Abstract
Objectives: The significant improvement in the contraceptive prevalence rate in Kaduna State, Nigeria, from 8.4% in 2008 to 18.5% in 2013 is a notable achievement. This article analyses the role of midwives as drivers of reproductive health commodity security (RHCS) and their impact on contraceptive use in Kaduna State. Methods: The United Nations Population Fund (UNFPA) supported the bimonthly review resupply meetings facilitated by midwives at State and local government area (LGA) levels. The midwives deliver contraception to the LGAs for onward distribution to 6974 of the 25,000 health facilities across the country according to usage data from the previous 2 months. They also collect requisition, issue and resupply form data from the previous 2 months. Results: The active participation of midwives at the bimonthly meetings improved data timeliness by 23% and data completeness by 50% in 1 year. Only one health facility ran out of intrauterine devices and only 17% reported running out of female condoms. The total number of contraceptives issued increased from 31,866 in 2012 to 177,828 in 2013, resulting in a couple–year protection increase from 3408 in 2012 to 102,207 in 2013. Conclusions: Creation of increased demand and engagement of midwives in providing family planning services, especially long-acting contraceptive methods, coupled with the removal of cost to the user and the strengthening of the supply chain have been major factors in more than doubling the contraceptive prevalence rate.
Chinese abstract
目的:在尼日利亚卡杜纳州,避孕普及率有了显著提高,从2008年的8.4%升高到2013年的18.5%,是一项卓越的成就。本文分析卡杜纳州助产人员促进生殖健康商品安全(RHCS)的作用和他们对避孕的影响。方法:联合国人口基金会(UNFPA)支持由州和地方政府(LGA)级别的助产人员协助召开的两月一次的回顾补给会议。助产人员给地方政府提供避孕工具,根据近2个月的使用数据分配给全国25000个卫生机构中的6974个。他们也收集近2个月的征用、问题和补给表单数据。结果:在两月一次会议中主动参与的助产人员在1年中提高了23%的数据及时性和50%的数据完整性。仅有1个卫生机构用尽宫内节育器,仅有17%的卫生机构用尽女性避孕套。发放避孕药的总量从2012年的31,866增加到2013年的177,828,使每对夫妇年保护从2012年的3408增加到2013年的102,207。结论:增加需求量的创新和助产人员提供计划生育服务,尤其是长效避孕方法,加上免除使用者的费用和加强供应链,成为避孕普及率增加2倍以上的主要因素。
Introduction
Nigeria has a low contraceptive prevalence rate of 10% and a high unmet contraceptive need of 17.8%. Nigeria plans to achieve an annual 2% increase in contraceptive prevalence rate based on the current annual increment rate and additional investment in family planning services. The government aims to increase the contraceptive prevalence rate to 36% by the year 2018, in part by making contraception free of charge.
Kaduna State, located in north-west Nigeria, is the third most populous State in the country: its population in 2014 was estimated to be 7.7 million, based on projections from the 2006 national census.[Citation1] In 2008, Kaduna State’s poor reproductive health indicators, although better than most other northern Nigerian States, were worse than the national average (). Kaduna State had a low contraceptive prevalence rate of 8%, a correspondingly high total fertility rate of 6.3 and a teenage pregnancy rate of 32%.[Citation2] The 25% unmet need for family planning was higher than the national average of 17.8%. Poor contraceptive uptake significantly contributed to the State’s high maternal mortality ratio of 1025/100,000 live births reported in 2010.[Citation3] This figure is significantly higher than the national maternal mortality ratio average of 545/100,000 live births.[Citation2]
Table 1. Reproductive health indicators: Kaduna State vs. national data (2008).[Citation2]
The high unmet need for family planning, with its attendant consequences of low contraceptive prevalence rate, high total fertility rate, and high teenage pregnancy and birth rates, was mainly driven by the unavailability of contraceptives at service delivery points. Other contributory factors included the low exposure to family planning messages, religious and cultural hindrances, and unwillingness to pay for contraceptive services.[Citation4] The perennial unavailability of contraceptives at public facilities was largely due to insufficient funding for their procurement and distribution.
Nigeria ranked 152 on the 2013 Human Development Index,[Citation5] with a poverty rate of 33.1%. Recognising that Nigeria would not be able to meet Millennium Development Goal 5B of universal access to reproductive health services by 2015, the country realised the need to secure a supply of modern contraceptives and other life-saving commodities at the lowest possible cost or provide them free of charge to users. The federal government with the support of the reproductive health commodity security (RHCS) technical working group developed an RHCS strategic plan for 2011–2015 and subsequently took a significant policy decision in April 2011 of declaring contraceptives free of charge at all public health facilities. The strategic plan defined RHCS as existing when every person is able to choose, obtain and use quality contraceptives and other essential reproductive health products whenever he or she needs them. The policy decision was backed by funding totalling $6.7 million from the Nigerian government; the United Nations Population Fund (UNFPA); the UK Department for International Development; the Canadian Department of Foreign Affairs, Trade and Development; and the US Agency for International Development, to procure contraceptives for Nigeria. This ensured that an increased quantity of contraceptive products would be procured and distributed among a greater number of public health facilities.
Other providers of family planning services and information were also involved: Marie Stopes Nigeria, Phase II of the Partnership for Transforming Health Systems, the Nigerian Urban Reproductive Health Initiative, the Society for Family Health, and the Planned Parenthood Federation of Nigeria. These bodies were involved in training frontline health workers, procuring additional contraceptives, and developing guidelines to create demand for family planning, change behaviour through social marketing, and distribute tasks among health care teams.
Rationale for intervention
Despite the availability of contraceptives at Nigeria’s central warehouse in the port city of Lagos, no budget was earmarked for their distribution from the warehouse to the service delivery points across the country. UNFPA, as the sole procurement agent for contraceptives in Nigeria, and to assist the federal government to meet its target of increasing the contraceptive prevalence rate to 36% by 2018, supported the distribution of contraceptives from the warehouse to the States and from the States to over 7000 public health facilities in the country ().
Figure 1. Contraceptive distribution channels in Nigeria. C: client; CBD: community-based distribution; FMOH: Federal Ministry of Health; Int’l NGO: international non-governmental organisation; IPPF: International Planned Parenthood Federation; NGO: non-governmental organisation; NGO SDP: non-governmental organisation service delivery point; PPFN: Planned Parenthood Federation of Nigeria.[Citation6] Source: Nigeria Reproductive Health Commodity Security Strategic Plan 2011–2015.
![Figure 1. Contraceptive distribution channels in Nigeria. C: client; CBD: community-based distribution; FMOH: Federal Ministry of Health; Int’l NGO: international non-governmental organisation; IPPF: International Planned Parenthood Federation; NGO: non-governmental organisation; NGO SDP: non-governmental organisation service delivery point; PPFN: Planned Parenthood Federation of Nigeria.[Citation6] Source: Nigeria Reproductive Health Commodity Security Strategic Plan 2011–2015.](/cms/asset/d18c78ed-d44c-477b-a139-a8f4e178482e/iejc_a_1137280_f0001_c.jpg)
Methods
Since 2012, UNFPA has supported the distribution of contraceptives to 34 of the 36 States in Nigeria and the Federal Capital Territory. State level distribution is done by adopting the USAID Deliver project’s ‘push’ model of distribution from the States through the local government areas (LGAs) to service delivery points arranged in clusters, termed review resupply meetings.
All 23 LGAs in Kaduna State are grouped into six clusters each consisting of between two and four LGAs. The review resupply meetings for each cluster take place at one of the service delivery points located in the host LGA, which is usually the most accessible LGA within the cluster. The bimonthly meetings are attended by all LGA reproductive health coordinators and family planning service providers from the host LGA and from two to three neighbouring LGAs within the cluster. The State team, consisting of the State family planning coordinator, the State reproductive health coordinator, the State monitoring and evaluation officer, and the State commodity store officer, conveys all types of available commodities to the LGAs for distribution at the meetings.
The meetings are facilitated largely (87%) by midwives, consisting of the State reproductive health coordinator, the State family planning coordinator and the reproductive health coordinator of the participating LGAs. At these meetings, each LGA reproductive health coordinator, with the support of a State team member, counts the stock at each service delivery point with the service provider, reviews the commodity records (registers; daily consumption records/tally cards; and requisition, issue and resupply forms) and issues commodities based on the consumption records and actual physical stock count. The LGA reproductive health coordinator then compiles the records of all service delivery points in the LGA and provides a summary to the State family planning coordinator. The State family planning coordinator collects, reviews and collates the requisition, issue and resupply form data of the previous 2 months for all the LGAs in the State for onward transmission to the Federal Ministry of Health. The stock of each LGA is then replenished according to its consumption data. Each LGA reproductive health coordinator provides family planning commodities to the service delivery point guided by its current consumption data.
Feedback is subsequently provided to the service providers on their performance. The forum is also used as an opportunity to engage service providers and reproductive health coordinators in discussions about programme developments and share good practices related to service provision. This distribution model requires relatively little investment. Essentially, the only requirement is an hourly wage and a transportation allowance for travel to and from the meeting locations. The success of this best practice is exemplified in Kaduna State, Nigeria.
Results
Increase in use of family planning methods
Between 2011 and 2013, consumption records at the State’s central contraceptive store indicated a trend of increasing consumption of all types of contraception. This trend was reflected by a significant increase reported in the national database in the number of people accessing contraception at service delivery points.[Citation7] In Kaduna State, the total number of people who received contraception from a public facility increased from 139,051 in 2012 to 208,850 in 2013[Citation7,Citation8] ().
Figure 2. Number of people accessing contraception in Kaduna State, Nigeria.[Citation7]
![Figure 2. Number of people accessing contraception in Kaduna State, Nigeria.[Citation7]](/cms/asset/47ff1a87-bb1b-4c16-8ac9-616aac8b1634/iejc_a_1137280_f0002_b.jpg)
Increases in the number of contraceptives distributed were greater for long-acting reversible contraception (LARC), including the subdermal etonogestrel and levonorgestrel implants and the copper-releasing intrauterine device (IUD). In 2012, only 32 health facilities in the State provided LARC methods for family planning. With the increase in availability of LARC methods since 2013, 96 health facilities have offered LARC as part of their family planning service. Method-specific records from Kaduna State’s contraceptive store showed that only 874 implants were distributed to health facilities across the State in 2011; this figure rose to 2238 in 2012 and it more than tripled in 2013 to reach 7884. The number of IUDs distributed almost doubled between 2011 and 2013 (from 1274 in 2011 to 2166 in 2013). The demand for injectable contraceptives also increased across the State from 56,304 in 2011 to 89,400 in 2013. The couple–year protection for all types of contraception increased from 3408 in 2012 to 102,207 in 2013 ().
Table 2. Progress of the contraceptive distribution model: 2012 vs. 2013.[Citation6]
Reduction in stock unavailability
Regular resupply of contraceptives to each service delivery point has proven that strengthening distribution to service providers via midwives at State and LGA levels significantly reduces stock unavailability. The UNFPA’s 2013 Global Programme to Enhance Reproductive Health Commodity Security (GPRHCS) survey reported that the average rate of stock unavailability in Kaduna State was 24.1%, which is an improvement from 30% in 2012.[Citation8] Indeed, there was almost no unavailability of IUDs, and only 17% of service delivery points reported unavailability of the female condom.
Improvement in reporting rates
In 2012, bimonthly data for requisition, issue and resupply form reports showed that timeliness stood at about 10% and completeness at less than 50%. These figures improved in 2013 to 33% for timeliness and 100% for completeness. Data quality also gradually improved, as 80% of the requisition, issue and resupply forms received in 2013 were original copies, as requested.
Rise in contraceptive prevalence rate
The investments made in ensuring the availability of contraceptives at service delivery points to meet demand have shown very positive results. Kaduna State’s contraceptive prevalence rate rose more than twofold between 2008 and 2013 (). According to the 2013 Nigeria Demographic and Health Survey,[Citation4] the contraceptive prevalence rate for modern contraceptives in Kaduna State rose from 8.4% in 2008 to 18.5% in 2013, which was above the national average of 9.8% and the regional average for north-west Nigeria of only 3.6%. A corresponding drop in total fertility rate, from 6.3 in 2008 to 4.1 in 2013, was also seen, which is below the national average of 5.5. The unmet need for family planning declined to 5% in 2013 from 25% in 2008.
Discussion
Findings and interpretation
There was a 50% increase in family planning uptake between 2012 and 2013. This figure consists of both new users and those requesting resupply. Several studies have attested to the key role of nurses in providing guidance and effective counselling to women seeking contraception, resulting in an increased uptake of contraceptive methods.[Citation10,Citation11] The engagement of midwives has been reported to significantly increase the use of every contraceptive method except injectables.[Citation10] Midwives with years of experience are perfectly suited to providing family planning services and information on the benefits and disadvantages of different contraceptive methods. They are able to address myths and misconceptions and are preferred providers by female clients.[Citation11]
The 200% increase in the number of health facilities providing LARC was facilitated by: (i) the availability of trained midwives; (ii) massive promotional campaigns conducted by various agencies such as UNFPA, Marie Stopes Nigeria, and the Nigerian Urban Reproductive Health Initiative; and (iii) the government policy of providing free family planning. In Ethiopia, the involvement of health extension workers increased the percentage of service delivery points offering at least three methods of modern contraception by 30% within 3 years.[Citation12] This is corroborated by reproductive health interventions in Sudan which engaged midwives as community mobilising agents and successfully promoted IUDs and implants among rural women.[Citation13]
Method-specific records from the Kaduna State contraceptive store from 2011 to 2013 indicated an increase, respectively, of 802%, 70% and 59% for implants, IUDs and injectables distributed to health facilities. These records are evidence of increased demand by new users, as distribution was guided by the previous 2 months’ consumption data from the health facilities.
The new approach reduced stock unavailability from 30% to 24.1% within the space of a year. A similar family planning outreach programme facilitated by health extension workers in Ethiopia also produced a dramatic reduction in stock unavailability.[Citation12] Stock is supplied bimonthly to service providers during review resupply meetings, thereby eliminating the logistical challenges of resupply from the State contraceptive store (). Nevertheless some items were at times unavailable in some facilities when service providers were absent during meetings. Also, the meetings were not conducted as regularly as scheduled, due to inadequate distribution funding, which is presently mainly provided by donors.
Figure 4. Process of bimonthly review and resupply meetings. FP: family planning; FPC: family planning coordinator; FPS: family planning service; M&E: monitoring and evaluation officer; NHMIS: National Health Management Information System; RHC: reproductive health coordinator; RIRF: requisition, issue and report form.
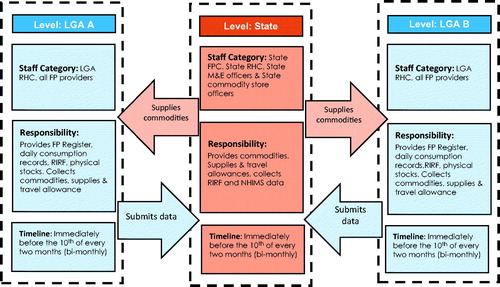
The 23% and 50% increases in data reporting for timeliness and completeness were due to the presence of midwives (87% of LGA reproductive health coordinators are midwives) at the bimonthly cluster meetings supported by the LGA monitoring and evaluation officers. All family planning use data that were normally expected to be submitted at LGA level by the first week of the new month in accordance with the National Health Management Information System were collected at these meetings. The collected data were reviewed at the meetings before the stock was replenished. The team also ensured that data were supplied on the original copies of the triplicate requisition, issue and resupply forms instead of on the duplicate copies sometimes submitted by providers. This ensures the availability of clear, readable data for entry at State level. Ideally, the provision of sound family planning information, services and record maintenance are key responsibilities of a midwife.[Citation14]
The 10.5% increase in the contraceptive prevalence rate, the 20% reduction in unmet contraceptive need and the 2.2 reductions in the total fertility rate over the space of 5 years are evidence of the impact of the new approach and of other demand creation interventions enabled by the new policy environment. Other studies have reported a similar reduction in family size and increase in couple–year protection following the engagement of midwives in family planning services in health care centres.[Citation10] In Ethiopia, the involvement of health extension workers increased the contraceptive prevalence rate from 14% to 30% in 4 years.[Citation12] In Iran, increased community participation consequent to the involvement of rural midwives and other stakeholders resulted in a 64% decline in total fertility rate between 1986 and 2000.[Citation15]
The rise in contraceptive prevalence rate and drop in total fertility rate in Kaduna State can be attributed to the improved availability of contraceptives provided in all public health facilities at no cost to the user by the Federal Government of Nigeria and its partner agencies. This followed a decade-long drive to increase numbers of all health workers, including doctors, nurse/midwives, community health extension workers and community-based distribution agents, by UNFPA, Phase II of the Partnership for Transforming Health Systems, and Marie Stopes Nigeria, in addition to the massive demand creation, especially for LARC, by the Nigerian Urban Reproductive Health Initiative and the Society for Family Health.
Strength and weaknesses of the programme
The strength of the results lies in the fact that the evidence was derived from standard data sources such as the National Health Management Information System, the Nigeria Demographic and Health Surveys and the GPRHCS survey, supplemented by routine family planning data collected at the service delivery points and from the bimonthly requisition, issue and resupply forms. Nevertheless, some minimal data entry errors, incomplete data and over-reporting cannot be completely ruled out. Also, contributions from parallel measures to create demand and improve access taken during the same period cannot be underestimated.
Similarities and differences in results and conclusions
Our results are similar to the achievements reported from various other countries funded by the GPRHCS.[Citation16] The GPRHCS provides a framework for assisting countries in planning to meet their own contraceptive needs. Continuous, long-term support provided by UNFPA has helped to move countries towards more predictable, planned and sustainable self-driven approaches to securing and using essential maternal health supplies. A range of activities are carried out in response to each country’s situation, e.g., policy advocacy, supply and procurement system strengthening, and demand creation.
The engagement of midwives at various levels of programme management and service provision to improve contraceptive supply has proven to be effective. This is because as frontline health workers they also understand the complexities surrounding, and the interrelationships between, logistics management, clinical service provision, record keeping, and availability of these essential commodities to users.
Relevance of the findings: implications for clinicians and policy-makers
The results have highlighted the need to expand the role of midwives from providing clinic services to taking leadership in overhauling the poor logistics practices of contraceptive supply in their State and LGA.
Unanswered questions and future research
Some grey areas which require further research include the effect of the quality of counselling provided to clients and their ability to make informed choices free from coercion. There is also the need to establish the effect of motivation, including recognition and reward, on the performance of staff and their role in improving access to quality family planning methods. Also, further elucidation is needed of the effect of other ongoing family planning interventions such as the establishment of a technical working group, supportive supervision, the government policy of free family planning and maternal and child health services, and the introduction of channel management software to strengthen the logistics management system. Such confounding interventions were reported in Sierra Leone to result in a 28% improvement in stock availability, an increased number of contraceptive users in 1 year, and a 3% improvement in contraceptive prevalence rate in 3 years.[Citation17]
Conclusions
The use of midwives to anchor the review resupply meetings for distributing contraceptives has increased the number of individuals accessing family planning services, increased overall contraceptive consumption, reduced rates of stock unavailability at service delivery points and improved RHCS in Kaduna State. These improvements have contributed to a doubling of the State’s contraceptive prevalence rate figure in a similar manner to the Ethiopian experience.[Citation12] In the long term, it will be interesting to see the corresponding changes in total fertility rate, teenage pregnancy rate and maternal mortality ratio as a result of the increased contraceptive prevalence rate and overall strengthening of RHCS in Kaduna State.
Acknowledgements
The authors acknowledge the monitoring and evaluation analyst of UNFPA Nigeria, Yinka Akibu, for his input in the production of Figure 4.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 2006 Population and Housing Census of the Federal Republic of Nigeria. National and State Population and Housing Tables. Priority Tables Volume 1. Abuja: National Population Commission 2009.
- National Population Commission, Federal Republic of Nigeria, Abuja, Nigeria. Nigeria Demographic and Health Survey 2008. Calverton (MD): ICF Macro 2009.
- Kaduna State Government. Strategic Health Development Plan 2010–2015. Kaduna: Kaduna State Ministry of Health 2010.
- National Population Commission, Federal Republic of Nigeria, Abuja, Nigeria. Nigeria Demographic and Health Survey 2013. Rockville (MD): ICF International 2014.
- UNDP Nigeria Annual Report 2014 [Internet; cited 2015 Jul 1]. Available from: www.ng.undp.org/content/nigeria/en/home/library/human_development/undp-nigeria-annual-report-2014.
- USAID. Nigeria: Reproductive Health Commodity Security Situation Analysis [Internet; cited 2015 Dec 6]. Available from: deliver.jsi.com/dlvr_content/resources/allpubs/country.
- Federal Ministry of Health. National Health Management Information System [Internet; cited 2015 Jul 2]. Available from: DHIS2nigeria.org.ng.
- Federal Republic of Nigeria, UNFPA. Facility Assessment for Reproductive Health Commodities and Services in Nigeria: 2013 Survey Report. 2014.
- Federal Republic of Nigeria. Nigeria Multiple Indicator Cluster Survey 2011. National Bureau of Statistics, Abuja, Nigeria. 2013.
- Jabbari H, Bakhshian F, Velayati A, et al. Effectiveness of presence of physician and midwife in quantity and quality of family planning services in health care centers. J Family Community Med. 2014; 21:1–5.
- Andriamasy BE. Midwives deliver family planning in Madagascar [Internet; cited 2015 Jun 30]. Available from: http://mariestopes.org/news/midwives-deliver-family-planning-madagascar.
- UNFPA. Ethiopia: Health workers expand access to modern methods. Recent Success Stories in Reproductive Health Commodity Security [Internet; cited 2015 Jun 30], Available from: www.myaccessrh.org/documents/10157/2bca0a44-be2e-480e-97ad-3670b83c5d0e.
- DKT Sudan. White paper. Ensuring the right for all to quality family planning options since 2005 [Internet; cited 2015 Jun 30]. Available from: http://www.dktinternational.org/publications-resources/newsletters/.
- Roles and responsibilities of a midwife [Internet; cited 2015 Jun 26]. Available from: tiger.library.dmu.ac.uk/bitstream/handle/123456789/52/Roles%20and%20responsibilities%20of%20the%20Midwife%20NMC.pdf?sequence=43.
- Vahidnia F. Case study: fertility decline in Iran [Internet]. Popul Envir 2007 [cited 2015 Jul 1];28:259–66. Available from: www.researchgate.net/publication/225748815_Case_study_fertility_decline_in_Iran.
- UNFPA. Preface. Recent Success Stories in Reproductive Health Commodity Security [Internet; cited 2015 Jun 30]. Available from: www.myaccessrh.org/documents/10157/2bca0a44-be2e-480e-97ad-3670b83c5d0e.
- UNFPA. Sierra Leone: Managing RHCS data more effectively. Recent Success Stories in Reproductive Health Commodity Security [Internet; cited 2015 Jun 30]. Available from: www.myaccessrh.org/documents/10157/2bca0a44-be2e-480e-97ad-3670b83c5d0e.

![Figure 3. Trends in contraceptive prevalence rate in Kaduna State, Nigeria. DHS: Demographic and Health Survey;[Citation2,Citation4] MICS: multiple indicator cluster.[Citation9]](/cms/asset/e4a4ff9e-d0a5-46c0-9afd-a4ae8a24beea/iejc_a_1137280_f0003_c.jpg)