Abstract
Objective: The objectives of this study were to evaluate the accuracy of computed tomography (CT)-based navigation and to investigate whether the level of surgeon experience affects the accuracy of cup positioning under navigation.
Methods: This study investigated 117 hips in 103 patients who underwent primary total hip arthroplasty (THA) by 7 surgeons using a CT-based navigation system. Pre- and postoperative CT images were matched using a volume registration technique. Postoperative cup angles and positions were then measured using the same pelvic coordinates, and results were compared for experienced and inexperienced surgeons.
Results: The mean absolute error of the cup angle was 1.8 ± 1.6° for inclination and 1.2 ± 1.1° for anteversion. The mean absolute errors of cup position were 1.9 ± 1.5 mm, 1.4 ± 1.2 mm, and 1.9 ± 1.3 mm on the x-, y- and z-axes, respectively. No significant differences in accuracy were identified between experienced and inexperienced surgeons.
Conclusions: The absolute spatial error of cup position was ≤2 mm for each axis, and the angle error was ≤2° for the angles of inclination and anteversion. This navigation system could therefore help surgeons perform accurate cup placement irrespective of the surgeon’s level of experience.
Introduction
In total hip arthroplasty (THA), the orientation of the acetabular cup is an important factor in preventing postoperative complications such as dislocation, accelerated wear and loosening [Citation1–3]. The level of experience of the surgeon has been suggested as one of the most important factors affecting rates of dislocation [Citation4–6] and revision [Citation7, Citation8]. However, variations in pelvic position on the operating table make the conventional technique using mechanical instruments inaccurate in terms of cup orientation [Citation4–6], even when performed by experienced surgeons [Citation9].
To address these issues, computer navigation has been introduced, in which the positions of the pelvis and instruments are tracked in real time. Computed tomography (CT)-based navigation is the most accurate of the various types of navigation currently available, and several reports have described clinical outcomes in terms of the precision of the cup angle achieved with CT-based navigation systems [Citation5, Citation10, Citation11]. However, there have been no reports describing the usefulness of such navigation systems to inexperienced surgeons. These systems may assist inexperienced surgeons in correct placement of the acetabular cup [Citation12], but may also result in more complicated operations and may not lead to good results.
On the other hand, a few reports have detailed the accuracy of measurements obtained using CT-based navigation, representing the difference between the values for cup placement position and angle recorded from navigation and those measured postoperatively. To evaluate the accuracy of measurements with CT-based navigation, cup placement visualized on postoperative CT should be compared with that recorded on preoperative CT using the same pelvic coordinates. Measurements of cup position and orientation are markedly influenced by the pelvic coordinates, and matching coordinates of the pelvis between two different CT image data sets from the same patient with the same anatomic landmarks is not sufficiently accurate [Citation13]. To accurately match positions of the pelvis between two CT image data sets, volume registration is an appropriate technique [Citation14, Citation15].
The objectives of this study were to evaluate the accuracy of cup placement measurements and to investigate whether the level of surgical experience affected the accuracy of cup placement with CT-based navigation.
Methods
Patients
From January 2007 to June 2008, a total of 136 hips in 120 patients underwent THA at Kyowakai Hospital, Osaka, using a CT-based navigation system (Stryker CT-Hip System V1.0-29, Stryker-Leibinger, Freiberg, Germany) and the same acetabular component (Trident, Stryker Orthopaedics, Mahwah, NJ). Seven patients (7 hips) who did not undergo postoperative CT were excluded from the study. Also excluded were 11 patients (12 hips) in whom dome screws were used. The remaining 117 hips in 103 patients were included in the study. All operations were performed by 7 surgeons: 3 senior surgeons (experienced surgeons), and 4 resident surgeons (inexperienced surgeons).
The mean age of the 103 patients (21 men, 82 women) was 60 years (range: 41–85 years). The right hip was affected in 46 patients, the left in 43 patients, and both hips in 14 patients. Mean body mass index (BMI) of the patients was 24 (range: 17–39; standard deviation: 4.6). The underlying pathology was osteoarthritis in 108 hips (secondary to hip dysplasia in 104 cases [96.3%]), avascular necrosis of the femoral head in 3 hips, rheumatoid arthritis in 4 hips, and rapidly destructive coxopathy in 2 hips (). Although a significant difference was apparent in preoperative diagnoses, the frequency of osteoarthritis, which accounted for the majority of cases, was almost the same in the two groups.
Table I. Patient demographic data.
All study protocols were approved by our institutional review board and informed consent was obtained from each patient.
Operative procedure using the CT-based navigation system
Preoperative planning. Preoperative CT images were obtained using a helical CT scanner (HiSpeed Advantage, GE Medical Systems, Milwaukee, WI) from the level of the anterior superior iliac spine (ASIS) to the femoral condyle. Imaging settings were as follows: resolution 512 × 512 pixels; field of view (FOV) 360 × 360 mm; slice thickness 1 mm; and pitch 3 mm. CT images in DICOM format were transferred to the navigation planning station. Pelvic coordinates were determined by pinpointing eight landmarks, including the bilateral ASIS, pubic tubercles and ischia, the pubic symphysis, and the sacral midplane. Cup size and position were determined with reference to the anteroposterior width of the acetabulum, bony coverage [Citation16], limb length, and stem anteversion [Citation17] (). Cup anteversion was based on stem anteversion, set at 10° increments [Citation18] while maintaining the radiographic inclination of the cup at 40° to avoid edge loading and excessive wear [Citation1, Citation19–21] ().
Preparation. All operations were performed with the patient in the lateral decubitus position using a posterolateral approach. Two φ 4-mm apex pins (Stryker Trauma AG, Selzach, Switzerland) were inserted into the pelvic brim percutaneously through stab incisions. The active marker tracker was then firmly connected to the apex pins with Hoffman II clamps (Stryker Trauma AG). The position of the infrared sensor camera array was adjusted toward the center of the perception range of the surgical field.
Registration. After resection of the femoral head and acetabular exposure, initial paired-point matching registration was performed by digitizing the four bony landmarks. Surface match registration was then performed by digitizing 30 points on the pelvic surface [Citation22]. When the root mean square (RMS) deviation between the surface model and digitized points was ≤1 mm and the digitized points were >80% utilized, the reliability of surface matching was verified by touching at least six characteristic points (the ASIS, the anterior, superior and posterior rims of the acetabulum, the ischial notch, and the acetabular fossa). If this verification was not accepted, the registration procedure was repeated until acceptable verification was obtained. To confirm that the trackers had not become loosened during the procedure, a verification point was recorded on the bone surface of the posterior column of the acetabulum after successful registration. This point was used to measure relative movement of the trackers and pelvis after registration. After press-fit fixation of the cup, the cup angles and spatial position were recorded and the verification point was digitized. When the point deviation was <2 mm, we defined the tracker as having no movement from the registration time and the navigation record of cup placement was judged to be reliable.
Figure 1. A cup planning model on the workstation. Cup angles and spatial position can be planned on a 3D pelvic model. Cup size was determined by referring to the anteroposterior width of the acetabulum, and inclination and anteversion were adjusted according to the stem anteversion angle needed to acquire the best range of motion. Finally, leg length was adjusted by changing the stem size and neck offset length.
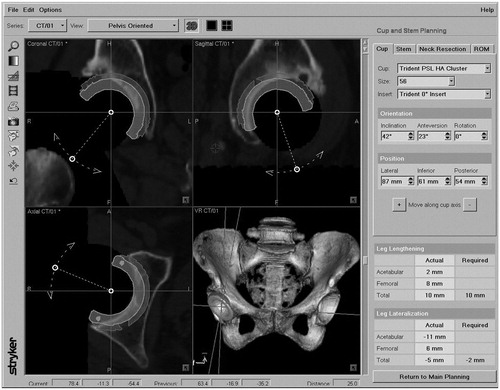
Table II. Target angles for the cup (radiographic definition).
Postoperative measurement of cup position
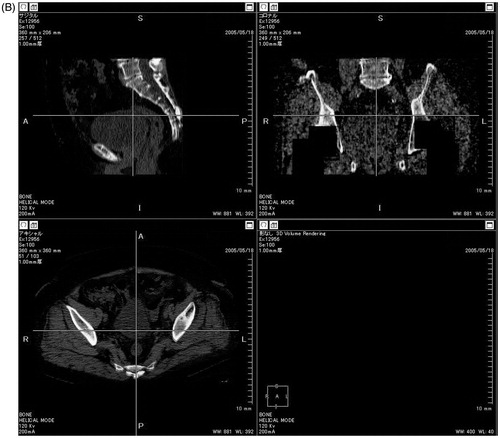
Volume registration technique. All 103 patients (117 hips) included in this study underwent pelvic CT at 3–4 weeks postoperatively. To match the position of the pelvis on pre- and postoperative CT images, we used a volume registration technique with three-dimensional (3D) viewer software (Virtual Place, Medical Image Laboratory, Tokyo, Japan) [Citation14, Citation15]. After carrying out 3D reconstruction of pre- and postoperative CT data, it was possible to establish a direct relationship between images by overlapping them semi-automatically (). The reproducibility of this method has been reported as 0.7° and 0.8 mm [Citation23].
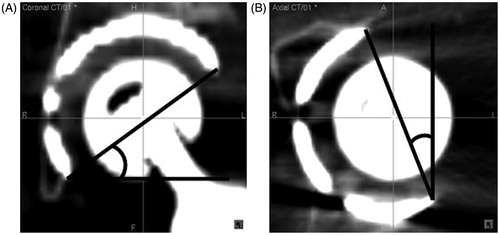
Angle measurement. After pelvic coordination of postoperative CT images, we measured the postoperative acetabular component position in the coronal and axial views using image-processing software (Scion Image, Scion, Frederick, MD) on multiplanar reconstructed views of the pelvis. The radiographic angle of inclination was measured on the coronal reconstructed view, and the anatomical angle of anteversion was measured on the axial reconstructed view (). Anatomical anteversion was converted to radiographic anteversion using a formula for a trigonometric function with radiographic inclination. To clarify inter- and intra-observer errors in this measurement method, cup angles were measured three times by two of the authors, and correlation coefficients and mean values were obtained. The measured values were then compared with those recorded by the navigation system. The difference between the postoperative measurement and the intraoperative record indicates the accuracy of measurements by CT-based navigation.
Spatial position measurement. On the navigation software, a virtual cup was placed at the position of the actual cup on postoperative CT images. Differences in spatial position for each axis (the x-[transverse] axis, y-[sagittal] axis, and z-[longitudinal] axis for each CT slice) were then measured using intraoperative navigation data and postoperative CT at the same pelvic reference using a volume registration technique.
Figure 2. Pre- and postoperative CT reconstruction views (white arrows) were interposed automatically using 3D viewer software. (A) Before interposition. (B) After interposition. This procedure can change the postoperative pelvic position into the planned pelvic coordinates.
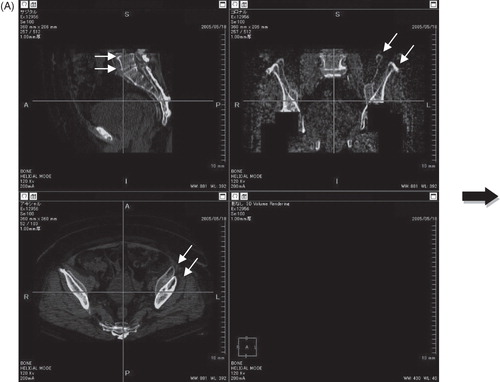
Figure 3. Postoperative measurement of the acetabular component position using image-processing software. The radiographic abduction angle was measured on the coronal view (A) and the anatomic anteversion angle was measured on the axial reconstruction view (B) at the same references used in planning.
Comparison between experienced and inexperienced surgeons
Seventy-eight THAs were performed by senior surgeons (experienced surgeons), who were performing approximately 50 THAs annually. The remaining 39 THAs were performed by resident surgeons (inexperienced surgeons), who were performing approximately 10 THAs annually. Profiles of the surgeons are shown in . To investigate whether the level of experience affected the accuracy of cup placement using this navigation system, we compared results related to cup orientation and the rate of intraoperative tracker loosening failure (deviation of verification >2 mm) for experienced and inexperienced surgeons.
Table III. Profiles of experienced and inexperienced surgeons.
Statistical analysis
The two groups (experienced vs. inexperienced) were compared using the t-test for the difference between the postoperative measurements and the intraoperative record, and Fisher’s exact test for gender, side, BMI, diagnosis, and the success rate of the registration point check. The Pearson correlation coefficient test was used to determine inter- and intra-observer correlations. All tests were considered statistically significant for values of p < 0.05.
Results
The intra-observer error for cup orientation was 0.26° (SD 0.40°) for inclination and 1.03° (SD 0.88°) for anteversion. Correlation coefficients were 0.97 for inclination and 0.93 for anteversion. The inter-observer error was 0.69° (SD 0.96°) for inclination and 0.53° (SD 1.47°) for anteversion. Correlation coefficients were 0.89 for inclination and 0.82 for anteversion.
Overall, the verification point check for the 117 hips was <2 mm in 87 hips (74%). Success was obtained for 59 hips (76%) by experienced surgeons and for 28 hips (72%) by inexperienced surgeons. No significant difference was apparent between the two groups (p = 0.84).
The overall difference between the postoperative measurement and the intraoperative record of cup angles in those cases in which the verification check was <2 mm (87 hips) was 0.5 ± 2.3° for inclination and −0.3 ± 1.6° for anteversion (). Between inclination and anteversion, no significant differences were identified in error or dispersion (inclination: p = 0.98; anteversion: p = 0.39). The mean spatial position error was 1.9 ± 1.5 mm on the x-axis, 1.4 ± 1.2 mm on the y-axis, and 1.9 ± 1.3 mm on the z-axis ().
Table IV. Difference in postoperative measurement from the intraoperative record of cup angle in cases for which the verification check was successful (87 hips).
With respect to the level of surgical experience, the mean difference between the postoperative measurement and the intraoperative record of cup angle was 0.5 ± 2.7° for inclination and −0.6 ± 1.3° for anteversion for inexperienced surgeons, and 0.5 ± 2.1° for inclination and −0.2 ± 1.7° for anteversion for experienced surgeons. No significant differences were identified between groups for angles (inclination: p = 0.98; anteversion: p = 0.39) ( and ), and 97% of cases were within ± 4.0°. The mean error of spatial position was 1.6 ± 1.2 mm on the x-axis, 1.3 ± 1.0 mm on the y-axis, and 1.7 ± 0.8 mm on the z-axis for inexperienced surgeons, and 2.0 ± 1.6 mm on the x-axis, 1.5 ± 1.3 mm on the y-axis, and 2.0 ± 1.5 mm on the z-axis for experienced surgeons. No significant differences were apparent between the two groups in spatial positioning (x-axis: p = 0.61; y-axis: p = 0.17; z-axis: p = 0.56) ( and ).
Figure 4. Box-plots showing the difference in postoperative measurement from the intraoperative record for the angles of abduction and anteversion for the cup. Box length represents the interquartile range (first to third quartiles). Lines within the boxes represent the median value. No significant differences were identified between experienced and inexperienced surgeons.
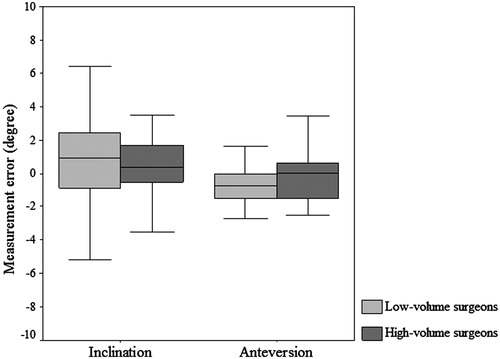
Figure 5. Box-plots showing differences in postoperative measurement from the intraoperative record for spatial position of the cup. No significant differences were apparent between the two groups.
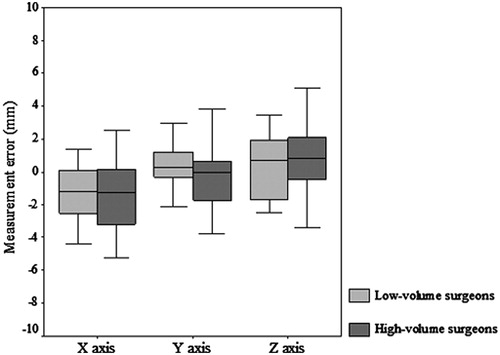
Table V. Mean spatial position error in cases in which the verification check was successful (87 hips).
Discussion
The present study showed quite a high level of accuracy for cup placement measurements using this CT-based navigation system, such as ≤2° for the mean error of absolute angle (1.8° for inclination; 1.2° for anteversion) and ≤2 mm for the mean error of absolute position (1.9 mm on the x-axis; 1.4 mm on the y-axis; and 1.9 mm on the z-axis). Furthermore, no significant differences in the accuracy of measurements were seen according to the level of surgical experience.
In THA, rates of dislocation [Citation4–6, Citation24] and revision [Citation7, Citation8] are reportedly lower for experienced surgeons than for inexperienced surgeons. Though it is obvious that the cause of these complications is multi-factorial, cup positioning using the navigation system may improve these rates even in the case of inexperienced surgeons. With inexperienced surgeons, however, navigation systems may result in more complicated operations and may not lead to a good result.
Thorey et al. [Citation25] reported that navigation may lead to a reduction in the length of the learning curve, improve the surgeon’s ability, and minimize outliers for inexperienced surgeons. However, whether navigation is useful in achieving precise placement of the cup regardless of the level of surgical experience remains unclear. We therefore divided the surgeons participating in the present study into experienced and inexperienced groups and investigated differences in achieved cup angle and spatial position [Citation26] between these two groups. The results showed no significant differences in the accuracy of cup positioning according to the level of surgical experience, in terms of both angle and spatial position.
Several limitations must be considered when interpreting the findings of this study. First is the retrospective nature of the study design. However, we were able to obtain postoperative CT images for 92.5% of the consecutive CT-based navigation hip series. We therefore think that bias in case selection was largely eliminated in this study. Second, one of the experienced surgeons always participated in the operation when an inexperienced surgeon used the navigation system. However, all the inexperienced surgeons completed the cases as the primary operator. Furthermore, the case series was initiated two years after the introduction of this navigation system at our institution. Consequently, both the experienced and inexperienced surgeons had already passed the “learning curve” period for navigation. This demonstrates that the inexperienced surgeons, after “learning”, can gain a good command of this navigation system. Third, the press-fit technique for the cup was not analyzed according to the level of surgical experience, in terms of parameters such as the incidence of use of dome screws or deviations of cup placement from the planned placement. Fourth, we excluded the 12 hips in which dome screws were used because the measurement of postoperative cup position with dome screws was technically demanding with this particular method. Recently, our group reported that there were no differences in cup angle between a revision THA group (in which dome screws were used in 70% of cases) and a primary THA group (in which no dome screw was used) using a more simplified measurement method [Citation27]. We therefore hypothesize that the influence of dome screws on the accuracy of cup positioning would be very small. One problem that arises when measuring the accuracy of cup positioning using two different images is how to precisely match the pre- and postoperative pelvic contours. Kalteis et al. [Citation11] reported that the accuracy of CT-based navigation was 3.0 ± 2.6° for inclination and 3.3 ± 2.3° for anteversion in absolute values. However, they also noted that the orientation of components is seriously influenced by pelvic references, and that matching two different images with the same reference points, such as the ASIS and pubic tubercles, is very difficult [Citation13]. We solved this problem using the volume registration technique [Citation14, Citation15], the reproducibility of which has already been determined, and achieved a high level of accuracy with 0.5 ± 2.3° for the inclination angle and −0.3 ± 1.6° for the anteversion angle of the cup using CT-based navigation. These results were more accurate than others that have been reported [Citation11]; this may be due to errors in matching pre- and postoperative pelvic references in previous studies.
Not only the accuracy of the cup angle, but also the accuracy of cup position is important for cases of distorted anatomy of the acetabulum, such as osteoarthritis secondary to hip dysplasia. When the spatial error is large, leg length may differ from the plan or the surgeon may break the acetabular column at the time of reaming. However, no prior reports have described the accuracy of spatial cup positioning with navigation. In the present study, we were able to measure accurately spatial errors of cup positioning using the volume registration technique and found that errors were ≤2 mm on each axis.
This study also found no significant differences in terms of the verification point check during navigation, the postoperative cup angle or spatial position. We thus conclude that this navigation system can assist in correct placement of the acetabular cup, irrespective of surgical experience, and that this technique is transferable from experienced surgeons to inexperienced surgeons within a short period of practice.
Declaration of interest
The authors report no commercial associations that might pose a conflict of interest in connection with this article.
References
- Patil S, Bergula A, Chen PC, Colwell CW Jr, D’Lima DD. 2003. Polyethylene wear and acetabular component orientation. J Bone Joint Surg Am 85-A(Suppl 4):56–63
- Nishii T, Sugano N, Miki H, Koyama T, Takao M, Yoshikawa H. 2004. Influence of component positions on dislocation: computed tomographic evaluations in a consecutive series of total hip arthroplasty. J Arthroplasty 19(2):162–6
- Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B. 2005. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br 87(6):762–9
- DiGioia AM, Jaramaz B, Blackwell M, Simon DA, Morgan F, Moody JE, Nikou C, Colgan BD, Aston CA, Labarca RS, et al. 1998. The Otto Aufranc Award. Image guided navigation system to measure intraoperatively acetabular implant alignment. Clin Orthop Relat Res (355):8–22
- Jolles BM, Genoud P, Hoffmeyer P. 2004. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop Relat Res (426):174–9
- Sugano N, Nishii T, Miki H, Yoshikawa H, Sato Y, Tamura S. 2007. Mid-term results of cementless total hip replacement using a ceramic-on-ceramic bearing with and without computer navigation. J Bone Joint Surg Br 89(4):455–60
- Losina E, Barrett J, Mahomed NN, Baron JA, Katz JN. 2004. Early failures of total hip replacement: effect of surgeon volume. Arthritis Rheum 50(4):1338–43
- Kreder HJ, Deyo RA, Koepsell T, Swiontkowski MF, Kreuter W. 1997. Relationship between the volume of total hip replacements performed by providers and the rates of postoperative complications in the state of Washington. J Bone Joint Surg Am 79(4):485–94
- Minoda Y, Kadowaki T, Kim M. 2006. Acetabular component orientation in 834 total hip arthroplasties using a manual technique. Clin Orthop Relat Res 445:186–91
- Blendea S, Eckman K, Jaramaz B, Levison TJ, DiGioia AM 3rd. 2005. Measurements of acetabular cup position and pelvic spatial orientation after total hip arthroplasty using computed tomography/radiography matching. Comput Aided Surg 10(1):37–43
- Kalteis T, Handel M, Bäthis H, Perlick L, Tingart M, Grifka J. 2006. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: Is it as accurate as CT-based navigation? J Bone Joint Surg Br 88(2):163–7
- Moskal JT, Capps SG. 2010. Improving the accuracy of acetabular component orientation: avoiding malposition. J Am Acad Orthop Surg 18(5):286–96
- Kalteis T, Handel M, Herold T, Perlick L, Paetzel C, Grifka J. 2006. Position of the acetabular cup – accuracy of radiographic calculation compared to CT-based measurement. Eur J Radiol 58(2):294–300
- Munch B, Ruegsegger P. 1993. 3-D repositioning and differential images of volumetric CT measurements. IEEE Trans Med Imaging 12(3):509–14
- Holden M, Hill DL, Denton ER, Jarosz JM, Cox TC, Rohlfing T, Goodey J, Hawkes DJ. 2000. Voxel similarity measures for 3-D serial MR brain image registration. IEEE Trans Med Imaging 19(2):94–102
- Takao M, Nakamura N, Ohzono K, Sakai T, Nishii T, Sugano N. 2011. The results of a press-fit-only technique for acetabular fixation in hip dysplasia. J Arthroplasty 26(4):562–8
- Sugano N, Takao M, Sakai T, Nishii T, Miki H, Nakamura N. 2009. Comparison of mini-incision total hip arthroplasty through an anterior approach and a posterior approach using navigation. Orthop Clin North Am 40(3):365–70
- Sugano N, Tsuda K, Miki H, Takao M, Suzuki N, Nakamura N. 2012. Dynamic measurements of hip movement in deep bending activities after total hip arthroplasty using a 4-dimensional motion analysis system. J Arthroplasty 27(8):1562–8
- Hirakawa K, Mitsugi N, Koshino T, Saito T, Hirasawa Y, Kubo T. 2001. Effect of acetabular cup position and orientation in cemented total hip arthroplasty. Clin Orthop Relat Res (388):135–42
- Udomkiat P, Dorr LD, Wan Z. 2002. Cementless hemispheric porous-coated sockets implanted with press-fit technique without screws: average ten-year follow-up. J Bone Joint Surg Am 84-A(7):1195–200
- Wan Z, Boutary M, Dorr LD. 2008. The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplasty 23(1):51-6
- Sugano N, Sasama T, Sato Y, Nakajima Y, Nishii T, Yonenobu K, Tamura S, Ochi T. 2001. Accuracy evaluation of surface-based registration methods in a computer navigation system for hip surgery performed through a posterolateral approach. Comput Aided Surg 6(4):195–203
- Watanabe Y MJ, Sasama T, Sato Y, Sugano N, Nishii T, Miki H, Yoshikawa H, Ochi T, Tamura S. 2003. Preprocessing method for rigid registration between pre- and postoperative CT images in total hip replacement. Med Imag Tech 21:358–68
- Malkani AL, Ong KL, Lau E, Kurtz SM, Justice BJ, Manley MT. 2010. Early- and late-term dislocation risk after primary hip arthroplasty in the Medicare population. J Arthroplasty 25(6 Suppl):21–5
- Thorey F, Klages P, Lerch M, Florkemeier T, Windhagen H, von Lewinski G. 2009. Cup positioning in primary total hip arthroplasty using an imageless navigation device: is there a learning curve? Orthopedics 32(10 Suppl):14–7
- Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. 2001. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am 83-A(11):1622–9
- Nakamura N, Nishii T, Kitada M, Iwana D, Sugano N. 2013. Application of computed tomography-based navigation for revision total hip arthroplasty. J Arthroplasty. [Epub ahead of print]