Abstract
Whereas the expansive open-door laminoplasty (EL) has been applied widely and the bone gutter on the hinge side is essential for EL, little is known regarding the mandatory width of the bone gutter. This study addressed the essential parameters of bone gutters for EL. Preoperative axial CT images of 20 patients suffering from cervical myelopathy were downloaded and entered into a computer. EL was then simulated using a computer-assisted technique and the thickness of the laminae at the gutter sites was measured. Accordingly, the width of the bone gutter was linked mathematically with the angle of the lifted lamina and the thickness of the lamina at the lamina-lateral mass junction. Furthermore, the average thickness of the laminae at the gutter site was 6.19 mm, and the appropriate bone gutter for EL was 5.13 to 7.15 mm. The width of the bone gutter can thus be planned precisely preoperatively, which may help improve the safety and accuracy of expansive open-door laminoplasty.
Introduction
Cervical laminoplasty has been widely adopted as a reliable and safe procedure for the treatment of multi-level cervical myelopathy including cervical spondylotic myelopathy (CSM), ossification of the posterior longitudinal ligament, and congenital cervical stenosis [Citation1–3]. Since the introduction of the classic technique by Hirabayashi and colleagues in 1981 [Citation1], a variety of studies have been reported, aiming to improve outcomes and minimize complications. At present, there are two main types of laminoplasty procedure: the expansive open-door laminoplasty (EL), also known as Hirabayashi laminoplasty, and the midline opening laminoplasty, also known as “French door” laminoplasty [Citation4].
EL allows for decompression of the cervical canal whilst maintaining the posterior elements simultaneously by elevating the laminae as a door upon a hinge. Consequently, it is of crucial importance for the surgery to keep the door open. The basic techniques of EL involve the creation of bone gutters on the lamina-lateral mass junctions using a high-speed burr, and the bone gutters in the hinged sides serve not only as hinges, but also as permanent stable elements, which gradually achieve osseous union following the surgery. From this point of view, the bone gutter on the hinged side plays a critical role in keeping the door open, and consequently in the outcome of the surgery. However, studies addressing the preparation of bone gutters are scant, and little is known regarding the mandatory width of bone gutters to maximize their function as hinges and subsequently facilitate osseous union.
To address these issues, this study aimed to clarify the essential parameters of bone gutters for EL via a computer-assisted analysis. Furthermore, a mathematical model based on the related parameters was established.
Methods
Patient data
Twenty consecutive patients who underwent expansive open-door laminoplasty in our institution during the period 2010–2012 were included in the study. They comprised 10 males and 10 female patients, with a mean age of 49.6 years (±SD: 14.89 years; range: 32–75 years). The diagnosis of cervical myelopathy was made based on clinical signs and symptoms of cervical myelopathy, with corresponding cervical stenosis on cervical MRI. The laminae involved were C3-6 in 7 patients and C3-7 in 13 patients. The study was approved by our institutional Ethics Committee (No. 20050917), with written informed consent being obtained from each patient.
Data collection
A CT scanner (GE Sytec 2000i) was used to perform scans from C3 to C7 of each patient, with a slice thickness of 3 mm, a window level of +300 Hounsfield units, and a window width of 1200 Hounsfield units. Preoperative axial CT images of the patients were downloaded and entered into the computer as described previously [Citation5]. The axial CT level of C5 was used on the grounds that C5 was involved in each of the laminoplasty surgeries performed.
Simulation of expansive open-door laminoplasty
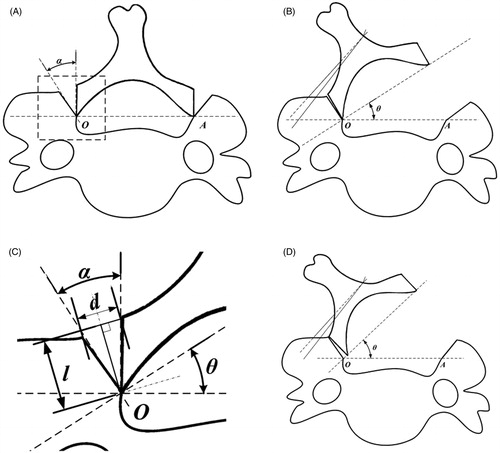
shows the bone gutters made at the lamina-lateral mass junctions on both sides. The lamina was then rotated around the most medial point of the gutter (O) until a target angle of open door was achieved, as shown in .
Figure 1. (A) The process of creating bone gutters during laminoplasty. (B) EL simulation with an elevated lamina angle of θ. (C) Radiological parameters and their geometric relationship in the bone gutter of EL. (D) EL simulation with an inappropriate bone gutter width. In this case, insufficient width of the bone gutter results in splitting of the gutter.
Radiographic assessment
Radiographs were digitized and entered into a DICOM PACS system. Visualization and measurements were performed using RadWorks 5.1 software (Applicare Medical Imaging BV, Zeist, The Netherlands). The thickness of the laminae of C5 where the bone gutters were made was measured independently by two spine surgeons.
Statistical analysis
The intra-observer and inter-observer reliability was analyzed using 2-way mixed-effect model intraclass correlation coefficients (ICCs). Reliability scores of less than 0.79, 0.80 to 0.89, and greater than 0.90 were regarded as poor, good, and excellent, respectively [Citation6]. SPSS 11 for Windows (SPSS, Inc., Chicago, IL) was used to perform the statistical analyses.
Results
The geometric relationship of the radiographic parameters of EL is shown in . From this geometric relationship, it can be deduced that
where θ is the angle of the lifted lamina, d is the width of the bone gutter, l is the thickness of the lamina, and α is the angle of the bone gutter in the bone gutter area of the hinged side.
Since the angle of the bone gutter should equal the angle of the lifted lamina, i.e., α = θ, then d = 2 l ċ tan(θ/2). Therefore, we can obtain d precisely on the basis of the data of l measured from CT scans of patients with CSM.
Good intra- and inter-observer reliability was noted in the evaluation of the thickness of laminae (>0.89). The mean thickness (l) of C5 laminae was 6.19 ± 1.18 mm (range: 5.05–8.06 mm).
Discussion
Cervical laminoplasty has been used for the posterior decompression of the cervical spinal cord in patients with multilevel cervical myelopathy [Citation1–3, Citation7]. The procedure allows widening of the spinal canal dimensions without permanently removing the dorsal elements of the cervical spine [Citation8]. However, re-closure of lifted laminae was reported as a short-term complication after EL using stay sutures or modified laminoplasty using various bone graft or fixation techniques [Citation9–11]. Fracture of a hinge or loss of spinal canal enlargement will result in nerve root or spinal cord palsy [Citation12], as later deterioration [Citation13], that may inevitably indicate re-operation (i.e., laminectomy) [Citation3, Citation8]. The key to preventing this lies in the preparation process for the bone gutter. Furthermore, the underlying determining factor in the outcome of laminoplasty, regardless of the diverse fixation methods for lifted laminae, is osseous union on the hinged side of the laminae. Therefore, the bone gutter on the hinged side of a laminoplasty plays a determining role in the clinical outcome of EL.
To our knowledge, this is the first study to predict accurate bone gutter width for EL via computer-assisted analysis.
In the study, a preoperative plan highlighting the bone gutter on the hinged side for EL was made using computer-aided analysis. EL was simulated and the involved parameters were integrated. Consequently, on the basis of the geometric relationship of the parameters, a mathematical equation was deduced which indicated that the width of the bone gutter (d) might be evaluated precisely prior to EL according to the thickness of the laminae (l) at the lamina-lateral mass junction. The thickness of the laminae (l) can be measured directly on CT images. These results may not only help shorten the preparation time for the bone gutter during surgery, but also help decrease bone gutter-related complications and consequently improve clinical outcomes. On the other hand, an inappropriate width of the bone gutter might lead to opening of the bone gutter edges, which would inevitably result in delayed union or non-union of the bone gutter and consequently to re-closure of the open door, as represented in .
Computer-assisted analysis has been used for spine surgery, not least for pedicle screw placement, with high-accuracy preoperative imaging and planning being translated into precise surgery [Citation14, Citation15]. In addition, a few studies have reported laminoplasty using computer-assisted analysis. Wang and colleagues [Citation5] studied canal expansion with both single open-door laminoplasty and double open-door laminoplasty using a computer-assisted technique. They concluded that the increased amount of canal following laminoplasty could be predicted by regression equations. However, the authors paid little attention to the bone gutter in laminoplasty. The computer-assisted simulation method of the present study was similar to that of Wang and colleagues. Therefore, computer-assisted analysis might be applied to more domains and facilitate accurate preoperative planning.
This study employed computer-assisted simulation and theoretical analysis with a mathematical equation. However, consistent with other theoretical analysis studies, we were unable to conduct a controlled clinical investigation comparing outcomes using preoperative planning with those obtained without planning. In common with other computer-assisted studies, the simulation of EL was conducted in a simplified and idealized way. It would be very difficult, if not impossible, to perform a similar simulation and analysis without simplification, as the shape of the bone gutter on the hinged side might be round and irregular in various scenarios (for patients as well as surgeons).
Apart from the width of the bone gutter (d), the angle of the lifted lamina (θ) is of crucial importance for clinical outcomes of EL since it is closely linked with canal enlargement [Citation5]. Clinically, studies have shown that neurologic improvement directly correlates with the degree of canal expansion. However, excessive expansion, as well as irregular canal area [Citation16], may be associated with additional problems [Citation17, Citation18]. It seems that optimal canal expansion approximates to 4 to 5 mm in the sagittal anteroposterior diameter [Citation2], correlating with an approximately 50% increase in canal area [Citation16, Citation19] and facilitating a 3-mm dorsal shift of the spinal cord [Citation20, Citation21]. Far more critical than canal expansion is subsequent cord expansion, with studies noting a direct correlation between Japanese Orthopedic Association scores and spinal cord area [Citation22]. On the other hand, previous studies reported the appropriate lamina angle (θ) [Citation17, Citation18], showing that θ should be within the range of 45–60° to prevent postoperative radiculopathy for single open-door laminoplasty. Therefore, the width of the bone gutter could be calculated on the basis of the equation with θ ranging from 45 to 60°.
In combination with the model used in our study, the bone gutter with a width ranging from 5.13 to 7.15 mm might be most appropriate for C5. With this in mind, we shortened the preparation process for the hinged bone gutter during the surgery for this patient series. On the other hand, in the open-door laminoplasty, a 3 - to 7-mm burr is usually used to form the gutter. In accordance with the model in this study, we propose that the smallest burr be used to obtain the V-shaped gutter, which will allow more bone contact when the lamina is elevated.
Given that the detailed information needed for expansive open-door laminoplasty could be predicted precisely using the equation, delicate preoperative planning might be applied in the foreseeable future to improve safety and accuracy, and thereby be beneficial for patients with cervical spondylotic myelopathy.
Declaration of interest
The authors report no declarations of interest.
References
- Hirabayashi K, Miyakawa J, Satomi K, et al. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976) 1981;6(4):354–64
- Hirabayashi K, Watanabe K, Wakano K, et al. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976) 1983;8(7):693–9
- Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 1: Clinical results and limitations of laminoplasty. Spine (Phila Pa 1976) 2007;32(6):647–53
- Hukuda S, Mochizuki T, Ogata M, et al. Operations for cervical spondylotic myelopathy. A comparison of the results of anterior and posterior procedures. J Bone Joint Surg Br 1985;67–B(4):609–15
- Wang XY, Dai LY, Xu HZ, Chi YL. Prediction of spinal canal expansion following cervical laminoplasty: A computer-simulated comparison between single and double-door techniques. Spine (Phila Pa 1976) 2006;31(24):2863–70
- Liu A, Schisterman EF, Wu C. Multistage evaluation of measurement error in a reliability study. Biometrics 2006;62(4):1190–6
- Hirabayashi K, Toyama Y, Chiba K. Expansive laminoplasty for myelopathy in ossification of the longitudinal ligament. Clin Orthop Relat Res 1999;(359):35–48
- Steinmetz MP, Resnick DK. Cervical laminoplasty. Spine J 2006;6(6 Suppl 1):S274–81
- Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine (Phila Pa 1976) 1988;13(7):870–6
- Satomi K, Ogawa J, Ishii Y, Hirabayashi K. Short-term complications and long-term results of expansive open-door laminoplasty for cervical stenotic myelopathy. Spine J 2001;1(1):26–30
- Lee JY, Hanks SE, Oxner W, et al. Use of small suture anchors in cervical laminoplasty to maintain canal expansion: a technical note. J Spinal Disord Tech 2007;20(1):33–5
- Yonenobu K, Oda T. Posterior approach to the degenerative cervical spine. Euro Spine J 2003;12:S195–201
- Chiba K, Ogawa Y, Ishii K, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy – average 14-year follow-up study. Spine (Phila Pa 1976) 2006;31(26):2998–3005
- Radermacher K, Portheine F, Anton M, et al. Computer assisted orthopaedic surgery with image based individual templates. Clin Orthop Relat Res 1998;(354):28–38
- Rao RD, Marawar SV, Stemper BD, et al. Computerized tomographic morphometric analysis of subaxial cervical spine pedicles in young asymptomatic volunteers. J Bone Joint Surg Am 2008;90(9):1914–21
- Baba H, Uchida K, Maezawa Y, et al. Three-dimensional computed tomography for evaluation of cervical spinal canal enlargement after en bloc open-door laminoplasty. Spinal Cord 1997;35(10):674–9
- O’Brien MF, Peterson D, Casey ATH, Crockard HA. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization: A computerized morphometric analysis. Spine (Phila Pa 1976) 1996;21(4):474–83
- Uematsu Y, Tokuhashi Y, Matsuzaki H. Radiculopathy after laminoplasty of the cervical spine. Spine (Phila Pa 1976) 1998;23(19):2057–62
- Shaffrey CI, Wiggins GC, Piccirilli CB, et al. Modified open-door laminoplasty for treatment of neurological deficits in younger patients with congenital spinal stenosis: analysis of clinical and radiographic data. J Neurosurg 1999;90(2 Suppl):170–7
- Sodeyama T, Goto S, Mochizuki M, et al. Effect of decompression enlargement laminoplasty for posterior shifting of the spinal cord. Spine (Phila Pa 1976) 1999;24(15):1527–1531; discussion 1531–2
- Vitarbo E, Sheth RN, Levi AD. Open-door expansile cervical laminoplasty. Neurosurgery 2007;60(1 Suppl 1):S154–9
- Nakano N, Nakano T, Nakano K. Comparison of the results of laminectomy and open-door laminoplasty for cervical spondylotic myeloradiculopathy and ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976) 1988;13(7):792–4