Abstract
Purpose: To introduce easy and useful methods using 3D navigation system with skin-fixed dynamic reference frame (DRF) in anterior cervical surgery and to validate its accuracy.
Methods: From September 2012 to May 2013, 31 patients underwent anterior cervical surgery and a total of 48 caspar distraction pins were inserted into each cervical vertebra. Every operation was performed using O-arm® navigation system with skin-fixed DRF. To validate the accuracy of these methods, a custom-made metal sleeve was used. In surgical field, through the metal sleeve, the tip of a navigation probe promptly contacts to the tip of caspar pin. We measured the vertical and horizontal distances and the angular deviation in sagittal plane between the caspar pin and the navigation probe on the virtual images and evaluated accuracy of navigation system with skin fixed DRF.
Results: Total 31 (males 20, females 11) patients and 48 caspar pins were included in this study. The mean horizontal distance between the caspar pin and the navigation probe displayed in navigation monitor was 0.49 ± 0.71 mm. The mean vertical distance between the caspar pin and the navigation probe displayed in navigation monitor was 0.88 ± 0.93 mm. And the mean angular deviation in sagittal plane between the caspar pin and the navigation probe displayed in navigation monitor was 0.59 ± 0.55°.
Conclusions: 3D navigation system with skin-fixed DRF in anterior cervical surgery is a simple and reliable method and it can be a helpful supplement to a spine surgeon’s judgement.
Introduction
Recently, a number of different manufacturers have offered spinal navigation systems that utilize technologies from preoperative CT scans to intraoperative 3D images which are being widely used in spinal surgeries.[Citation1–5] Although there are some differences in hardware and software functions, these systems basically enable the surgical instrument to be shown in reference to the displayed imaging anatomy in real time. Therefore, more precise and delicate operation after minimal exposure of the spinal structures could be possible even in deformed or severely degenerated spines.[Citation6] But setting up the navigation system has a steep learning curve which is difficult and requires a significant amount of time, especially in the case of early experience of image-guided surgery even in a simple procedure.[Citation3–5] Among every step of introducing the navigation system, the most important thing is the registration process for matching the image anatomy to the surgical anatomy. And setting a reliable reference frames has an important role to reduce registration inaccuracy. Our team already introduced a skin-fixed dynamic reference frame (DRF) into mini open transforaminal lumbar interbody fusion which can minimize interruption of surgical flow and effectively provide accuracy comparable to that obtained using a fixed bony attachment point for the DRF.[Citation7] On the other hand, until recently, in anterior cervical surgery, most surgeons did not use navigation systems because it was sufficient to perform anterior cervical discectomy and fusion or corpectomy under fluoroscope guidance or portable radiography. However, with continuous development of the techniques for minimal invasive and motion preservation surgeries such as anterior foraminotomy or multilevel oblique corpectomy, it is frequently required for those surgeries to acquire and use immediately updated anatomical information as well as positional information of surgical instruments under real-time multiplanar virtual image guidance at surgical field. Naturally, the use of navigation systems in anterior cervical surgeries has gradually increased. In these cases, setting up the navigation system is usually done with the fixed reference frame (FRF) which is attached to the head rest or operation table. But in this circumstance, the positioning of the patient on the operation table is occasionally movable, which can cause significant errors in the navigation system. To overcome this limitation, we designed skin-fixed DRF in anterior cervical surgery. The purpose of this study is to introduce a skin-fixed DRF in anterior cervical surgery and to validate its accuracy.
Materials and methods
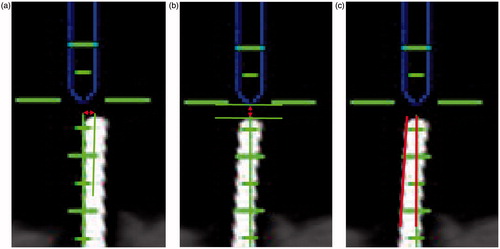
From September 2012 to May 2013, 31 patients underwent minimally invasive anterior cervical surgery and a total of 48 caspar pins were inserted into each cervical vertebra. Every operation was performed using Stealth station® and O-arm® (Medtronic Sofamor Danek, Inc., Memphis, TN). Detailed processes are as below. Prior to the surgical draping, the placement of 18 gauze needles on the surface of the operative level should be confirmed with portable radiography. While draping the patient, the forehead was exposed and covered with OPSITE® (Smith & Nephew, Hull, UK). And the DRF was firmly fixed on the exposed patient’s forehead using a fragmented OPSITE® (). According to the portable radiography, index level was exposed and caspar distraction pins were inserted to the each cervical vertebra. Then intraoperative 3D images of relevant spinal levels were obtained using O-arm®. The acquired image data were reformatted by the computer workstation into coronal, axial, sagittal, and three-dimensional views of the spinal anatomy. And setting up the navigation system was done based on the O-arm® image. To validate the accuracy of the skin-fixed DRF in anterior cervical surgery, a custom-made metal sleeve was used, which could maintain a constant connection between the tip of the caspar pin and the navigation probe, none of which were hand-held (). The metal sleeve had an outer diameter of 5 mm. The inside diameter was 3.4 mm and length was 123 mm. In surgical field, through the metal sleeve, the tip of navigation probe promptly contacted the tip of caspar pin. If there was a gap or an angular deviation between the tip of the caspar pin and the navigation probe on the virtual image, it could be considered as an error of navigation system. To minimize iatrogenic error or deviation, validation was performed immediately after intraoperative O-arm® scanning. Three images were captured at each operation, which showed the relationship between the tip of the caspar pin and the navigation probe on the computer workstation and were transferred to the custom software (Piview; Infinitt Co., Seoul, Korea). Finally, the vertical–horizontal distances and the angular deviation between the caspar pin and the navigation probe were measured three times each on sagittal plane by single observer (J.Y.C.) who did not participate in the operation (). Intra-class correlation coefficients (ICC) were used to determine the intra-observer reliabilities. And all measured data were analyzed using the Statistical Package for the Social Sciences software version 17.0 K (SPSS, Inc., Chicago, IL).
Figure 1. (a) During the draping the patient's forehead and eyes are exposed, and eyebrows are covered with sterile gauze to protect them from adhesive surgical film. (b) Exposed forehead is covered by transparent surgical film. (c) Mount reference frame on the forehead and fix it firmly with fragmented surgical film.
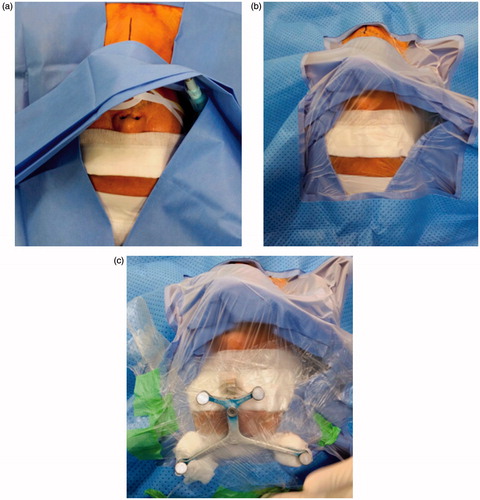
Figure 2. A custom-made metal sleeve (top of picture) can maintain a constant connection between the tip of the caspar pin (bottom right of picture) and the navigation probe (bottom left of picture), none of which were taken handheld. Each tip of caspar pin and navigation probe contacts promptly by the metal sleeve.

Figure 3. (a) A red bidirectional arrow indicates horizontal distance in sagittal plane between center of navigation probe (top) and caspar pin (bottom). (b) A red bidirectional arrow indicates vertical distance in sagittal plane between each end of navigation probe (top) and caspar pin (bottom). (c) Two red lines indicate cobb’s angle in sagittal plane between navigation probe (top) and caspar pin (bottom).
Results
In total 31 (males 20, females 11) patients and 48 caspar pins were included in this study. Anterior discectomy and fusion (ACDF) was performed in 3 patients; anterior corpectomy and fusion in 1; anterior foraminotomy in 4; and multilevel oblique corpectomy in 23, respectively ().
Table 1. Operative procedures.
A single-level surgery was done in 10 patients; two-level surgery in 11; and three-level surgery in 10. The mean time duration to set up navigation system with skin fixed DRF was only 4.8 min. There were no major complications or revision surgeries due to the navigational error and unintended durotomy was developed only in three cases without any neural injury, in which all of them had severe space-occupying calcified OPLL, but in all cases, in situ dura repair was done with artificial dura.
Consequently, the mean horizontal distance between the caspar pin and the navigation probe displayed in navigation monitor was 0.49 ± 0.71 mm. The mean vertical distance between the caspar pin and the navigation probe displayed in navigation monitor 0.88 ± 0.93 mm. And the mean angular deviation in sagittal plane between the caspar pin and the navigation probe displayed in navigation monitor was 0.59 ± 0.55° (). ICC value was 0.74 for intra-observer reliability.
Table 2. Measured parameters.
Discussion
To use the Stealth station® and O-arm® for image guidance, DRF is attached to the patient. An electro-optical camera tracks the position of the DRF in relation to the O-arm® during image acquisition. The obtained images are reconstructed and transferred to the computer workstation of Stealth station®. As with the Stealth station®, and O-arm®, the images are acquired with DRF fixed to the patient and integrated LED tracker of the O-arm®, therefore the registration step is allowed to be done automatically. This kind of registration process can reduce error origin from surgeon-dependent registration which requires a learning curve in selecting and matching the anatomical landmarks for optimal registration.[Citation8] But remaining problems are how to attach the DRF firmly to the patient and maintain its stable position during the operation without inhibiting the surgeon’s motion. Because the accuracy of the navigation system highly depends on the integrity of DRF which maintains the synchronization between the virtual navigated positions and the actual anatomical positions, consequently stable fixation of the reference frame is a critical step in navigated surgery.[Citation7] In anterior cervical surgery, the patient is usually placed in a supine position on the operating table. There is no reliable bony structure around the neck. Therefore in many cases of cervical operation using navigation system, reference frame is attached to the head rest or operation table instead of patient’s body.[Citation9–11] But in this setting, the movement of the patient on the operation table can cause significant mismatch between real anatomy and virtual images. And the reference frame may prohibit the natural movement of assistant surgeon during the operation. To overcome all of these inconveniences, we designed a simple and minimal-space-occupying methods to set up DRF. Simply attaching the DRF to the patient’s forehead using surgical tapes instead of conventional methods make the reference frame attached to bed or headrest. It takes only a few minutes. But results from these novel methods are reliable and satisfactory. The mean errors in the horizontal and vertical planes were 0.49 and 0.88 mm, respectively, and the angular deviation was only 0.59°. Although procedure-specific limitations of acceptable registration error exist, in general, the mean fiducial localization errors of less than 1.5 mm are considered adequate for most spinal procedures.[Citation12–15] We usually use this method to perform anterior cervical foraminotomy and multilevel oblique corpectomy especially in order to check depth and width of corpectomy as well as location of pedicle and foramen transversarium. Despite long segment surgeries, the length of skin incision can be limited, so it is possible to elevate the tension of skin and muscle until retracting the caspar pins which can distort original position and angle of them. In this situation, although there is no navigational error, the tips of caspar pin and navigation probe cannot contact each other promptly in virtual images. But other anatomical landmarks are usually found in the correct position in the virtual images. Consequently, we can perform several kinds of surgeries successfully. There have been only three cases of unintended durotomy without any neural injury, which also are not related with navigational error, because all of these cases have severe space-occupying calcified OPLL and dural adhesion. But there were no major complications such as neurovascular or tracheo-esophageal complex injury.
Nevertheless there were several limitations. First this study was performed with a small number of cases. It is required to evaluate more caspar retraction pins. Second, a single observer participated in the evaluation. For better intra- and inter-observer reliabilities, there should be multiobservers in measurement. Third, although the skin-fixed DRF can reduce the possible navigational errors occurred from the movement of the patient on the operation table, it is still not perfect. Because it is not fixed to the bony structures, a significant change in the patient’s position can cause inevitable navigational errors. Finally, notwithstanding the fact that the navigation system with skin-fixed DRF has an acceptable range of error in cervical spine, even an error of just a few millimeters can lead to devastating complications. To overcome this, surgical and anatomical orientation rather than blind faith in the navigation system will be required.
Conclusion
With development of the navigation system, a spine surgeon can perform complex and minimal invasive surgery successfully without radiation hazard, but many surgeons are still unfavorable to the navigation system and do not trust it due to its expensive cost, complex methods for registration and set-up process, learning curve, and interruptions to working flow. We think this method will be one part of solution to overcome these kinds of problems. And we believe that 3D navigation system with skin-fixed DRF in anterior cervical surgery can be a helpful supplement to a spine surgeon’s judgement.
Declaration of interest
Sang Hoon Jang, Ji Young Cho, Won chul Choi, Ho Yeon Lee, Sang Ho Lee, Jae Taek Hong declare that they have no conflict of interest. This study was supported by a grant from the Wooridul Spine Foundation.
References
- Acosta FL, Thompson TL, Campbell S, et al. Use of intraoperative isocentric C-arm 3D fluoroscopy for sextant percutaneous pedicle screw placement: case report and review of the literature. Spine 2005;5:339–343.
- Fritsch E, Duchow J, Seil R, et al. Accuracy of fluoroscopic navigation of pedicle screws. CT-based evaluation of bone screw placement. Der Orthopade 2002;31:385–391.
- Holly LT, Foley KT. Intraoperative spinal navigation. Spine 2003;28:S54–S61.
- Tjardes T, Shafizadeh S, Rixen D, et al. Image-guided spine surgery: state of the art and future directions. Eur Spine J 2010;19:25–45.
- Holly LT, Foley KT. Image guidance in spine surgery. Orthop Clin North Am 2007;38:451–461.
- Moses ZB, Mayer RR, Strickland BA, et al. Neuronavigation in minimally invasive spine surgery. Neurosurg Focus 2013;35:E12.
- Cho JY, Chan CK, Lee SH, Lee HY. The accuracy of 3D image navigation with a cutaneously fixed dynamic reference frame in minimally invasive transforaminal lumbar interbody fusion. Comput Aided Surg 2012;17:300–309.
- Holly LT, Bloch O, Johnson JP. Evaluation of registration techniques for spinal image guidance. J Neurosurg Spine 2006;4:323–328.
- Hott JS, Papadopoulos SM, Theodore N, et al. Intraoperative iso-C C-arm navigation in cervical spinal surgery: review of the first 52 cases. Spine 2004;29:2856–2860.
- Summers LE, Kouri JG, Yang M, et al. Odontoid screw placement using isocentric 3-dimensional C-arm fluoroscopy. J Spinal Disord Tech 2008;21:45–48.
- Nottmeier EW, Young PM. Image-guided placement of occipitocervical instrumentation using a reference arc attached to the headholder. Neurosurgery 2010;66:138–142.
- Rampersaud YR, Simon DA, Foley KT. Accuracy requirements for image-guided spinal pedicle screw placement. Spine 2001;26:352–359.
- Best NM, Sasso RC, Garrido BJ. Computer-assisted spinal navigation using a percutaneous dynamic reference frame for posterior fusions of the lumbar spine. Am J Orthop (Belle Mead, NJ) 2009;38:387–391.
- Villavicencio AT, Burneikiene S, Bulsara KR, Thramann JJ. Utility of computerized isocentric fluoroscopy for minimally invasive spinal surgical techniques. J Spinal Disord Tech 2005;18:369–375.
