ABSTRACT
Background
Individuals with Down syndrome are an at-risk population for severe COVID-19 outcomes, due to genetic predispositions and comorbidities. The current study focused on differences between persons with and without Down syndrome regarding age and severity of disease.
Method
We used medical statistics to compare patients with and without Down syndrome who were admitted to Swiss hospitals (2020 and 2022) with a COVID-19 diagnosis. Differences in age, hospitalisation characteristics, mortality, and additional diagnoses were investigated.
Results
Results revealed a lower median age and greater risk of intensive care unit admission and mortality among patients with Down syndrome. No differences were found in length of hospital stay.
Conclusions
There is some evidence of increased vulnerability in people with Down syndrome compared to other patients, particularly in terms of mortality rates. However, compared to studies from other countries, the situation of people with Down syndrome does not appear to be particularly critical.
People with intellectual disabilities are particularly impacted by COVID-19 due to increased risk of infection, barriers in accessing and understanding information, and the risk of developing mental health problems (Bakaniene et al., Citation2023; Courtenay & Perera, Citation2020; Perera et al., Citation2020). However, the type and extent of vulnerability can vary widely between different types of disability, as each is associated with different comorbidities. In the present study, we focused on people with Down syndrome, as these people in Switzerland have been given a special status as a separate risk category during the pandemic (people with other disabilities sometimes had this status indirectly if they suffered from one of the listed pre-existing conditions). People with Down syndrome are assumed to be particularly at risk, due to their high prevalence of medical complications and genetic predispositions, which are thought to be related to an increased risk of severe disease progression (e.g., Bensussen et al., Citation2022; Capone et al., Citation2018; Espinosa, Citation2020; Illouz et al., Citation2021; Van Goor & Massa, Citation1997). On the other hand, individuals with Down syndrome also differ considerably in terms of their health and risk factors. Hence, the extent of vulnerability in people with Down syndrome, and whether certain life situations or genetic factors could in fact be protective, have not yet been thoroughly investigated.
In addition, national contexts that affect health care system quality and protective measures implementation during the pandemic varied widely, thus overall prognosis for at-risk groups may likewise vary strongly. To examine how people with Down syndrome were affected by COVID-19, we used medical statistics from Switzerland to examine their vulnerability based on characteristics of hospitalisation and disease progression.
Risk and protective factors related to Down syndrome
Previous studies have identified the most common comorbidities in people with Down syndrome (G. T. Capone et al., Citation2018; Illouz et al., Citation2021; Van Goor & Massa, Citation1997). These comorbidities include numerous risk factors for severe outcomes in COVID-19 (Centers of Diseases and Control Prevention, Citation2022), including obesity, cardiac and respiratory disease, and diabetes. Additional risk factors are increased prevalence of immune dysregulation caused by Trisomy 21 and other genetic specificities that facilitate infection with SARS-CoV-2 (Bensussen et al., Citation2022; Espinosa, Citation2020; Evangelho et al., Citation2022; Majithia & Ribeiro, Citation2022). Since these comorbidities are likely to be associated with more severe disease progression, it would be particularly important to minimise the risk of infection in this population. However, characteristics related to intellectual functioning and life circumstances may increase risk of infection. For example, it is more difficult for people with Down syndrome to understand and comply with protective measures such as mask wearing and physical distancing (Fujino & Itai, Citation2023). On the other hand, persons with Down syndrome who lived in social medical institutions were subject to more stringent protective measures than private households during the pandemic (e.g., Federal Office of Public Health, Citation2021b), thus, living situation could function as a protective factor for COVID-19 infection.
International studies indicate an overall increased vulnerability of individuals with Down syndrome to infection risk and disease severity, whereby there are large differences in the magnitude of vulnerability. With regard to the risk of infection, the state of research is not consistent. Some genetic predispositions in Down syndrome that favour inflammatory processes would suggest increased susceptibility to infection (Bensussen et al., Citation2022; Majithia & Ribeiro, Citation2022). Yet there also exist immune responses in Down syndrome that are theorised to inhibit infection and thus prevent disease progression (Altable & de la Serna, Citation2021; De Toma & Dierssen, Citation2021). Similarly, the state of research on the risk of infection is not consistent. One study based on medical statistics from England provides evidence that, compared to typically developing people, individuals with Down syndrome are proportionally more likely to become infected with COVID-19 (Baksh et al., Citation2022). Yet another study from Israel (Illouz et al., Citation2021), which used a comparable design, did not find a significant difference between the two populations, even though this study examined a larger sample. The authors assumed that these results might be related to the strict protective measures in Israel.
In addition to the risk of infection, there are some indications that individuals with Down syndrome are at higher risk for severe disease progression compared to those without Down syndrome. For example, medical statistics from Brazil, Iran, and the United States have shown that people with Down syndrome are more likely to require intensive care unit (ICU) treatment and to receive invasive mechanical ventilation (Boschiero, Lutti Filho, et al., Citation2022; Emami et al., Citation2021; Malle, Gao, et al., Citation2021). These findings could be related to the fact that people with Down syndrome are more susceptible to pulmonary diseases. For example, a retrospective study showed that 25% of adults with Down syndrome admitted to hospital between 1997 and 2014 were diagnosed with obstructive pulmonary disease (Aparicio et al., Citation2023). A similar study, which examined patients with Down syndrome over a period of 28 years, found a strongly increased tendency to pneumonia (11.19%) compared to an age- and gender-matched control group (3.18%; Chicoine et al., Citation2021). There is also evidence that sepsis resulting from COVID-19 infection is more common in people with Down syndrome compared to people without Down syndrome (Malle, Gao, et al., Citation2021). Individuals with Down syndrome are also at significantly increased risk of mortality following hospitalisation with COVID-19, with the observed increase in risk varying from approximately two to ten times (Boschiero, Lutti Filho, et al., Citation2022; Boschiero, Palamim, et al., Citation2022; Clift et al., Citation2021; Emami et al., Citation2021). Furthermore, people with Down syndrome who died from COVID-19 were younger and presented a higher incidence of superinfections, autoimmune disease, obesity, and dementia, compared to people without Down syndrome (Villani et al., Citation2020). This pattern of increased morbidity has also been examined in children with Down syndrome who contract COVID-19 (Emes et al., Citation2021; Leung et al., Citation2023; Malle, Bastard, et al., Citation2021). Depending on the study, mortality was considered low (Emes et al., Citation2021) or elevated compared to typically developing children (Leung et al., Citation2023). Thus, evidence regarding the magnitude of vulnerability of people with Down syndrome is inconsistent and needs further clarification. It should also be pointed out that the studies mentioned are not entirely comparable. Although they all compared patients with and without Down syndrome, they used different criteria for the comparison. In some studies, the samples were matched (by age and gender, sometimes by ethnicity) and sometimes other medical conditions were excluded from the control group. In other studies, the comparison group was the entire hospital population without Down syndrome (without additional exclusion criteria). In addition, a recent literature review on co-occurring medical conditions in adults with Down syndrome concludes that people with Down syndrome are a very complex and heterogeneous population and that different study designs and sample sizes make it difficult to derive generalised implications (Capone et al., Citation2020).
In the context of a pandemic, both national health protection policies and the quality and characteristics of the health care system must be considered (such as financial, spatial, and staff resources, knowledge, priorities, treatment approaches, and availability of prevention and treatment measures). Pinku et al. (Citation2022) compared the morbidity and mortality of people with Down syndrome in India compared to high-income countries, and found that the incidence of both hospitalisation and medical complications were higher in India than in high-income countries.
COVID-19 policies in Switzerland
We first provide basic information on Swiss health policy regarding COVID-19 as context for our study and its results. Switzerland uses a federal system, whereby the federal government and cantons share responsibility for population health. Shared responsibility also exists for pandemic management. However, an important distinction must be made between the “normal situation” and the “special situation”. In the normal situation, the federal government only assumes responsibility for monitoring, information, and coordination tasks, whereas concrete pandemic control measures are left to the 26 cantons, including the provision of population-level protection measures, treatment, testing, and vaccination. However, if the government declares a special situation (Art. 6 of the Epidemic Law, EpG SR 818.101), then it can order measures that must be implemented in all cantons.
At the outset of the COVID-19 pandemic, a national COVID-19 Task Force was established in Switzerland in March 2020, which supported the federal government by providing specialised expertise. In September 2020, the federal government created a COVID-19 Law and a COVID −19 Ordinance Special Situation (SR 818.101.26). Federal COVID-19 policy was guided by the principles of subsidiarity, effectiveness, and proportionality. Uniform federal regulations were established with respect to vaccination, testing, and recovery records. Categories of persons at particular risk were defined by the Federal Office of Public Health (2023). Persons aged 16 and over with Down syndrome were one of four specially designated risk groups, along with persons aged 65 and over, persons aged 16 and over with chronic diseases, and pregnant women. Designation as a special risk group had several implications relevant to our study, including prioritisation for vaccines. Vaccinations were strongly recommended but not mandatory for any population group. In addition, the federal government recommended and temporarily mandated special measures for social medical institutions (including institutions for persons with disabilities). These measures included, for example, visitation and contact restrictions, strict hygiene rules, and isolation measures in case of infection. The overarching goals of Switzerland’s COVID-19 policies were to protect the health of the population, avoid overwhelming the healthcare system, and simultaneously minimise the social and economic impact of the pandemic.
Objectives of the current study
The purpose of this study was to compare hospitalisation characteristics and disease progression between people with and without Down syndrome, using data from the Medical Statistics of Swiss Hospitals. Results will be discussed within the context of international literature. We examined the following research questions:
For patients diagnosed with COVID-19, does a median age difference exist between people with and without Down syndrome?
Do people with Down syndrome who are diagnosed with COVID-19 experience differences in hospital length of stay, compared to people without Down syndrome who are diagnosed with COVID-19?
Do people with Down syndrome who are diagnosed with COVID-19 experience disproportionately higher likelihood of ICU admission compared to people without Down syndrome who are diagnosed with COVID-19?
Do people with Down syndrome who are diagnosed with COVID-19 experience greater mortality than people without Down syndrome who are diagnosed with COVID-19?
Methods
Medical statistics of Swiss hospitals
Data from the Medical Statistics of Swiss Hospitals consist of mandatory reports documenting all treatment cases dating back to 1998. A treatment case is defined as an inpatient hospital stay from entry until exit. The statistics therefore always refer to a stay and not to a person. If a person is repeatedly admitted to hospital, a new entry is made. However, there is also an individual patient number to identify repeated admissions. Reported statistics include demographic data (e.g., age, sex, nationality) and information on hospital stay (e.g., type of admission, length of stay). All diagnoses are coded according to the International Statistical Classification Of Diseases And Related Health Problems, 10th revision, German Modification (ICD-10-GM; hereafter ICD-10). All treatments are coded according to the Swiss Operation Classification (Federal Statistical Office, Citation2021). We entered in a data usage agreement for three years of data (2020–2022) with the Swiss federal government, as represented by the Swiss Federal Statistical Office. Some data have been removed or further encrypted to protect data privacy (e.g., date of birth).
Data preparation and sampling procedure
The original data sets included more than 1.3 million cases of hospital admissions per year. We first identified the subset of people with Down syndrome by selecting for cases who had ICD-10 code Q90.- (Trisomy 21) as a main diagnosis or secondary diagnosis. The number of cases with Down syndrome was 706 in 2020 and 823 in 2021 (N = 1,529 in total). To compare the frequency of hospitalisations with COVID-19 infection between people with and without Down syndrome, an equally sized random sample of cases without Down syndrome was drawn from the overall data sets for each year.
In a second step, all cases with an ICD-10 code of U07.1! (COVID-19, virus detected) were extracted, which produced 36,166 cases in 2020 and 39,929 in 2021. Of these, 49 cases with Down syndrome were identified in 2020 and 73 in 2021 (N = 122 in total). To conduct comparisons within the population with confirmed COVID-19 infection, a random sample of cases without Down syndrome was drawn. There were no exclusion criteria for this random sample, except that a COVID-19 diagnosis had to be confirmed. Given the relatively small number of cases with Down syndrome in this subsample, a somewhat larger comparison group of cases without Down syndrome was selected. This procedure corresponds to best practice recommendations for methodological conduct in order to achieve adequate statistical power(Israel, Citation1992). The online calculator by Raosoft (Citation2004), which is based on the formula of Israel (Citation1992), recommended a subsample of 381 cases with COVID-19 infection and no Down syndrome for each year (N = 762 in total).
Furthermore, codes for pneumonia (J128), sepsis (A418), acute respiratory failure (J960), and respiratory distress syndrome (J80), which were required for further analyses on mortality, were selected from the reported diagnoses. In addition to ICD-10 codes, we used information about length of hospital stay, ICU admission, and whether a person was deceased. However, the dataset does not clearly delineate which diagnosis was the cause of death or ICU admission.
Data analyses
We first described the sample characteristics of people with and without Down syndrome according to age distribution, gender, and pre-admission residence. Second, we conducted preliminary analyses to compare the two samples regarding the incidence of COVID-19 diagnosis. To answer our research questions, we used inferential statistical procedures using the software SPSS 28 (IBM Corp, Citation2021). When comparing the two groups (Down syndrome, no Down syndrome), we used cross-tabulation with Chi-square test when there was a binary outcome (ICU admission or not) and the Mann–Whitney-U test when there was an ordered categorical outcome (age categories). When predicting length of hospital stay, we conducted a multiple regression analysis to control for whether a patient was deceased or not. Although more severe cases tend to have longer hospital stays, results could be biased by the presence of severe cases who die shortly after admission, thereby shortening their hospital stay. When predicting mortality, a binary outcome, we used a logistic regression approach to additionally control for age. Although several risk factors are thought to be associated with Down syndrome, patients with Down syndrome also tend to be younger, which might affect mortality. In addition, we provide further descriptive information regarding the main diagnosis of the deceased patients.
Results
Sample demographics
The following demographics refer to the total sample of cases with Down syndrome and the equally sized random sample of cases without Down syndrome, which were hospitalised between 1 January 2020 and 31 December 2021 (N = 3,058). Demographic data are determined by how they were recorded in the Medical Statistics of Swiss Hospitals. Age was recorded categorically using 20 levels (each covering five years). The lowest age category consisted of cases aged 0–4 years and the highest category 95 years and older. Gender was assessed using a binary variable (male, female). Since different regulations applied to private households and institutions in the context of COVID-19, data on residence before hospital admission are presented.
As can be seen in , the median age category of cases with Down syndrome who were hospitalised is lower (25-29 years) than that of cases without Down syndrome (60-64 years). Further, while males are slightly underrepresented in the non- Down syndrome sample (48.2%), they are overrepresented among cases with Down syndrome (58.3%). Regarding residence before hospital admission, patients with Down syndrome were more likely to live in institutions (rather than private homes) than persons without Down syndrome (16.0% vs. 2.8%). It is assumed that these institutions would typically be residential assisted living facilities for adults with intellectual disabilities. However, the specific type of institution is not evident from the data coding. All presented demographic differences were statistically significant (p < .001).
Table 1. Sample demographics (N = 3,058).
We first conducted preliminary analyses to compare the incidence of COVID-19 diagnosis in cases with Down syndrome compared to the same-size random sample of cases without Down syndrome. Results indicate that among the total sample of N = 3,058 cases, those with Down syndrome were significantly more likely to be diagnosed with COVID-19 (p < .001; see ).
Table 2. Cross-table of Down syndrome and COVID-19 diagnosis (N = 3,058).
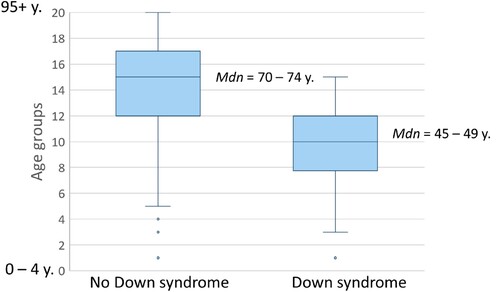
Analyses concerning the research questions are based on the subsample of cases with COVID-19 diagnosis (N Down syndrome: 122; N no Down syndrome: 762; N total: 884). Research question 1 refers to the difference in age between Down syndrome and non- Down syndrome cases. In line with the findings from the total sample, results indicate that also among persons diagnosed with COVID-19, those with Down syndrome are significantly younger (z (884): −11.58, p < .001). The median age of patients without Down syndrome was 70–74 years with a strong general tendency towards older age, while the median age of patients with Down syndrome was 45–49 years with a less strong tendency towards older age (see ). The difference between the two samples reveals a large effect size (d = 0.84), according to the interpretation of Cohen (Citation1988).
To answer research question 2, we examined whether Down syndrome and non- Down syndrome cases differed in their length of hospital stay, controlling for whether a person was deceased (which was assumed to potentially bias the results for length of stay). Mean length of stay was 9.30 days for Down syndrome cases (range: 1–44) and 11.57 (range: 1–141) for non- Down syndrome cases. Despite this descriptive difference, Down syndrome was not found to be a significant predictor of length of hospital stay (p = .051), and neither was mortality (p = .925; see ).
Table 3. Regression analysis to predict length of hospital stay by Down syndrome and mortality (N = 884).
Research question 3 focused on differences in ICU admission between Down syndrome and non- Down syndrome cases. As can be seen in , those with Down syndrome were admitted to the ICU more frequently than those without Down syndrome (p = .021). However, the effect size was small (V = .08).
Table 4. Cross-table of Down syndrome and ICU admission (N = 884).
In context of research question 4, we further investigated mortality rates in both groups. In the total sample of cases with Down syndrome (N = 122) and the respective random sample of cases without Down syndrome (N = 762), 18 (14.8%) persons with Down syndrome and 67 (8.8%) without Down syndrome were deceased. Given that age is a major risk factor for mortality in COVID-19, and given that patients with Down syndrome were on average observed to be younger than those without Down syndrome, we used a stepwise logistic regression approach to compare results with and without controlling for age. Results reveal that Down syndrome increases the risk of mortality by a factor of 1.8, which is significant at the 5% level (p = .040; see ). However, when age is included as a control variable, results indicate a more than seven times higher mortality risk for patients with Down syndrome, which is significant at the 1% level (p < .001). Hence, accounting for the fact that patients with Down syndrome are generally younger increases the effect of Down syndrome as a risk factor for mortality.
Table 5. Logistic regression analysis to predict mortality by Down syndrome and age (N = 884).
Although the Medical Statistics of Swiss Hospitals records diagnoses but not cause of death, we conducted descriptive analyses of which primary diagnoses occurred most frequently among deceased patients. In both groups, pneumonia was the most frequent primary diagnosis (Down syndrome: 72.2%; no Down syndrome: 62.7%). Other common principal diseases included sepsis, acute respiratory failure, and respiratory distress syndrome. All these diagnoses can be related to COVID-19 infection; however, this link is not directly evident in the data. Due to the small number of deceased people, especially in our subsample of cases with Down syndrome, further testing for group differences regarding primary diagnoses would have been inconclusive.
Discussion
Preliminary analyses revealed that among hospitalised persons in Switzerland, those with Down syndrome were overrepresented among cases with COVID-19 diagnosis, providing first insights into possible increased vulnerability. However, these results must be interpreted with caution, since there exist no precise statistics on the prevalence of Down syndrome in the overall Swiss population. Thus, it is impossible to determine whether the distribution of people with Down syndrome corresponds to the distribution of hospital admissions observed here. For example, it would be possible for people with Down syndrome (especially if they are professionally assisted in institutions) to be admitted to hospital more rapidly in the case of medical complications. Thus, they may be overrepresented in hospital admission data, potentially increasing the relative frequency of a COVID-19 diagnosis. The international literature is mixed, with studies that indicate an increased risk of infection for people with Down syndrome (e.g., Baksh et al., Citation2022) and those that found no difference from the general population (e.g., Illouz et al., Citation2021). Thus, it cannot be clearly determined whether people with Down syndrome are generally at higher risk for infection.
When only the sample with COVID-19 diagnosis was considered, we found that individuals with Down syndrome were significantly younger than those without Down syndrome. Two potential implications emerge. On the one hand, it suggests an increased vulnerability of people with Down syndrome to COVID-19, as they may be more susceptible to infection with COVID-19 at a younger age. On the other hand, since age is a major risk factor for severe disease progression, patients with Down syndrome might also benefit from their younger age. Regarding severe disease progression, a mixed picture emerged for patients with Down syndrome. In terms of length of hospital stay, there were no significant differences between the two groups, and therefore no evidence of greater vulnerability in people with Down syndrome. As already stated, it would be possible for people with Down syndrome to be admitted to the hospital more quickly in some cases, but to also leave the hospital soon because they are not seriously ill. A proportion of people with Down syndrome, on the other hand, might become critically ill, which in turn increases length of stay. Thus, the differences between the two samples would potentially be balanced again. Possible bias due to fatality cases that are hospitalised for only a short time was controlled for in the analyses.
Proportionally higher ICU admissions among patients with Down syndrome were observed, indicating increased vulnerability for severe disease progression, which is in line with previous studies (Boschiero, Lutti Filho, et al., Citation2022; Emami et al., Citation2021; Malle, Gao, et al., Citation2021). The same pattern was found regarding mortality rates: people with Down syndrome and COVID-19 diagnosis were proportionately more likely to die than people without Down syndrome who had a COVID-19 diagnosis. When controlling for the mean younger age of patients with Down syndrome compared to those without Down syndrome, the risk of mortality in Down syndrome was found to be more than seven times higher. These results align with the international state of research, where a two- to ten-fold increased risk was found (Boschiero, Lutti Filho, et al., Citation2022; Boschiero, Palamim, et al., Citation2022; Clift et al., Citation2021; Emami et al., Citation2021). It is important to keep in mind that the dataset provided no information about the exact cause of death. The additional diagnoses frequently mentioned in case fatalities, particularly pneumonia and respiratory problems, suggest a likely association with COVID-19. However, the data do not directly indicate whether COVID-19 was the cause of these indicators that point to greater disease severity (i.e., length of stay, ICU admission, and mortality).
Overall, there is some evidence of increased vulnerability regarding disease severity and mortality among people with Down syndrome. Yet, apart from the mortality risk, the effects were rather small and in some cases there were no differences at all, although a larger part of the international research points to a highly increased risk in Down syndrome (Baksh et al., Citation2022; Bensussen et al., Citation2022; Espinosa, Citation2020). Several potential explanations exist. First, results could indicate successful implementation of protective measures in Switzerland during the pandemic. Although Switzerland overall adopted less stringent COVID-19 policies than other countries (e.g., only a very short complete lockdown in spring 2020), much emphasis was placed on protecting vulnerable individuals in assisted living facilities (Federal Office of Public Health, Citation2021). Furthermore, people with Down syndrome (in addition to elderly people and people with pre-existing medical conditions) were listed as a special risk group in Switzerland at an early stage of the pandemic, and were thus given priority in the vaccination program. In contrast, there is no evidence of health care disadvantage or triage among people with Down syndrome based on data from the Medical Statistics of Swiss Hospitals. Nevertheless, a substantially increased mortality risk was evident in people with Down syndrome. Although this result should be interpreted with caution given the very low absolute number of fatalities in patients with Down syndrome, it may also suggest that an at-risk population is likely to remain at higher risk than the general population despite protective measures and adequate medical care. However, there is also evidence that the risk gap between the Down syndrome and non- Down syndrome population is larger in low-income than in high-income countries (Pinku et al., Citation2022).
Strengths, limitations, and future directions
A strength of the present study was the completeness of the data, which were based on national mandatory statistics collected from all Swiss hospitals. This allowed us to investigate the entire population of people with Down syndrome admitted to a hospital during a two-year span of the COVID-19 pandemic. Access to all coded diagnoses and various hospitalisation characteristics can be considered additional advantages of this study. However, several limitations with respect to the conclusions that can be drawn from these results must be noted. It was not possible to link data from the Medical Statistics of Swiss Hospitals with statistics on patient cause of death, thus it is unclear whether a person died with or from COVID-19. Studies that can provide more precise information about the cause of death or severe disease progression would help fill this research gap. Furthermore, the present results were based on a cross-section of all hospital admissions during two years of the pandemic. Longitudinal data that allow for analyses of the effects of restrictions and vaccination on hospitalisation and mortality over time could provide better insights into policies that would be most effective in future pandemics. In addition, there are indications that other disabilities may also be associated with an increased risk of severe disease progression in COVID-19. It would therefore be interesting to further investigate the vulnerability of people with other disabilities and compare them with people with Down syndrome. Finally, further comparisons between high- and low-income countries would increase understanding of the extent to which the quality of health care affects the relative risk of vulnerable populations, such as people with Down syndrome.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Altable, M., & de la Serna, J. M. (2021). Down’s syndrome and COVID-19: risk or protection factor against infection? A molecular and genetic approach. Neurological Sciences, 42, 407–413. https://doi.org/10.1007/s10072-020-04880-x
- Aparicio, P., Barba, R., Moldenhauer, F., Suárez, C., & Real de Asúa, D. (2023). What brings adults with Down syndrome to the hospital? A retrospective review of a Spanish cohort between 1997 and 2014. Journal of Applied Research in Intellectual Disabilities, 36(1), 143–152. https://doi.org/10.1111/jar.13043
- Bakaniene, I., Dominiak-Świgoń, M., Meneses da Silva Santos, M. A., Pantazatos, D., Grammatikou, M., Montanari, M., Virgili, I., Galeoto, G., Flocco, P., Bernabei, L., & Prasauskiene, A. (2023). Challenges of online learning for children with special educational needs and disabilities during the COVID-19 pandemic: A scoping review. Journal of Intellectual & Developmental Disability, 48(2), 105–116. https://doi.org/10.3109/13668250.2022.2096956
- Baksh, R. A., Strydom, A., Pape, S. E., Chan, L. F., & Gulliford, M. C. (2022). Susceptibility to COVID-19 diagnosis in people with Down syndrome compared to the general population: Matched-cohort study using primary care electronic records in the UK. Journal of General Internal Medicine, 37(8), 2009–2015. https://doi.org/10.1007/s11606-022-07420-9
- Bensussen, A., Valcarcel, A., Álvarez-Buylla, E. R., & Díaz, J. (2022). ORF8 and health complications of COVID-19 in Down syndrome patients. Frontiers in Genetics, 13, 1–4. https://doi.org/10.3389/fgene.2022.830426
- Boschiero, M. N., Lutti Filho, J. R., Ortega, M. M., & Marson, F. A. L. (2022a). High case fatality rate in individuals with Down syndrome and COVID-19 in Brazil: A two-year report. Journal of Clinical Pathology, 75(10), 717–720. https://doi.org/10.1136/jcp-2021-207802
- Boschiero, M. N., Palamim, C. V. C., Ortega, M. M., & Marson, F. A. L. (2022b). Clinical characteristics and comorbidities of COVID-19 in unvaccinated patients with Down syndrome: First year report in Brazil. Human Genetics, 141(12), 1887–1904. https://doi.org/10.1007/s00439-022-02468-3
- Capone, G., Stephens, M., Santoro, S., Chicoine, B., Bulova, P., Peterson, M., Jasien, J., & Smith, A. J. (2020). Co-occurring medical conditions in adults with Down syndrome: A systematic review toward the development of health care guidelines. American Journal of Medical Genetics Part A, 182(7), 1832–1845. https://doi.org/10.1002/ajmg.a.61604
- Capone, G. T., Chicoine, B., Bulova, P., Stephens, M., Hart, S., Crissman, B., Videlefsky, A., Myers, K., Roizen, N., Esbensen, A., Peterson, M., Santoro, S., Woodward, J., Martin, B., & Smith, D. (2018). Co-occurring medical conditions in adults with Down syndrome: A systematic review toward the development of health care guidelines. American Journal of Medical Genetics Part A, 176(1), 116–133. https://doi.org/10.1002/ajmg.a.38512
- Centers of Diseases and Control Prevention. (2022). Medical conditions. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
- Chicoine, B., Rivelli, A., Fitzpatrick, V., Chicoine, L., Jia, G., & Rzhetsky, A. (2021). Prevalence of common disease conditions in a large cohort of individuals with Down syndrome in the United States. Journal of Patient-Centered Research and Reviews, 8(2), 86–97. https://doi.org/10.17294/2330-0698.1824
- Clift, A. K., Coupland, C. A. C., Keogh, R. H., Hemingway, H., & Hippisley-Cox, J. (2021). COVID-19 mortality risk in Down syndrome: Results from a cohort study of 8 million adults. Annals of Internal Medicine, 174(4), 572–576. https://doi.org/10.7326/M20-4986
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Routledge.
- Courtenay, K., & Perera, B. (2020). COVID-19 and people with intellectual disability: Impacts of a pandemic. Irish journal of psychological medicine, 37, 231–236. https://doi.org/10.1017/ipm.2020.45
- De Toma, I., & Dierssen, M. (2021). Network analysis of Down syndrome and SARS-CoV-2 identifies risk and protective factors for COVID-19. Scientific Reports, 11, 1–12. https://doi.org/10.1038/s41598-021-81451-w
- Emami, A., Javanmardi, F., Akbari, A., & Asadi-Pooya, A. A. (2021). COVID-19 in patients with Down syndrome. Neurological Sciences, 42(5), 1649–1652. https://doi.org/10.1007/s10072-021-05091-8
- Emes, D., Hüls, A., Baumer, N., Dierssen, M., Puri, S., Russell, L., Sherman, S. L., Strydom, A., Bargagna, S., Brandão, A. C., Costa, A. C. S., Feany, P. T., Chicoine, B. A., Ghosh, S., Rebillat, A. S., Sgandurra, G., Valentini, D., Rohrer, T. R., Levin, J., & Lakhanpaul, M. (2021). Covid-19 in children with down syndrome: Data from the trisomy 21 research society survey. Journal of Clinical Medicine, 10(21), 1–19. https://doi.org/10.3390/jcm10215125
- Espinosa, J. M. (2020). Down syndrome and COVID-19: A perfect storm? Cell Reports Medicine, 1(2), 1–8. https://doi.org/10.1016/j.xcrm.2020.100019
- Evangelho, V. G. O., Bello, M. L., Castro, H. C., & Amorim, M. R. (2022). Down syndrome: The aggravation of COVID-19 may be partially justified by the expression of TMPRSS2. Neurological Sciences, 43(2), 789–790. https://doi.org/10.1007/s10072-021-05715-z
- Federal Office of Public Health. (2021a). COVID-19. https://www.bag.admin.ch/bag/en/home/krankheiten/krankheiten-im-ueberblick/coronavirus/covid-19.html.
- Federal Office of Public Health. (2021b). COVID-19: Informationen und Empfehlungen für sozialmedizinische Institutionen wie Alters- und Pflegeheime.
- Federal Statistical Office. (2021). Swiss classification of surgical interventions (CHOP): Systematic index - version 2021. https://www.bfs.admin.ch/news/en/2020-0124.
- Fujino, H., & Itai, M. (2023). Disinfection behavior for COVID-19 in individuals with Down syndrome and caregivers’ distress in Japan: A cross-sectional retrospective study. Journal of Developmental and Physical Disabilities, 35(1), 81–96. https://doi.org/10.1007/s10882-022-09845-w
- IBM Corp. (2021). IBM SPSS statistics for windows, Version 28.0.
- Illouz, T., Biragyn, A., Frenkel-Morgenstern, M., Weissberg, O., Gorohovski, A., Merzon, E., Green, I., Iulita, F., Flores-Aguilar, L., Dierssen, M., De Toma, I., Lifshitz, H., Antonarakis, S. E., Yu, E., Herault, Y., Potier, M.-C., Botté, A., Roper, R., Sredni, B., … Okun, E. (2021). Specific susceptibility to COVID-19 in adults with Down syndrome. NeuroMolecular Medicine, 23(4), 561–571. https://doi.org/10.1007/s12017-021-08651-5
- Israel, G. D. (1992). Determining sample size. In Program Evaluation and Organizational Development, 6, 1–5.
- Leung, C., Su, L., Simões-E-Silva, A. C., Arocha, L. S., de Paiva, K. M., & Haas, P. (2023). Risk for severe illness and death among pediatric patients with Down syndrome hospitalized for COVID-19, Brazil. Emerging Infectious Diseases, 29(1), 26–35. https://doi.org/10.3201/eid2901.220530
- Majithia, M., & Ribeiro, S. P. (2022). COVID-19 and Down syndrome: The spark in the fuel. Nature Reviews Immunology, 22(7), 404–405. https://doi.org/10.1038/s41577-022-00745-w
- Malle, L., Bastard, P., Martin-Nalda, A., Carpenter, T., Bush, D., Patel, R., Colobran, R., Soler-Palacin, P., Casanova, J. L., Gans, M., Rivière, J. G., & Bogunovic, D. (2021a). Atypical inflammatory syndrome triggered by SARS-CoV-2 in infants with Down syndrome. Journal of Clinical Immunology, 41(7), 1457–1462. https://doi.org/10.1007/s10875-021-01078-4
- Malle, L., Gao, C., Hur, C., Truong, H. Q., Bouvier, N. M., Percha, B., Kong, X. F., & Bogunovic, D. (2021b). Individuals with Down syndrome hospitalized with COVID-19 have more severe disease. Genetics in Medicine, 23(3), 576–580. https://doi.org/10.1038/s41436-020-01004-w
- Perera, B., Audi, S., Solomou, S., Courtenay, K., & Ramsay, H. (2020). Mental and physical health conditions in people with intellectual disabilities: Comparing local and national data. British Journal of Learning Disabilities, 48(1), 19–27. https://doi.org/10.1111/bld.12304
- Pinku, H., Hüls, A., Feany, P. T., Baumer, N., Dierssen, M., Bargagna, S., Costa, A. C. S., Chicoine, B. A., Rebillat, A. S., Sgandurra, G., Valentini, D., Rohrer, R. T., Levin, J., Lakhanpaul, M., Carfì, A., Sherman, S. L., Strydom, A., & Ghosh, S. (2022). Differences in clinical presentation, severity, and treatment of COVID-19 among individuals with Down syndrome from India and high-income countries: Data from the Trisomy 21 Research Society Survey. Journal of Global Health, 12, 1–11. https://doi.org/10.7189/jogh.12.05035
- Raosoft. (2004). Sample size calculator. http://www.raosoft.com/samplesize.html.
- Van Goor, J. C., & Massa, G. G. (1997). Increased incidence and prevalence of diabetes mellitus in Down's syndrome. Archives of Disease in Childhood, 77(2), 183. https://doi.org/10.1136/adc.77.2.183g
- Villani, E. R., Carfì, A., Di Paola, A., Palmieri, L., Donfrancesco, C., Lo Noce, C., Taruscio, D., Meli, P., Salerno, P., Kodra, Y., Pricci, F., Tamburo de Bella, M., Floridia, M., & Onder, G. (2020). Clinical characteristics of individuals with Down syndrome deceased with CoVID-19 in Italy — A case series. American Journal of Medical Genetics Part A, 182(12), 2964–2970. https://doi.org/10.1002/ajmg.a.61867