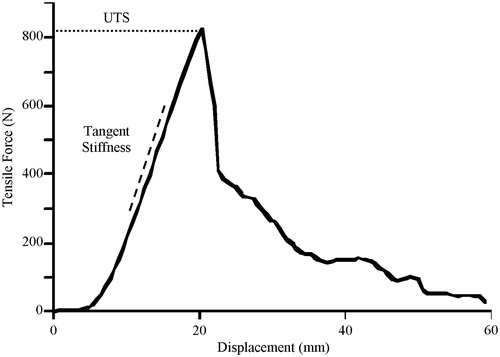
Following assessment of knee laxity, specimens were prepared for mechanical testing of the structural properties of the collateral ligaments. The methodology for this has been described in detail elsewhere [Citation34]. In brief, the specimen was sectioned sagittally and remnants of the cruciate ligaments, posterior capsule and any other remaining tissue were dissected free to leave two bone-collateral ligament-bone specimens (). Each specimen was then secured in a uni-axial materials testing machine and, following 10 preconditioning cycles (3.5% strain at 1 Hz), extended to failure at a rate of 500 mm min−1. Force and displacement data were used to calculate the ultimate tensile strength and stiffness of the two ligaments. Ultimate tensile strength was defined as the maximum force reached during testing. Stiffness was derived via two methods. A traditional measure of ligament stiffness (tangent stiffness) was determined for each ligament by calculating the gradient of the linear section of the force-displacement curve (). In addition, instantaneous stiffness of each ligament was estimated at forces corresponding to the peak moment applied manually to the knee during the clinical laxity testing. Instantaneous stiffness was calculated by determining analytically the first-order derivative of polynomial functions fit to the force-displacement data [Citation37].
Figure 2. A bone-ligament-bone preparation mounted in the tensile testing apparatus. (1) Femur; (2) Lateral collateral ligament; (3) Fibula.
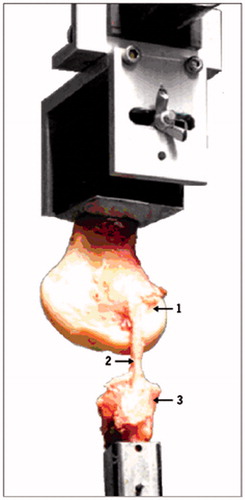
Figure 3. Tangent stiffness and ultimate tensile strength parameters derived from a typical force-displacement curve for the MCL. Tangent stiffness was defined by the slope of the linear section of the force-displacement curve (offset for illustrative purposes), while ultimate tensile strength was defined as the peak force during failure testing. Note that the force applied during manual laxity testing (N) lies within the “toe” region of the force-displacement curve, and is well below the tensile strain at which structural properties are typically calculated.
Statistics
Statistical analysis was carried out using the Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL). Paired t-tests were used to compare normally distributed variables (varus and valgus stress angles, force applied during stress testing). Pearson’s correlations were used to investigate potential relationships between dependent variables. For all tests, significance was assessed at an alpha level of 0.05.
Results
The MCL and LCL were found to be well-defined structures on dissection and free of obvious musculoskeletal pathology. One of the 10 specimens failed via fracture of the femur during mechanical testing, and consequently was excluded from the study, giving a total of 9 knees for subsequent analysis.
Assessment of knee laxity
The median coronal alignment of the knees in extension was 2° valgus, and ranged between 3° varus and 8° valgus. Six of the 9 knees were valgus (FTA > 0°), one was varus (FTA < 0°), and two were neutrally aligned (FTA = 0°). The mean varus laxity for the 9 knees was 4 ± 1° (range: 3–6°), while the mean valgus laxity was 4 ± 2° (range: 2–8°) ().
Table I. Mean (± SD) knee joint laxity, manually applied force, and structural properties of the MCL and LCL for each specimen.
The mean force applied during all laxity tests was 10 ± 3 N. There was no statistically significant difference between the force applied in either direction during varus and valgus laxity testing (p = 0.17). Similarly, there was no significant correlation between the force applied during laxity testing and the resultant angular deviation in a varus (r = 0.24) or valgus (r = 0.13) direction.
Collateral ligament properties
The principal structural properties of the collateral ligaments are shown in [34]. While the ultimate tensile strength of the MCL was significantly greater than that of the LCL (p < 0.001), there was no statistically significant difference in the tangent stiffness or instantaneous stiffness of the two ligaments at forces equivalent to those applied during laxity testing.
Measures of varus and valgus laxity were not significantly correlated with the tangent stiffness or ultimate tensile strength of the collateral ligaments (). However, there was a significant correlation between the force applied during stress testing and the instantaneous stiffness of the medial (r = 0.92, p = 0.001) and lateral (r = 0.69, p = 0.04) collateral ligaments ().
Figure 4. Correlation between applied force and ligament instantaneous stiffness at that force for valgus/MCL and varus/LCL tests.
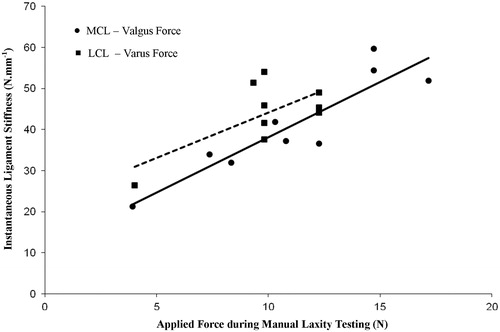
Table II. Correlation coefficients and corresponding p-values between measures of varus and valgus knee laxity and the principal structural properties of the corresponding ligament.
Discussion
This study tested the hypothesis that the mechanical properties of the collateral ligaments of the knee would govern varus and valgus stress angles measured with the aid of an optically based navigation system. Contrary to our hypothesis, we found that the magnitude of stress angles was correlated neither with the force applied during laxity testing nor the structural properties of the restraining collateral ligaments. As shown in , the magnitude of the force applied during clinical laxity testing was small (10 N) and well below that of forces used to determine the key structural properties of ligaments (i.e., the linear section of the force-displacement curve, >200 N). Thus, clinical tests of knee laxity do not give an indication of the true elastic or restraining properties of the collateral ligaments.
While it may be argued that measures of laxity reflect the low-stress behavior of the ligaments, equivalent to the so-called “toe region” of the force-displacement curve, angular deviation was also unrelated to the instantaneous stiffness of the collateral ligaments at forces equivalent to those applied during laxity testing. Thus, varus and valgus stress angles of the knee may be influenced by deformation of other soft tissue structures, and some variable degree of laxity may be possible without eliciting strain on the collateral ligaments.
Although varus and valgus stress angles were unrelated to the applied force or restraining properties of the collateral ligaments, the force applied during manual laxity testing was correlated significantly with the instantaneous stiffness of the two ligaments. We therefore hypothesize that, during manual testing, the operator may have sensed a change in the stiffness of these ligaments as the perceived end-point of the movement. Speculatively, this perception may be surgeon-specific and may explain previous reports of large inter-surgeon variation when assessing laxity in vivo using a non-invasive navigation system [Citation38]. Therefore, further research evaluating factors related to the determination of a perceived end-point of clinical laxity testing appears warranted.
The mean force applied during clinical laxity testing in this study (10 N) is considerably lower than the values reported elsewhere for examination of the joint in vivo [Citation39]. This would be expected, due to the resistance provided by active structures and other anatomical restraints which were removed from our specimens. A clinical examination of knee laxity on a patient is an attempt to isolate and test only the passive restraints provided by the ligaments and joint geometry, not the active restraints or joint compressive forces. Such isolation is not possible in vivo, so only a limited evaluation of the ligaments that provide joint stability is possible by the clinical laxity tests [Citation40].
This study has a number of limitations which should be considered when interpreting the results. Measurements of initial coronal alignment are a result of the test set-up, which does not perfectly recreate the natural anatomy of the lower limb. Hence, initial alignment is used solely as a neutral reference point for subsequent determination of laxity. Furthermore, this study focused on individual structures and is therefore not a true representation of knee behavior in vivo. While we have chosen to focus on the primary ligamentous stabilizers of the extended knee during coronal laxity testing, other structures undoubtedly act as secondary restraints [Citation8]. Thus, the experiment represents an idealized version of the in vivo condition, and further study would be required to investigate the relationships between laxity and the properties of the other stabilizing structures. Also, all laxity tests in this study were carried out with the knee joint held in three degrees of flexion, but there is evidence to suggest that measurements of laxity change with flexion of the knee [Citation28]. Therefore, further work is required to assess any potential influences of laxity over a range of knee flexion angles.
Nonetheless, the findings of the present study suggest that angular deviation of the knee during varus and valgus laxity testing is not related to traditional structural properties of the restraining collateral ligaments. However, the force applied by operators during clinical testing, although low, is correlated positively to the instantaneous stiffness of the ligament, suggesting that operators may perceive a change in the low-stress behavior of these ligaments.
Conclusion
The findings of the current study suggest that clinically assessed knee laxity is independent of traditional measures of structural properties of the collateral ligaments. However, the force applied during manual stress testing of the knee was correlated with the instantaneous stiffness of the collateral ligaments. Therefore, clinicians may perceive an “end-point” based on the low-stress behavior of these ligaments, particularly a rate of change of stiffness. Further work is required to understand the relationships between applied force and resultant stress angles, and how this relates to clinical outcomes for TKA. This and other useful applications of this evolving technology continue to increase the relevance of the quantitative data afforded by current navigation systems.
Declaration of interest
Dr. Wearing is funded through a Smart Futures Fellowship from the Department of Employment, Economic Development and Innovation, Queensland Government. The authors report no declarations of interest.
Acknowledgment
The authors wish to thank Mr D.J.A. Smith for his technical assistance.
Notes
*Prior presentations relating to this study were given at the 12th Meeting of the Combined Orthopaedic Associations, Glasgow, 12–17 September 2010; the 10th Annual Meeting of the International Society for Computer Assisted Orthopaedic Surgery (CAOS-International), Paris, 16–19 June 2010; and the 4th Annual Conference of the British Society for Computer Assisted Orthopaedic Surgery (CAOS-UK), London, 27–29 November 2009.
References
- Coytes PC. 1999. Revision knee placement in Ontario, Canada. J Bone Joint Surg 81A:773–82
- Feng EL, Stulberg SD, Wixson RL. 1994. Progressive subluxation and polyethylene wear in total knee replacements with flat articular surfaces. Clin Orthop Relat Res 299:60–71
- Jeffery RS, Morris RW, Denham RA. 1991. Coronal alignment after total knee replacement. J Bone Joint Surg 73B:709–14
- Sharkey PF, Hozack WJ, Rothman RH, et al. 2002. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13
- Parratte S, Pagnano MW, Trousdale RT, Berry DJ. 2010. Effect of postoperative mechanical axis alignment on the fifteen year survival of modern, cemented total knee replacements. J Bone Joint Surg 92A:2143–9
- Sikorski JM. 2008. Alignment in total knee replacement. J Bone Joint Surg 90B:1121–7
- Whiteside LA. 2002. Soft tissue balancing: the knee. J Arthroplasty 17:23–7
- Grood ES, Noyes FR, Butler DL, Suntay WJ. 1981. Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees. J Bone Joint Surg 63A:1257–69
- Markolf KL, Mensch JS, Amstutz HC. 1976. Stiffness and laxity of the knee – the contributions of the supporting structures. A quantitative in vitro study. J Bone Joint Surg 58A:583–94
- Engh GA. 2003. The difficult knee: severe varus and valgus. Clin Orthop Relat Res 416:58–63
- Van Damme G, Defoort K, Ducoulombier Y, et al. 2005. What should the surgeon aim for when performing computer-assisted total knee arthroplasty? J Bone Joint Surg 87A:52–8
- Nilsdotter AK, Toksvig-Larsen S, Roos EM. 2009. Knee arthroplasty: are patients’ expectations fulfilled? A prospective study of pain and function in 102 patients with 5-year follow-up. Acta Orthop 80:55–61
- Delp SL, Stulberg SD, Davies B, et al. 1998. Computer assisted knee replacement. Clin Orthop Relat Res 354:49–56
- Matsen FA, Garbini JL, Sidles JA, et al. 1993. Robotic assistance in orthopaedic surgery. A proof of principle using distal femoral arthroplasty. Clin Orthop Relat Res 296:178–86
- Stulberg SD, Picard F, Saragaglia D. 2000. Computer-assisted total knee arthroplasty. Oper Tech Orthop 10:25–39
- Choong PF, Dowsey MM, Stoney JD. 2009. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty 24:560–69
- Kluge WH. 2007. Mini-symposium: Computer-assisted surgery in orthopaedics (iv): Computer-assisted knee replacement techniques. Curr Orthopaed 21:200–6
- Longstaff LM, Sloan K, Stamp N, et al. 2009. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty 24:570–8
- Lüring C, Oczipka F, Perlick L, et al. 2009. Two year follow-up comparing computer assisted versus freehand TKR on joint stability, muscular function and patients satisfaction. Knee Surg Sports Traumatol Arthrosc 17:228–32
- Tingart M, Lüring C, Bäthis H, et al. 2008. Computer-assisted total knee arthroplasty versus the conventional technique: how precise is navigation in clinical routine? Knee Surg Sports Traumatol Arthrosc 16:44–50
- Tokuhara Y, Nakagawa S, Kobayashi A, et al. 2004. The flexion gap in normal knees; an MRI study. J Bone Joint Surg 86B:1133–6
- Bäthis H, Perlick L, Tingart M, et al. 2004. Alignment in total knee arthroplasty. A comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg 86B:682–7
- Chauhan SK, Scott RG, Breidahl W, Beaver RJ. 2004. Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. J Bone Joint Surg 86B:372–7
- Jenny J, Boeri C. 2001. Computer-assisted implantation of total knee prostheses: A case-control comparative study with classical instrumentation. Comput Aided Surg 6:217–20
- Matziolis G, Krocker D, Weiss U, et al. 2007. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg 89A:236–43
- Sparman M, Wolke B, Czupalla H, et al. 2003. Positioning of total knee arthroplasty with and without navigation support: a prospective, randomised study. J Bone Joint Surg 85B:830–5
- Victor J, Hoste D. 2004. Image-based computer-assisted total knee arthroplasty leads to lower variability in coronal alignment. Clin Orthop Relat Res 428:131–9
- Jenny J-Y. 2010. Coronal plane knee laxity measurement: Is computer-assisted navigation useful? Orthop Traumatol Surg Res 96:583–8
- Picard F, Deakin AH, Clarke JV, et al. 2007. A quantitative method of effective soft tissue management for varus knees in total knee replacement surgery using navigational techniques. Proc Inst Mech Eng H 221:763–72
- Hakki S, Coleman S, Saleh K, et al. 2009. Navigational predictors in determining the necessity for collateral ligament release in total knee replacement. J Bone Joint Surg 91B:1178–82
- Luring C, Hüfner T, Perlick L, et al. 2006. The effectiveness of sequential medial soft tissue release on coronal alignment in total knee arthroplasty: using a computer navigation model. J Arthroplasty 21:428–34
- Luring C, Oczipka F, Grifka J, Perlick L. 2008. The computer-assisted sequential lateral soft-tissue release in total knee arthroplasty for valgus knees. Int Orthop 32:229–35
- Saragaglia D, Chaussard C, Rubens-Duval B. 2006. Navigation as a predictor of soft tissue release during 90 cases of computer-assisted total knee arthroplasty. Orthopedics 29:137–8
- Wilson WT, Deakin AH, Payne AW, et al. 2012. Comparative analysis of the structural properties of the collateral ligaments of the human knee. J Orthop Sports Phys Ther 42:345–51
- Winter DA. 1990. Biomechanics and Motor Control of Human Movement. 2nd ed. New York: John Wiley & Sons. pp 51–74
- Stulberg SD, Loan P, Sarin V. 2002. Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg 84A:90–8
- Maitland ME, Bell GD, Mohtadi NG, Herzog W. 1995. Quantitative analysis of anterior cruciate ligament instability. Clin Biomech 10:93–7
- Clarke JV, Riches PE, Picard F, Deakin AH. 2012. Non-invasive computer-assisted measurement of knee alignment. Comput Aided Surg 17:29–39
- Clarke JV, Wilson WT, Wearing SC, et al. 2012. Standardising the clinical assessment of coronal knee laxity. Proc Inst Mech Eng H 226:699–708
- Noyes FR, Grood ES, Butler DL, Raterman L. 1980. Knee ligament tests: what do they really mean? Phys Ther 60:1578–81