Abstract
More knowledge is needed about how different rehabilitation models in the municipality influence stroke survivors’ ability in activities of daily living (ADL). Objectives: To compare three models of outpatient rehabilitation; early supported discharge (ESD) in a day unit, ESD at home and traditional treatment in the municipality (control group), regarding change in ADL ability during the first three months after stroke. Methods: A group comparison study was designed within a randomized controlled trial. Included participants were tested with the Assessment of Motor and Process Skills (AMPS) at baseline and discharged directly home. Primary and secondary outcomes were the AMPS and the modified Rankin Scale (mRS). Results and conclusions: Included were 154 participants (57% men, median age 73 years), and 103 participants completed the study. There were no significant group differences in pre–post changed ADL ability measured by the AMPS. To find the best rehabilitation model to improve the quality of stroke survivors’ motor and process skills needs further research. Patients participating in the ESD rehabilitation models were, compared with traditional treatment, significantly associated with improved ADL ability measured by the mRS when controlling for confounding factors, indicating that patients with social needs and physical impairment after stroke may benefit from ESD rehabilitation models.
Introduction
Stroke is a major cause of disability in the Western world. It is assumed that the burden of stroke will rise in the future because of an increasing elderly population and better survival after stroke (Citation1,2). Many stroke survivors are in need of rehabilitation (Citation3), and ability in activities of daily living (ADL) is a highly recommended marker of treatment effect (Citation4). Limited ADL skills imply costs for the society (Citation5), individual burdens like post-stroke depression (Citation6), and loss of social contact and valued roles (Citation7). This emphasizes the importance of designing rehabilitation models with the best possible gain in stroke survivors’ ADL ability.
A 2013 Cochrane report from Stroke Units Trialists’ Collaboration has established that acute care in an organized inpatient stroke unit is beneficial for patients in their endeavour to regain independence early after stroke and to remain independent in the long run (Citation8). A 2012 Cochrane report from Early Supported Discharge Trialists recommends ESD from hospital and follow-up rehabilitation at home, rather than conventional care in hospital, in order to reduce long-term dependency after mild-to-moderate stroke (Citation9). The applied ESD assumes coordinated treatment delivered by multidisciplinary ESD teams in the municipality who offer task-specific and intensive intervention (Citation4,9,10). A systematic review reports a positive effect of ESD and home rehabilitation on instrumental ADL like cooking and other activities requiring increased interaction with the environment, but no effect on basic ADL like dressing and toileting (Citation11). Another review comparing home-based rehabilitation with centre-based rehabilitation in the municipality suggests a functional benefit in favour of home-based rehabilitation up to six months after the stroke (Citation12). However, according to a later Cochrane report no effect was found on basic ADL scores and the reported improvements in patients’ instrumental ADL scores seems to disappear in the long run (Citation9).
One possible explanation for the limited effect may be a ceiling effect for some of the well-known outcome measures, meaning that many stroke survivors might already have reached the measure’s best score at discharge (Citation13). Others have pointed out that responsiveness to change is not satisfactorily evaluated for many of the commonly used instruments (Citation14). The modified Rankin Scale (mRS) is one frequently used measure of ADL ability and is widely applied in randomized controlled trials (RCT) for evaluating recovery after stroke. In a literature review assessing the psychometric properties of mRS, it is suggested that mRS might be advantageous over other commonly used instruments in terms of ceiling effect, but the use of mRS is criticized for being subjective and the information regarding its responsiveness to change is limited (Citation15). The Assessment of Motor and Process Skills (AMPS) has relatively recently been recommended as a measure of ADL ability after stroke (Citation16). The AMPS meets the requirements of standardization, it is objective, and no ceiling effect is reported (Citation17). Its ability to detect change is adequately evaluated (Citation14). To our knowledge the AMPS has formerly not been used in the context of ESD and only in two RCTs including stroke survivors, comparing changed ADL ability between home- and hospital-based day rehabilitation for a marginalized group of young stroke survivors (Citation18) and a mixed group including patients with stroke (Citation19). No differences between the groups were found in these studies.
Current evidence supports ESD from hospital to home after acute hospital treatment as patients have demonstrated benefits in independence. However, the influence of different rehabilitation models on the patients’ ADL ability is still scarcely explored. A limitation in previous studies may also have been inappropriate measurement tools, and a lack of focus on different contexts for rehabilitation. The objective of this study was to compare three models of outpatient rehabilitation: ESD in a day unit, ESD at home, and traditional treatment in the municipality (control group) using the AMPS as a primary outcome and the mRS as a secondary outcome measure. It was hypothesized that the ESD models would result in superior outcomes regarding change in ADL ability (performance and independence) during the first three months after stroke.
Materials and methods
Design
A group comparison study was designed within a RCT entitled “ESD Stroke Bergen” (Citation20). The intervention was ESD in a day unit or ESD at home. The control group were given traditional treatment in the municipality. The study was approved by a Norwegian Regional Ethics Committee (No.070.08).
Inclusion and exclusion criteria
Eligibility criteria for the RCT (Citation20) were: included within 6–120 hours after admission to the hospital and within 1–7 days after symptom onset, National Institute of Health Stroke Scale (NIHSS) score of 2–26 at inclusion, or increased mRS score of two points, if 0 or 1 previously. Written informed consent for participation in the study was given by the participants themselves or by relatives. Exclusion criteria were: poor knowledge of the Norwegian language before the stroke, serious conditions like psychiatric disorders, or substance abuse of importance to the cerebral disorder and subsequent rehabilitation process. Included in the present sub-study were only patients who were tested with the AMPS at baseline and discharged directly home. Excluded were those who went to an institution before homecoming. Patients without follow-up testing were dropouts.
Outcomes
The AMPS, our primary outcome measure, has relatively recently been recommended as a measure of ADL ability after stroke (Citation16). Research has demonstrated high reliability for test–retest, inter- and intra-tester, as well as parallel forms reliability (Citation17,21,22). Several studies support the validity of AMPS used in stroke survivors, despite differences in underlying impairments (Citation23,24), across age (Citation25) and gender (Citation26,27), making the AMPS appropriate for the current study. In particular, the AMPS provide information concerning a patient’s ADL ability given on two separate interval scales; the quality of the patient’s motor skills (AMPS motor) ranging from –3 to +4, and the quality of process skills (AMPS process) ranging from –4 to +3 (Citation17,28). The higher the score along the AMPS scales, the higher the quality of a person’s ADL skills in performing any ADL task (Citation17). The AMPS is considered a measure placed somewhere between the evaluation of discreet body function and global ADL. The scores on the scales are commonly dichotomized to determine whether the quality of one’s ADL skills is sufficient to live independently at home or not. Dichotomized AMPS, motor and process, were used as secondary outcomes. Independence was indicated by a score above 1.5 on the AMPS motor scale and above 1.0 on the AMPS process scale (Citation29). Scores below or equal to these cut-off levels indicated dependency. A matched decision between the dichotomized AMPS outcomes (motor and process) is shown as a highly accurate estimate in the prediction of need for assistance when living at home (Citation29). An outcome termed AMPS total was therefore used to reflect participants who were categorized as independent measured with both AMPS motor and AMPS process scales.
The mRS was another secondary measure used, a standardized and recommended instrument of global ADL performance, demonstrating high reliability and validity in stroke survivors (Citation15). A seven-point ordinal scale (0–6) was used (Citation30). Zero indicates competent ADL performance, 1 minor physical impairments, 2 participation restrictions (independent in ADL), 3 and 4 ADL limitations, 5 severe disabilities, and 6 deaths. The mRS is also used to determine whether the patient is dependent or independent in ADL. This categorical variable is given by a criterion-referenced cut-off score below or equal to 2 that indicates independent ADL performance. Scores above 2 indicate dependency in ADL (Citation31).
Procedure
Recruitment
The inclusion period was December 2008 to December 2011, with a three-month re-testing after inclusion, ending in March 2012. The participants were enrolled in the study by a person who was not involved in either the randomization process or the treatment. None of the authors were involved in treatment or data collection.
Randomization
The participants were randomly assigned to one of three groups, ESD in a day unit, ESD at home, or traditional treatment in the municipality, following computer-generated block randomization with six participants in each block, in the same order as they were included in the study. The group was unknown to the patients and those who administered the tests at baseline. The patients were instructed not to inform those who were involved in the re-testing of their group allocation.
Intervention
ESD intervention meant that the patients were discharged from hospital to their home as early as possible, taking medical and practical conditions into consideration, provided that support was given by a multidisciplinary hospital outreach team during hospitalization and to the end of follow-up. This team served as a link among all stakeholders and coordinated the rehabilitation process. This included handling home visits, transfers between units at different health-care levels and a systematic multidisciplinary follow-up at the hospital outpatient clinic at three months after inclusion in the study. After the return home, a multidisciplinary municipal health-care team was responsible for further support and treatment, provided either in a day unit or at home (Citation20). For both ESD groups, treatment was guided by national guidelines (Citation16), started with a home visit within three days after discharge, and lasted for a maximum of five weeks after the home visit (Citation32). Additionally, the patients were encouraged to engage in meaningful activities on their own, and most patients chose ADLs as their home exercise (Citation32). The participants’ were provided with medical support from their general practitioner or treatment by other relevant health-care professionals (Citation20). The main difference between the ESD interventions was the context of rehabilitation and some difference in length of treatment.
ESD day unit
Participants in the day-unit group were transferred from their homes to a day unit for treatment by the municipal health-care team, usually given by an occupational therapist and/or a physiotherapist (Citation32). Intensity of treatment was in mean (min, max) 22 hours (4 hours, 50 hours) spread over four weeks (Citation33). Treatment was mainly individualized and focused on specific functions like training of memory or of hand function, but also on specific instrumental ADL activities (Citation32). Eating lunch together gave the opportunity to socialize with other stroke survivors. Treatment in groups such as walking together was offered, but to a limited extent. Additional treatment by a physiotherapist in the municipality was received by 24% of the participants (Citation32).
ESD home
The patients in the home group were offered treatment in their home by the municipal health-care team (Citation32). Intensity of treatment was in mean (min, max) 17 hours (1 hour, 49 hours), spread over four weeks (Citation33). Treatment was mainly directed towards ADLs, but function-specific treatment was also offered (Citation32). Treatment was usually given by an occupational therapist and/or a physiotherapist. In the home group, 27% of the participants received additional physiotherapy in the municipality (Citation32).
Control group
The control group were not supported or followed by the hospital outreach team or the municipal health-care team. Follow-up treatment in the municipality is usually prescribed from hospital and partly on the basis of the patient’s scores on physical outcome measures like the mRS, meaning that follow-up rehabilitation is not provided to all patients (Citation34). Ordinary treatment is based on the patient’s needs, and probably guided by national guidelines (Citation16). This may involve treatment at home by a nurse, physical therapist, or occupational therapist from the home municipality and/or treatment by a private practising physiotherapist. There is usually no overall coordination of the rehabilitation process and no multidisciplinary team is available. The patient is commonly contacted by a health-care professional based on recommendations from the hospital. No further information regarding content, length, or intensity of treatment is available for the control group.
Testing and re-testing
The baseline AMPS test was carried out at the Department of Occupational Therapy. This was close to the stroke unit where the participants received their acute treatment, and where the baseline mRS were assessed. There was a median of one day between the participant’s admission to hospital and the baseline AMPS. Re-testing was conducted in conjunction with the systematic three-month follow-up. To standardize the AMPS re-testing condition, the test was carried out at the hospital outpatient clinic. The assessment is in accordance with the AMPS manual (Citation17,28), which means observations of a patient performing two self-chosen and previously known ADL tasks, and calibrated therapists focusing on patients’ small skills like grasping a tool or selecting an appropriate sequence of implantation. How effectively, safely, and independently the ADL task is performed, as well as the effort used during performance, is the basis for the scores given on a four-point ordinal scale. This raw score was converted by a many-faceted Rasch analysis taking into account that patients vary in ADL ability, therapists vary in severity of their ratings, and ADL tasks vary in difficulty (Citation17).
The baseline mRS was conducted seven days after inclusion or earlier if needed depending on time of discharge. Re-test was in conjunction with the systematic three-month follow-up. No equipment was required for the mRS re-testing, which therefore was performed either at the hospital outpatient clinic or during home visits. The baseline mRS was administered by trained stroke nurses or neurologists and re-testing was done by a trained physiotherapist. Their clinical assessment was guided by a structured interview (Citation30), including conversation with and observation of the patient, and was the background for the scores given.
Sample size
A sample size of 64 participants per group was necessary to detect a clinically important difference of 0.5 logits (SD = 1) in both AMPS measures between three groups. This is in agreement with the AMPS manual (Citation17), with a two-tailed 5% significance level and a power of 80%. The main study (ESD Stroke Bergen) used mRS as main outcome for sample size calculation, and the sample size for the present sub-sample of patients discharged home directly was smaller than recommended for comparing three groups with AMPS.
Statistical methods
Descriptive statistics (frequencies and percentages, means and SD, median and range) were used to characterize the included participants at baseline, as well as the patients who were re-tested and those who were dropouts. The last two groups were compared by t-test (age, AMPS and mRS scales, bed-days), Mann–Whitney U-test (NIHSS) or exact chi-square (gender, civil status, type of stroke, affected hemisphere, AMPS and mRS cut-offs).
For the patients who completed the study we tested whether there were pre–post changes in AMPS and mRS by paired-samples t-test (scale measures) or McNemar’s test (dichotomized measures) and whether the pre–post changes differ between the three treatment groups using ANOVA (scale measures) or exact chi-square (dichotomized measures).
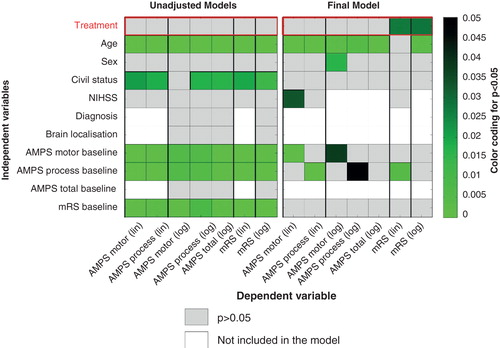
Taking into account the violation of the randomization properties because of the high dropout rate we had to control for possible confounding. This was done by estimating regression models with AMPS and mRS at three months as dependent and treatment as independent variable, adjusted for age, sex, civil status, as well as baseline NIHSS and ADL scores. For AMPS and mRS scale measures we fitted a linear model with treatment in two groups (ESD home and ESD day unit as one group versus control group), while we used a logistic regression with treatment in three groups (ESD home and ESD day unit as separate groups versus control group) for dichotomized measures. For all regressions we first estimated an unadjusted model to examine the association between the dependent variables at follow-up and each independent variable and then a fully adjusted model to investigate the association between the dependent variables and the total impact of all independent variables. These results, and the results from a correlation analysis between the independent variables, were used to define a final regression model based on clinical relevance and significance (Citation24,35,36). This way of modelling enabled us to increase the power in the model as much as possible due to the limited sample size.
Level of significance was set at 0.05. SPSS 21.0 (SPSS Inc., IL, USA) was used for statistical analysis and Matlab 2010b for graphics.
Results
Included in the current study were 154 participants who were tested with the AMPS at baseline and discharged directly home. From the included sample, 103 participants were re-tested at three months and thereby completed the study (). Baseline characteristics of the included sample are given in . The median age of the participants was 73 years, 57% were men and 62% lived with a partner. The median NIHSS score was in the mild range (median score 4.0) of the scale (Citation31) and most (91%) had suffered an ischaemic stroke. A majority of the participants were dependent in ADL at baseline as measured by the dichotomous AMPS, while this was the case for a minority as measured by the dichotomous mRS. The baseline characteristics of participants who completed the study and those who were dropouts are given in . Dropouts were found to be older (p = 0.003), more often live alone (p = 0.008), and suffer a more complicated stroke (p = 0.041) compared with those who completed the study. Pre–post changes in outcomes are shown in . For the cohort who completed the study, significant pre–post within-group improvements were found for the AMPS scores (all p < 0.001), but no significant changes were found for the mRS (p = 0.063). also shows trends of differences in changed outcome from baseline to three month follow-up between ESD groups and control group, but no significant differences were found. The results of the regression analyses are illustrated in . Details are found in the supporting information shown in Tables S1–S7. Controlling for possible confounding factors, no significant association was found for ESD groups versus control group of improved ADL ability for any AMPS scale, while significant associations were found for the mRS scale (p = 0.027) and the dichotomous mRS (p = 0.028). We observed for the merged ESD groups (day unit and home in one group) a significantly better relationship with improved ADL performance (lower score) at three months, than for the control group [B(CI) = –0.39(–0.73,–0.05)], and for each of the ESD groups significantly higher odds to be classified as independent than for the control group defined as the reference group (home: OR[CI] = 10.45 [1.47, 74.15], day-unit OR[CI] = 19.71 [1.74, 222.63]). Note that ADL ability was significantly associated with age in most models. AMPS scores (motor and process) at three months were significantly associated with corresponding baseline scores, while AMPS total and mRS were not.
Figure 1. Flow diagram of all stroke patients randomized to different models of stroke rehabilitation at baseline, being assessed by the AMPS at baseline, and discharged home directly, as well as patients who completed the study, being re-tested with the AMPS at 3 months, and dropouts.
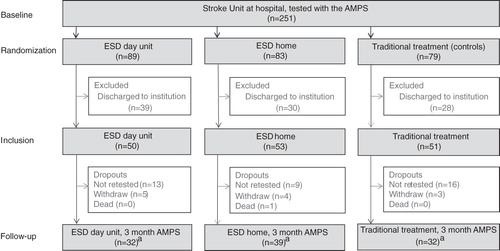
Table I. Baseline characteristics of included participants by intervention groups and control group.
Table II. Differences in baseline characteristics between participants who were included in pre–post analysis and those who were dropouts.
Table III. Pre–post change in activities of daily living (ADL) and between-group comparisons.
Discussion
In this study we examined the effect of ESD models of rehabilitation on changed ADL ability (performance or independence) in patients with stroke discharged directly home. During the first three months after stroke, we found no significant differences when comparing change between participants in the ESD home or ESD day unit, and traditional treatment groups. Controlling for possible confounding factors, the ESD rehabilitation models were not found to be associated with improvement in ADL ability (performance or independence) measured by the AMPS. The mRS, the secondary outcome measure was, however, associated with the rehabilitation models.
Strengths and limitations
The strengths of this study are the psychometric qualities of the AMPS, the use of blinded test administrators and the relatively high number of included participants tested with the AMPS, although the power of the study was low. The baseline characteristics of the cohort included () are well balanced between the intervention groups and control group even if this was a non-stratified sub-study of patients discharged home directly. As expected, the participants had stroke severity at the mild end of the NIHSS scale, previously shown to be the target population of ESD intervention (Citation4,9). A high proportion of the participants also managed fairly well in ADL. The high proportions of independent patients, indicated by the mRS but not by the AMPS, are probably mostly due to the timeframe between the two tests, and might reflect improvement that tends to occur early after the stroke (Citation34).
The low and almost equal number of bed-days in the stroke unit, shown for both intervention groups and control group, were unexpected and represent a limitation of the current study. The short stay at the stroke unit may be due to better stroke treatment and hence better outcome during the last decade (Citation37). A trend towards shorter hospital stays is shown to be the case for all Scandinavian countries (Citation37). Promising results from new methods of treatment may also contribute to better functional outcome and might reduce the need for long stays in acute stroke units (Citation38), indicating a need to focus on the effect of a shorter hospital stay in future studies (Citation39).
The cohort analysed () consisted of younger patients, and included more men and more patients with ischaemic stroke when compared with the general Norwegian stroke population (Citation40). The main concern with the current study is, however, the high loss to follow-up. Many of these participants were old, lived alone, and suffered a complicated stroke, challenges which have also previously been described (Citation41). This offers valuable information to researchers involved in re-testing, in situations where participants are supposed to attend hospital follow-ups. A pick-up and return service in connection with the re-testing, or re-testing in the patient’s home might have helped to limit the loss to follow-up. However, the effect of the environment on the AMPS results when testing similar patients in the hospital and in their homes is not fully understood, nor is the use of different hospital environments in pre–post assessments (Citation17), which might have biased the outcome of the current study. Although we chose to rely on research showing adequate inter-rater reliability for the AMPS and the mRS (Citation15,17), readers must also be aware of possible bias caused by the use of different testers in pre–post assessment, as well as the limited sample size leading to low power and increased probability of type II error.
Changed ADL ability and between-group comparisons
We did not find a significant effect of ESD on the patients’ changed ADL ability (performance or independence) compared with treatment as usual. An explanation may have been the assumed application of national guidelines for treatment and rehabilitation after stroke (Citation16), which gives reasons to believe that stroke survivors in all treatment groups were provided with high-quality rehabilitation. Even if we lack some information concerning the content and amount of treatment received by the control group, which is a limitation of the current study, it seems likely that treatment in the ESD groups did not differ essentially from the treatment given in the municipality. Even if patients dependent in ADL are assumed to be referred for further follow-up rehabilitation after being discharged home (Citation34), more detailed information on the control group is needed, and should be incorporated in future studies of ESD. Note that, even if not significant, we observed a slightly better outcome in the ESD groups based on change scores on the mRS (), and the relatively good clinical condition of the stroke survivors at baseline, which hampers the possibility of revealing any differences even with a high sample size. However, Gjelsvik et al. found, in a similar sample of the current RCT, a positive effect of ESD on self-reported ADL (Citation33). This means perhaps poor concurrences between stroke survivors’ perceived problems and what is captured by standardized measures (Citation42,43) such as AMPS and mRS. Other authors have also suggested a need for health-care professionals to pay attention to outcomes dealing with the emotional consequences of stroke (Citation44).
In our study, we found a significant improvement in ADL ability (performance and independence) within the cohort who were tested by the AMPS at both test points, and most of the participants ended up being independent in ADL. This suggests success of the overall rehabilitation scheme and confirms the benefits of AMPS in capturing improvement (Citation14). This potential benefit of the AMPS in clinical practice may be taken into consideration by health-care professionals involved in stroke rehabilitation. Within those who were re-tested, no significant difference was found by the mRS in changed ADL ability. This may be due to the fact that a substantial proportion of patients worsened their pre–post ADL ability, indicating that the mRS may be better suited to capture deterioration than the AMPS. The relatively high proportion of independent patients shown by the mRS at baseline suggests that also a ceiling effect may have been introduced by dichotomizing the mRS. Evaluation of responsiveness of the mRS in different subgroups of patients with stroke is warranted (Citation15).
Controlling for confounding factors
Controlling for possible confounding factors, we found the patients participating in the ESD rehabilitation models, compared with traditional treatment, to be significantly associated with improved ADL ability (performance and independence) measured by the mRS, but not by the AMPS. While the AMPS is a measure of motor and process skills needed to perform ADL tasks (Citation17), underlying physical impairment and participation in society is part of the assessment using the mRS (Citation15,30). Taking the measurements’ somewhat divergent focus into account, our results may indicate that ESD is best suited towards improvement of physical and/or social functioning. The best rehabilitation model for stroke survivors with other needs, however, justifies further investigation. Expanding health-care professionals’ understanding of stroke survivors’ ADL skills in performing ADL tasks might require an evaluation of the widespread confidence in global ADL measures, which has been pointed out in previous studies (Citation9). The effect of treatment seems to be weaker than the effect of age and ADL ability before treatment, measured by the AMPS. This is in line with previous research, which found a decline in ADL ability as measured by the AMPS, associated with increased age (Citation24). Other indicators, such as cognitive abilities or comorbidities, are also cofactors explaining changes in ADL ability among stroke survivors, factors we did not have access to in our study (Citation15).
Conclusions
The current study suggests that there is no difference between the treatments when comparing change in independence and performance measured by the AMPS. Consequently, we cannot give a clear recommendation on how to improve the quality of stroke survivors’ motor and process skills in performing ADL tasks in the best way, which must remain to be investigated in further research. On the other hand, patients with social and physical needs after stroke may benefit from ESD.
IOCC_A_1042403_SM1223.docx
Download MS Word (47.2 KB)Acknowledgements
The Norwegian Extra Foundation for Health and Rehabilitation funded this study (project number 2011/2/0135). The authors especially thank the research participants. They also thank Håkon Hofstad for contributing data to this study and the occupational therapists involved in the planning of the study and collection of the AMPS data.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Notes
References
- Truelsen T, Piechowski-Jozwiak B, Bonita R, Mathers C, Bogousslavsky J, Boysen G. Stroke incidence and prevalence in Europe: A review of available data. Eur J Neurol 2006;13:581–98.
- Donnan G, Fisher M, Macleod M, Davis S. Stroke. Lancet 2008;371:1612–23.
- Young J, Forster A. Review of stroke rehabilitation. BMJ 2007;334:86–90.
- Fisher R, Gayor C, Kerr M, Langhorne P, Anderson C, Bautz-Holter E, et al. A consensus on stroke: Early supported discharge. Stroke 2011;42:1392–7.
- Björkdahl A, Sunnerhagen K. Process skill rather than motor skill seems to be a predictor of costs for rehabilitation after a stroke in working age; A longitudinal study with a 1 year follow-up post discharge. BMC Health Serv Res 2007;7:209.
- Ouimet M, Primeau F, Cole M. Psychosocial risk factors in poststroke depression: A systematic review. Can J Psychiatry 2001;46:819–28.
- Pound P, Gompertz P, Ebrahim S. A patient-centred study of the consequences of stroke. Clin Rehabil 1998;12:338–47.
- Stroke Unit Trialists’ Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev 2013;9:CD000197.
- Fearon P, Langhorne P; Early Supported Discharge Trialists. Services for reducing duration of hospital care for acute stroke patients. Cochrane Database Syst Rev 2012;9:CD000443.
- Walker M. Stroke rehabilitation: Evidence-based or evidence-tinged? J Rehabil Med 2007;39:193–7.
- Winkel A, Ekdahl C, Gard G. Early discharge to therapy-based rehabilitation at home in patients with stroke: A systematic review. Phys Ther Rev 2008;13:167–87.
- Hillier S, Inglis-Jassiem G. Rehabilitation for community-dwelling people with stroke: Home or center based? A systematic review. Int J Stroke 2010;5:178–86.
- Disler P, Wade D. Should all stroke rehabilitation be home based? Am J Phys Med Rehabil 2003;82:733–5.
- Pouline V, Korner-Bitensky N, Dawson D. Stroke-spesific executive function assessment: A literature review of performance-based tools. Aust Occup Ther J 2013;60:3–19.
- Banks J, Marotta C. Outcomes validity and reliability of the modified Rankin scale: Implications for stroke clinical trials: A literature review and synthesis. Stroke 2007;38:1091–6.
- Helsedirektoratet. [National guidelines for treatment and rehabilitation after stroke]. In Helsedirektoratet, editor. Nasjonale retningslinjer for behandling og rehabilitering av hjerneslag. Helsebiblioteket.no: Helsebiblioteket, Oslo; 2010.
- Fisher A, Jones K. Assessment of motor and process skills volume 1: Developement, standardization, and administration manual. 7th ed. Fort Collins, Colorado USA: Three Star Press, Inc; 2010.
- Björkdahl A, Nilsson A, Grimby G, Sunnerhagen K. Does a short period of rehabilitation in the home setting facilitate functioning after stroke? A randomized controlled trial. Clin Rehabil 2006;20:1038–49.
- Crotty M, Giles L, Halbert J, Harding J, Miller M. Home versus day rehabilitation: A randomized controlled trial. Age Ageing 2008;37:628–33.
- Hofstad H, Naess H, Moe-Nilssen R, Skouen J. Early supported discharge after stroke in Bergen (ESD Stroke Bergen): A randomized controlled trial comparing rehabilitation in a day unit or in the patients’ homes with conventional treatment. Int J Stroke 2013;8:582–7.
- Bernspäng B. Rater calibration stability for the assessment of motor and process skills. Scand J Occup Ther 1999;6:101–9.
- Kirkley K, Fisher A. Alternate forms reliability of assessment of motor and process skills. J Outcome Meas 1999;3:53–70.
- Bernspäng B, Fisher A. Differences between persons with right or left cerebral vascular accident on the assessment of motor and process skills. Arch Phys Med Rehabil 1995;76:1144–51.
- Rexroth P, Fisher A, Merritt B, Gliner J. ADL differences in individuals with unilateral hemispheric stroke. Can J Occup Ther 2005;72:212–21.
- Dickerson A, Fisher A. Age differences in functional performance. Am J Occup Ther 1993;47:686–92.
- Duran L, Fisher A. Male and female performance on the assessment of motor and process skills. Arch Phys Med Rehabil 1996;77:1019–24.
- Merritt B, Fisher A. Gender differences in the performance of activities of daily living. Arch Phys Med Rehabil 2003;84:1872–7.
- Fisher A, Jones K. Assessment of motor and process skills volume 2: User MANUAL. 7th ed. Fort Collins, Colorado, USA: Three Star Press, Inc; 2010.
- Merritt B. Utilizing AMPS ability measures to predict level of community dependence. Scand J Occup Ther 2010;17:70–6.
- Wilson J, Hareendran A, FGrant M, Baired T, Schulz U, Muir K, et al. Improving the assessment of outcomes in stroke: Use of a structured interview to assign grades on the modified Rankin Scale. Stroke 2002;33:2243–6.
- Thomassen L, Waje-Andreassen U, Naess H, Elvik M, Russell D. Long-term effect of intravenous thrombolytic therapy in acute stroke: Responder analysis versus uniform analysis of excellent outcome. Cerebrovasc Dis 2005;20:470–4.
- Aasebø K, Rørlien K, Hauken J, Kupca A, Lindås L, Myklebust S. [Report from a developement project. Day- and outreach rehabilitation. A sub-project of "Early supported discharge after stroke in Bergen"] Rapport fra et utviklingsprosjekt. Dag- og oppsøkende rehabilitering. Delprosjekt i Slagbehandlingskjede-Bergen 2009–2011. Bergen Kommune: 2011.
- Gjelsvik B, Hofstad H, Smedal T, Eide G, Næss H, Skouen J, et al. Balance and walking after three different models of stroke rehabilitation: Early supported discharge in a day unit or at home, and traditional treatment (control). BMJ Open 2014;4:e004358.
- Thomassen L, Waje-Andreassen U, Næss H, Brøgger J. Treatment of cerebrovascular disease in a comprehensive stroke unit [Behandling av cerebrovaskulære sykdommer i slagenhet]. Tidsskr Nor Laegeforen 2011;8:819–23.
- Hoffman T, McKenna K, Cooke D, Tooth L. Outcomes after stroke: Basic and instrumental acctivities of daily living, community reintegration and generic health status. Aust Occup Ther J 2003;50:225–33.
- Weimar C, Ziegler A, König I, Diener H. Prediciting functional outcome and survival after acute ischemic stroke. J Neurol 2002;249:888–95.
- Appelros P, Jonsson F, Åsberg S, Asplund K, Glader E, Åsberg K, et al. Trends in stroke treatment and outcome between 1995 and 2010: Observations from Riks-stroke, the swedish stroke register. Cerebrovasc Dis 2014;37:22–9.
- European Stroke Organisation (ESO), European Society for Minimally Invasive Neurological Theraphy (ESMINT), European Society of Neuroradiology (ESNR). Consensus statement on mechanical thrombectomy in acute ischemic stroke. ESO-Karolinska Stroke Update 2014; November 16–18; Stockholm. 2014.
- Sunnerhagen K, Danielsson A, Rafsten L, Björkdahl A, Axelsson Å, Nordin Å, et al. Gothenburg very early supported discharge study (GOTVED) NCT01622205: A block randomized trial with superiority desgn of very early supported discharge for patients with stroke. BMC Neurol 2013;13:66.
- Ellekjær H, Selmer R. [Stroke - similar incidence, better prognosis] Hjerneslag - like mange rammes, men prognosen er bedre.]. Tidsskr Nor Laegeforen 2007;127:740–3.
- Feigin V, Forouzanfar M, Krishnamurthi R, Mensah G, Connor M, Bennett D, et al. Global and regional burden of stroke during 1990–2010: Findings from the Global Burden of Disease Study 2010. Lancet 2014;383:245–55.
- Dowswell G, Lawler J, Dowswell T, Young J, Forster A, Hearn J. Investigating recovery from stroke: A qualitative study. J Clin Nurs 2000;9:507–15.
- Tistad M, Ytterberg C, Tham K, von Koch L. Poor concurrence between disabilities as described by patients and established assessment tools three months after stroke: A mixed methods approach. J Neurol Sci 2012;313:160–6.
- Taule T, Strand L, Sture J, Råheim M. Striving for a life worth living: Stroke survivors’ experiences of home rehabilitation. Scand J Caring Sci 2015. doi:10.1111/scs.12193.
Supplementary material available online
Tables S1–S7