ABSTRACT
Background
Older people with intellectual disability (ID) are at high risk of incidents leading to hospital visits.
Method
Through national registers, 7936 people with ID, aged 55+ years in 2012, and a same-aged referent cohort from the general population were identified. Information on diagnoses made in inpatient and outpatient specialist health care during 2002–2012 was collected.
Results
Compared to their age-peers in the general population, people with ID were 41% more likely to seek care for effects of foreign body entering through natural orifice, and 92% more for poisoning by drugs, medicaments and biological substances.
Conclusions
There is a need to develop and evaluate evidence-based interventions to prevent unnecessary suffering and early death related to poisoning or respiratory diseases among older people with ID. To do this, implementation of risk assessments and increased knowledge of the consequences of poisoning and incidents of foreign bodies entering the respiratory organs are necessary.
People who have a cognitive impairment are less able to recognise and avoid risk (Greenspan, Switzky, & Woods, Citation2011), and thereby have an increased risk of incidents. Intellectual disability (ID) is characterised by significant limitations in intellectual functioning and adaptive behaviour (Schalock et al., Citation2007), and adults with ID have been found to have a higher rate of injury than people from the general population (Petropoulou et al., Citation2016). Also, “injury, poisoning, and certain other consequences of external causes” is the most common diagnostic group for hospitalisation among people with ID (Skorpen, Nicolaisen, & Langballe, Citation2016). Even so, injury prevention in this group has not been addressed to the extent that the magnitude of the problem requires (Finlayson, Jackson, Mantry, Morrison, & Cooper, Citation2015; Sherrard, Ozanne-Smith, & Staines, Citation2004).
As aging is associated with cognitive impairment, older people with ID comprise a group at especially high risk of injuries and incidents. At the same time, they comprise a group where preventive measures may have a large impact. However, in order to implement such preventive measures it is necessary to determine types of incidents experienced by older people with ID, as well as risk factors for them.
The aim of this study was to compare occurrence of incidents leading to inpatient and outpatient specialist health care between older people with ID and their age-peers in the general population. Also, to investigate possible associations between type and severity of ID on one hand, and injuries and incidents on the other, among older people with ID. We use the term “incident” rather than “accident” to emphasise that the situations causing them are avoidable – they do not just happen.
Methods
This study is part of a project that has been described in detail elsewhere (Axmon, Björne, Nylander, & Ahlström, Citation2016; Sandberg, Ahlström, Axmon, & Kristensson, Citation2016). Briefly, the Swedish LSS register was used to identify all people with at least one measure of support for people with ID in 2012, aged at least 55 years and alive at the end of that year (ID cohort, n = 7936). Statistics Sweden provided a referent cohort from the general population (gPop cohort), one-to-one-matched by sex and year of birth. Within the ID cohort, we identified 1154 people (15%) with at least one diagnosis of ID (F7 in ICD-10) during the study period (2002–2012). These were categorised as having mild (n = 614, corresponding to 53% of those with ID diagnosis), moderate (n = 285, 25%), or severe/profound ID (n = 255, 22%). We also identified 472 people (6% of total) with at least one diagnosis of Down Syndrome (DS) during the study period.
We used the Swedish National Patient Register to identify all people in both cohorts with inpatient or outpatient specialist health care (healthcare episode) with a diagnosis in any of the ICD-10 (International Statistical Classification of Diseases and Related Health Problems 10th Revision) blocks T15–T19 (effects of foreign body entering through natural orifice), T20–T32 (burns and corrosions), T33–T35 (frostbite), T36–T50 (poisoning by drugs, medicaments, and biological substances), and T51–T65 (toxic effects of substances chiefly nonmedicinal as to source) during 2002–2012. Unless otherwise mentioned, diagnoses were aggregated to “present” or “absent” for each block. Thus if a patient was diagnosed with burn and corrosion of both head and neck (T20) and trunk (T21) during the same healthcare episode, a diagnosis in the diagnostic block burns and corrosions (T20–T32) was considered present. Using logistic regression, we estimated the odds ratio (OR) with the 95% confidence interval (CI) for the ID cohort versus the gPop cohort for having each outcome at least once during the study period. Analyses were only performed if each group to be compared comprised at least five observations. P-values less than 0.05 were considered statistically significant.
Results
Effects of foreign body entering through natural orifice
People in the ID cohort were more likely than those in the gPop cohort to have effects of foreign body entering through natural orifice ( and ). Among those with at least one such diagnosis, 70% in the ID cohort and 76% in the gPop cohort had only one. Considering all single diagnoses (i.e., not aggregating to block level but allowing for multiple diagnoses within the same diagnostic block at the same visit), the most common diagnosis in the ID cohort was foreign body in oesophagus (T18.1), which corresponded to 45% (n = 122) of all diagnoses in this block, and was recorded at least once for 77 people in the ID cohort. This was followed by foreign body in unspecified part of the ear (T16.9; diagnoses: 11%, n = 29; people: n = 17), pharynx (T17.2; 9%, n = 24; n = 21), bronchus (T17.5; 8%, n = 22; n = 12), nostril (T17.1; 6%, n = 17; n = 8), and respiratory tract, part unspecified (T17.9; 4%, n = 12; n = 8). All other diagnoses were recorded fewer than 10 times in the ID cohort.
Figure 1. Percentage of people with at least one healthcare episode due to effects of foreign body entering through natural orifice in a cohort of older people with intellectual disability (ID), including Down Syndrome (DS), and a referent cohort from the general population (gPop).
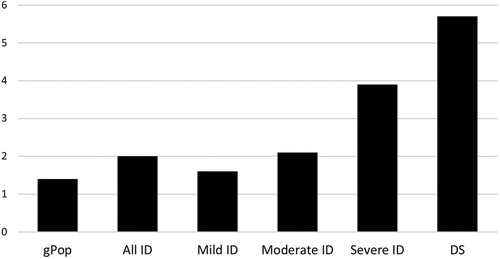
Table 1. Diagnoses of injuries, poisoning, and incidents in a cohort of 7936 older people with intellectual disability (ID) and a referent cohort from the general population (gPop), one-to-one-matched by sex and year of birth.
Within the ID cohort, 10 (1.6%) people with mild ID experienced 20 healthcare episodes due to effects of foreign body entering through natural orifice, 6 (2.1%) with moderate ID experienced 8 such visits, and 10 (3.9%) with severe/profound ID 13 visits (). There was no statistically significant difference between those with mild and moderate ID (OR for moderate vs. mild 1.29, 95% CI 0.47–3.59), but those with severe/profound ID had an increased risk compared to those with mild ID (OR 2.45, 95% CI 1.01–6.97). As in the total ID cohort, the most common single diagnosis at each level of severity was foreign body in the oesophagus (T18.1).
We found 41 healthcare episodes for 27 (5.7%) people with DS compared to 211 visits for 133 (2.2%) people without DS (OR 2.70; 95% CI 1.76–4.13; ). Again, the most common single diagnosis was foreign body in the oesophagus (T18.1).
Poisoning by drugs, medicaments, and biological substances
Poisoning by drugs, medicaments, and biological substances was almost twice as likely in the ID cohort as in the gPop cohort (). Among those with at least one such diagnosis, 83% in the ID cohort and 79% in the gPop cohort had only one. Considering all single diagnoses, that is, not aggregating on block level, the most common in the ID cohort was other and unspecified substances (T50.9; 77%, n = 76; n = 47). No other diagnosis was recorded more than 5 times in the ID cohort.
Within the ID cohort, 11 (1.8%) people with mild ID experienced 17 healthcare episodes due to poisoning, the most common one being by other and unspecified drugs, medicaments, and biological substances (T50.9). The number of healthcare episodes among those with moderate or severe/profound ID was fewer than 5 in each group.
Five (1.1%) people with DS had one healthcare episode each due to poisoning, compared to 73 healthcare episodes for 60 (1.0%) people without DS (OR 1.07, 95% CI 0.43–2.67). Similar to the whole ID cohort, the most common single diagnosis among people with DS was poisoning by other and unspecified drugs, medicaments, and biological substances (T50.9).
Other incidents
No single diagnosis in the blocks burns and corrosions (T20–T32) and toxic effects of substances chiefly nonmedicinal as to source (T51–T65) was recorded at more than five healthcare episodes in the ID cohort. Frostbites were experienced by fewer than 5 people in each cohort and data regarding this diagnosis are therefore not presented.
Discussion
Although the number of incidents leading to healthcare episodes was low, both among older people with ID and in the general population, older people with ID had increased risk of seeking inpatient and outpatient specialist health care for effects of foreign body entering through natural orifice as well as for poisoning by drugs, medicaments, and biological substances.
Previous studies regarding incidents among older people with ID have mainly focused on fall-related injuries (Axmon, Ahlström, & Sandberg, Citation2018; Axmon, Sandberg, Ahlström, & Midlöv, Citation2018; Enkelaar, Smulders, van Schrojenstein Lantman-de Valk, Weerdesteyn, & Geurts, Citation2013; Smulders, Enkelaar, Weerdesteyn, Geurts, & van Schrojenstein Lantman-de Valk, Citation2013), which is not surprising, as fractures are the most common cause of hospitalisation among diagnoses of injury, poisoning, and certain other consequences of external causes (Skorpen et al., Citation2016). Indeed, to the best of our knowledge, only one previous study has assessed poisonings and objects stuck in part of body (Finlayson, Morrison, Jackson, Mantry, & Cooper, Citation2010). They found increased risk of poisoning compared to the general population, but – in contrast to our study – no difference regarding object stuck in part of body. This discrepancy may be explained by differences in the definitions of outcomes, as Finlayson et al. (Citation2010) did not include food. However, in the general adult population, food is the most common reason for emergency department visits for complaints related to swallowing or choking (Erbil et al., Citation2013). Also, whereas our study was register-based, Finlayson et al. (Citation2010) used self-reported data.
Risk assessments may be a way of reducing incidents among people with ID (Finlayson et al., Citation2010). These should consider potentially underlying causes, such as dysphagia, that is, difficulties in eating, drinking, or swallowing. Dysphagia affects many older persons because of degenerative processes in mouth, throat, and nerves (Sura, Madhavan, Carnaby, & Crary, Citation2012), and is also a common condition among people with ID (Chadwick & Jolliffe, Citation2009; Robertson, Chadwick, Baines, Emerson, & Hatton, Citation2017). Consequently, it is not an unlikely contributing cause for the increased risk of healthcare episodes due to effects of foreign body entering through natural orifice, specifically those with foreign body in the digestive or respiratory tract. Thus a potential way to reduce this type of incidents may be to adjust the texture of food, for example, by mashing or thickening it. It is also important for staff and other carers to be vigilant when feeding.
Respiratory disease is one of the most common cause of death among people with ID and DS (Englund, Jonsson, Zander, Gustafsson, & Anneren, Citation2013; Ng, Flygare Wallén, & Ahlström, Citation2017), with pneumonia and pneumonitis due to solids or fluids, or both ranking high within this diagnostic group. Thus knowledge regarding a potential association between incidents in the respiratory organs and serious consequences such as pneumonia and death is needed.
Polypharmacy is more common among older people with ID than among older people in the general population (Peklar et al., Citation2017). Consequently, drug–drug interactions are more likely to occur among older people with ID and may thus be a cause of poisonings in this group. Moreover, antipsychotics are common among older people with ID (Axmon, Sandberg et al., Citation2018; O'Dwyer et al., Citation2017), and adverse events are frequent among people with ID using antipsychotics (Scheifes et al., Citation2016). Thus poisonings may also be an adverse event related to use of antipsychotics.
Conclusion
Older people with ID have comparatively high frequencies of poisoning by drugs, medicaments, and biological substances as well as incidents involving foreign body in natural orifice, mainly in the respiratory organs. This frail group may be helped by a safer living environment, where risk assessments are incorporated in the daily living support. For those with poisoning and recurrent incidents, it is important to identify underlying causes. Annual reviews of medication may be one way to prevent poisoning. The necessity of safe oral intake of liquids and food among persons with ID is evident in order to reduce mortality and the need for health care. Consultations with, for example, dieticians and occupational therapists may support staff and carers to develop relevant and individualised interventions adapted to each person's health condition.
Acknowledgements
This work was funded by Forte, the Swedish Research Council for Health, Working Life and Welfare no. 2014-4753. The funding body has not imposed any restrictions on free access to or publication of the research data. All authors have contributed, seen, and approved of the manuscript and agree to the order of the authors as listed on the title page.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Axmon, A., Ahlström, G., & Sandberg, M. (2018). Falls resulting in health care among older people with intellectual disability in comparison with the general population. Journal of Intellectual Disability Research, doi: 10.1111/jir.12564
- Axmon, A., Björne, P., Nylander, L., & Ahlström, G. (2016). Psychiatric care utilization among older people with intellectual disability in comparison with the general population: A register study. BMC Psychiatry, 16(1), 389. doi: 10.1186/s12888-016-1094-0
- Axmon, A., Sandberg, M., Ahlström, G., & Midlöv, P. (2018). Fall-risk-increasing drugs and falls requiring health care among older people with intellectual disability in comparison with the general population: A register study. PLoS One, 13(6), e0199218. doi: 10.1371/journal.pone.0199218
- Chadwick, D. D., & Jolliffe, J. (2009). A descriptive investigation of dysphagia in adults with intellectual disabilities. Journal of Intellectual Disability Research, 53(1), 29–43. doi: 10.1111/j.1365-2788.2008.01115.x
- Englund, A., Jonsson, B., Zander, C. S., Gustafsson, J., & Anneren, G. (2013). Changes in mortality and causes of death in the Swedish Down syndrome population. American Journal of Medical Genetics. Part A, 161a(4), 642–649. doi: 10.1002/ajmg.a.35706
- Enkelaar, L., Smulders, E., van Schrojenstein Lantman-de Valk, H., Weerdesteyn, V., & & Geurts, A. C. (2013). Prospective study on risk factors for falling in elderly persons with mild to moderate intellectual disabilities. Research in Developmental Disabilities, 34(11), 3754–3765. doi: 10.1016/j.ridd.2013.07.041
- Erbil, B., Karaca, M. A., Aslaner, M. A., Ibrahimov, Z., Kunt, M. M., Akpinar, E., & Özmen, M. M. (2013). Emergency admissions due to swallowed foreign bodies in adults. World Journal of Gastroenterology, 19(38), 6447–6452. doi: 10.3748/wjg.v19.i38.6447
- Finlayson, J., Jackson, A., Mantry, D., Morrison, J., & Cooper, S. A. (2015). The provision of aids and adaptations, risk assessments, and incident reporting and recording procedures in relation to injury prevention for adults with intellectual disabilities: Cohort study. Journal of Intellectual Disability Research, 59(6), 519–529. doi: 10.1111/jir.12154
- Finlayson, J., Morrison, J., Jackson, A., Mantry, D., & Cooper, S. A. (2010). Injuries, falls and accidents among adults with intellectual disabilities. Prospective cohort study. Journal of Intellectual Disability Research, 54(11), 966–980. doi: 10.1111/j.1365-2788.2010.01319.x
- Greenspan, S., Switzky, H. N., & Woods, G. W. (2011). Intelligence involves risk-awareness and intellectual disability involves risk-unawareness: Implications of a theory of common sense. Journal of Intellectual & Developmental Disability, 36(4), 242–253. doi: 10.3109/13668250.2011.626759
- Ng, N., Flygare Wallén, E., & Ahlström, G. (2017). Mortality patterns and risk among older men and women with intellectual disability: A Swedish national retrospective cohort study. BMC Geriatrics, 17(1), 269. doi: 10.1186/s12877-017-0665-3
- O'Dwyer, M., Peklar, J., Mulryan, N., McCallion, P., McCarron, M., & Henman, M. C. (2017). Prevalence, patterns and factors associated with psychotropic use in older adults with intellectual disabilities in Ireland. Journal of Intellectual Disability Research, 61(10), 969–983. doi: 10.1111/jir.12391
- Peklar, J., Kos, M., O'Dwyer, M., McCarron, M., McCallion, P., Kenny, R. A., & Henman, M. C. (2017). Medication and supplement use in older people with and without intellectual disability: An observational, cross-sectional study. PLoS One, 12(9), e0184390. doi: 10.1371/journal.pone.0184390
- Petropoulou, E., Finlayson, J., Hay, M., Spencer, W., Park, R., Tannock, H., … Skelton, D. A. (2016). Injuries reported and recorded for adults with intellectual disabilities who live with paid support in Scotland: A comparison with Scottish adults in the general population. Journal of Applied Research in intellectual Disabilities, doi: 10.1111/jar.12244
- Robertson, J., Chadwick, D., Baines, S., Emerson, E., & Hatton, C. (2017). Prevalence of dysphagia in people with intellectual disability: A systematic review. Intellectual and Developmental Disabilities, 55(6), 377–391. doi: 10.1352/1934-9556-55.6.377
- Sandberg, M., Ahlström, G., Axmon, A., & Kristensson, J. (2016). Somatic healthcare utilisation patterns among older people with intellectual disability: An 11-year register study. BMC Health Services Research, 16(1), 642. doi: 10.1186/s12913-016-1880-x
- Schalock, R. L., Luckasson, R. A., Shogren, K. A., Borthwick-Duffy, S., Bradley, V., Buntinx, W. H. E., … Yeager, M. H. (2007). The renaming of mental retardation: Understanding the change to the term intellectual disability. Intellectual and Developmental Disabilities, 45(2), 116–124. doi: 10.1352/1934-9556(2007)45[116:Tromru]2.0.Co;2
- Scheifes, A., Walraven, S., Stolker, J. J., Nijman, H. L., Egberts, T. C., & Heerdink, E. R. (2016). Adverse events and the relation with quality of life in adults with intellectual disability and challenging behaviour using psychotropic drugs. Research in Developmental Disabilities, 49-50, 13–21. doi: 10.1016/j.ridd.2015.11.017
- Sherrard, J., Ozanne-Smith, J., & Staines, C. (2004). Prevention of unintentional injury to people with intellectual disability: A review of the evidence. Journal of Intellectual Disability Research, 48(Pt 7), 639–645. doi: 10.1111/j.1365-2788.2003.00570.x
- Skorpen, S., Nicolaisen, M., & Langballe, E. M. (2016). Hospitalisation in adults with intellectual disabilities compared with the general population in Norway. Journal of Intellectual Disability Research, doi: 10.1111/jir.12255
- Smulders, E., Enkelaar, L., Weerdesteyn, V., Geurts, A. C., & van Schrojenstein Lantman-de Valk, H. (2013). Falls in older persons with intellectual disabilities: Fall rate, circumstances and consequences. Journal of Intellectual Disability Research, 57(12), 1173–1182. doi: 10.1111/j.1365-2788.2012.01643.x
- Sura, L., Madhavan, A., Carnaby, G., & Crary, M. A. (2012). Dysphagia in the elderly: Management and nutritional considerations. Clinical Interventions in Aging, 7, 287–298. doi: 10.2147/CIA.S23404
