Abstract
Introduction. The effects of testosterone have been extensively characterized, but little attention has been given to the timetable of occurrence of the various effects of testosterone.
Methods. The timetables of effects on sexual and psychological variables in 40 hypogonadal men receiving treatment with either parenteral testosterone enanthate (TE) or undecanoate (TU).
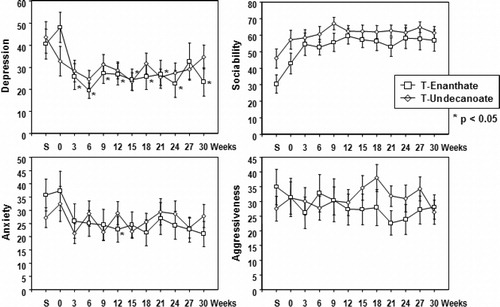
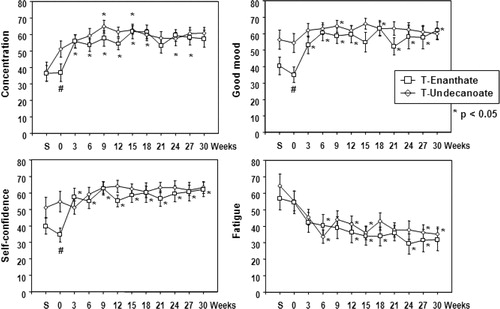
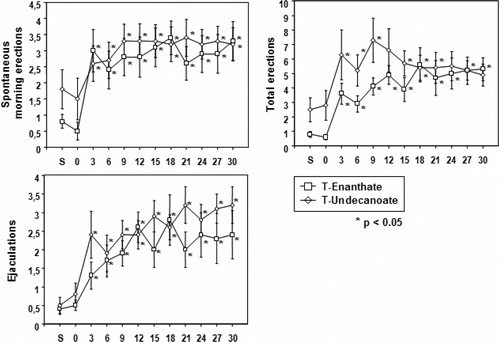
Results. Sexual thoughts/fantasies and sexual interest/desire/spontaneous morning erections emerged quickly and plateaued after 3 weeks. Total erections rose to a maximum over 9 weeks and then plateaued. Ejaculations per week/satisfaction with sex life rose over the first 3 weeks, increasing steadily to a plateau at 12 weeks. Depression scores decreased to reach a plateau after 6 weeks. Aggressiveness did not change. Scores of concentration improved and reached a plateau after 3 weeks in the group treated with TE and after 9 weeks in the group treated with TU. Good mood improved after 6–9 weeks. Positive effects on self-confidence appeared between 3–6 weeks and on fatigue after 9–12 weeks.
Conclusion. Insight into the emergence of effects may be useful information for the patient and for the attending physician in monitoring clinical effects of testosterone treatment of hypogonadal men.
Keywords:
Introduction
Treatment of hypogonadal men with testosterone is rewarding, for the patients as well as the physician. The patient experiences, to his satisfaction, profound changes in his physical appearance and his mental make-up. The attending physician observes the changes the patient undergoes and rarely fails to be fascinated by the multitude of functions testosterone appears to have in process of masculinization in the broadest sense.
Although the effects of testosterone have been described in detail, relatively little attention has been given to the timetable of the various effects of testosterone. This seems relevant. To the attending physician, monitoring the effects of administration of testosterone will be facilitated when it is known when certain effects can and should be expected. Patients like to receive information when the effects will set in. If patients have not been exposed to testosterone at the usual time of puberty, they must be counseled about the emergence of sexual thoughts and dreams, an increase in erections and seminal emissions.
In this study the effects of two treatment modalities of testosterone were analyzed: parenteral testosterone enanthate (TE) or long-acting parenteral testosterone undecanoate (TU). The latter is a rather novel testosterone preparation [Citation1,Citation2]. Over a period of 30 weeks, every 3 weeks the effects of testosterone administration on parameters of sexual functioning and mood were analyzed.
Subjects and methods
The study analyzed the relationship of time following administration vs. effects on sexual functioning and mood in an open-label, randomized, prospective clinical trial design [Citation3]. Subjects received either the traditional parenteral testosterone ester, TE or the new parenteral long acting testosterone undecanoate. Forty men were included in the study. Their ages ranged between 18 and 65 years and their serum testosterone levels at inclusion in the present study were <5 nmol/L (normal range, 10–30 nmol/L) following discontinuation of prior testosterone treatment for at least 8 weeks, and, if testosterone pellets had been used, for 12 months.
Seven patients had not received testosterone therapy previously. To ensure that the patients were meeting the inclusion criteria, they underwent two initial screening visits 42 and 21 days prior to randomization. If medical history, physical examination, and laboratory analysis at screening revealed evidence of severe physical or mental illness, of alcohol or drug abuse, or of any contraindication against testosterone treatment such as severe lower urinary tract symptoms, suspected malignancy of the prostate, erythrocytosis, heart/liver/kidney failure), patients were excluded from participation in the study. All patients gave their written informed consent to inclusion in the study. The study protocols were approved by the Ethics Committee of the University and the State Medical Board, Cologne, Germany.
The study medication (testosterone undecanoate (TU) (Nebido®) 1000 mg in 4 ml castor oil) and Testosteron-Depot JENAPHARM® Injektionslösung (TE 250 mg in 1 ml oily solution)) were manufactured by Jenapharm GmbH & Co. KG, Jena, Germany. All i.m. injections were administered into the gluteus medius muscle, starting on Day 0. The first four TU injections were given at two intervals of 6 weeks, the following after an interval of 9 weeks. All following injections were given at 12-week intervals [Citation18]. TE injections were administered at 3-week intervals. Every 3 weeks during the comparison study, patients presented for blood sampling and assessment of individual study variables.
The patients were randomly assigned (using the SAS software) to treatment with either TU i.m. (n = 20) or TE i.m. (n = 20) for 30 weeks. There were no essential differences between the two treatment groups regarding age, BMI, and baseline serum testosterone levels.
The study was financially supported by Jenapharm GmbH & Co KG, Jena, Germany.
For the assessment of possible psychosexual effects a standardized questionnaire published by Behre et al. [Citation4,Citation5] based on standardized questionnaires [Citation6,Citation7], was used, assessing general mood and sexual activity, as well as frequency of erections and ejaculations and number of morning waking erections, sexual thoughts and fantasies, sexual interest and desire, satisfaction with sexuality, as well as questions of general well-being during the past 7 days. In our experience compliance with tasks for the patients is best before a new visit to the clinic. Therefore, the data were collected for three consecutive days before each clinic visit over the 30 weeks of the study when the effects of TU were compared to those of TE. Patients were asked to rate their state concerning 12 different items (sociability, concentration, agitation, self-confidence, listlessness (inertness), dizziness, activation, depression, fatigue, anxiety, good mood, and aggressivity). The ratings were performed by the patients using a 10-cm visual analog scale, a horizontal line, on which a subject indicated his response checking tick-marks on a scale with two extremes designated ‘not at all’ and ‘very strong’. The subjects marked a point between these two extremes of ‘not at all’ and ‘very strong’ to specify their level of agreement to a statement. This method resembles a Likert-type scale, though in our scale, points were not fixed as in the Likert scales which commonly have a 5- or 7-point scale.
The ratings related to sexual fantasies, sexual interest, and satisfaction with sex life were recorded in the same way.
The answers were evaluated by measuring the distance between the beginning of the line segment (‘not at all’ and the mark made by the subject, multiplying this value by 100 and dividing by the length of the whole line segment.
Statistical analysis
For statistical analysis to examine the time-dependent effects of exposure a weight function within a generalized linear model was estimated. The shape of the weight function, which is modeled as a cubic B-spline, gives information about the impact of exposure increments at different times [Citation8].
Results
As reported earlier [Citation3] in the TE group, mean trough levels of serum T were always less than 10 nmol/l before the next injection, whereas in the TU group, mean trough levels of serum T were 14.1 ± 4.5 nmol/l after the first two doses (6-wk intervals) and 16.3 ± 5.7 nmol/l after the 9-wk interval at Week 30.
There were only a few minor statistically significant differences between the two treatment modalities with regard to their effects on the parameters of the study and their timetables; they were apparent in the non-sexual items of the effects of testosterone administration. Sexual thoughts/fantasies and sexual interest /desire rose quickly and plateaued 3 weeks after start of testosterone administration (P < 0.05) (). Spontaneous morning erections showed a similar pattern (P < 0.05). Total erections rose to a maximum over 9 weeks (P < 0.05) and then plateaued (). Ejaculations per week rose over the first 3 weeks (P < 0.05), and then increased steadily to a plateau reached after 12 weeks (P < 0.05 when compared with values at 3 weeks) (). Satisfaction with sex life showed a similar trend (P < 0.05) ().
Figure 1. Timetable of sexual thoughts/fantasy, sexual interest/desire and satisfaction with sex in hypogonadal men receiving treatment with testosterone enanthate (TE) or testosterone undecanaote (TU) over 30 weeks.
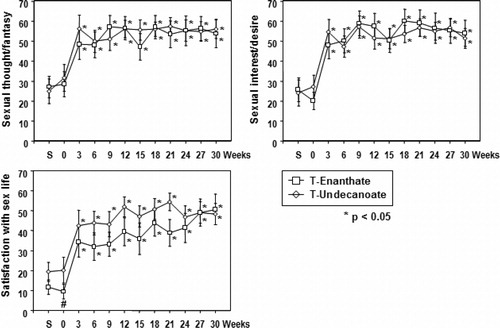
Figure 2. Timetable of spontaneous morning erections, total erections, and ejacualtions in hypogonadal men receiving treatment with testosterone enanthate (TE) or testosterone undecanaote (TU) over 30 weeks.
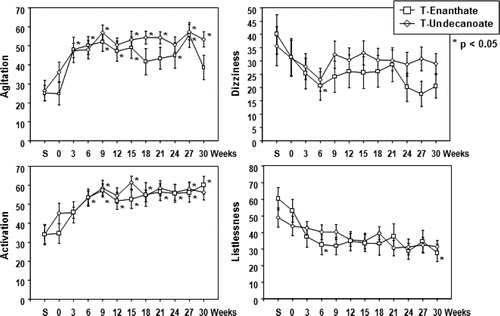
There was an improvement in scores of agitation starting 3–6 weeks after initiation of testosterone administration and plateauing after 9 weeks (). Dizziness improved slightly but reached statistical significance only in the population treated with TE (). Activation increased and plateaued after 6–9 weeks (). Listlessness (or inertness) improved slightly with statistical significance only in the population treated with TE (). Depression scores decreased (P < 0.05) to reach a plateau after 6 weeks (). Scores of sociability did not improve significantly (). Scores on anxiety improved slightly but reached statistical significance only in the group treated with TE (). Scores of aggressiveness did not change over the study period (). Scores of concentration improved and reached a plateau after 3 weeks in the group treated with TE and this was the case after 9 weeks in the group treated with TU (). There was a modest but significant increase in good mood after 6–9 weeks (P < 0.05) (). The positive effects on self-confidence appeared earlier and plateaued between 3 and 6 weeks (P < 0.05 (). Positive effects on fatigue were slower to plateau after 9–12 weeks (P < 0.05) ().
Figure 3. Timetable of psychological parameters (agitation, dizziness, activation, and listlessness) in hypogonadal men receiving treatment with testosterone enanthate (TE) or testosterone undecanaote (TU) over 30 weeks.
Discussion
This study of administration of parenteral TE and parenteral TU to hypogonadal men monitored when effects on sexual and mood parameters became manifest and reached a pleateau.
It appeared that effects on libidinous aspects of sexual behavior appeared rather rapidly, and reached a maximum already 3 weeks after start of testosterone administration. Effects on morning erections were equally rapid. Effects on total number of erections were slower in reaching a maximum after 9 weeks. There is some speculation that the neurophysiological mechanism of nocturnal erections is not identical with that of erections associated with sexual fantasies/activities [Citation9,Citation10]. This might be the case for morning erections which are, similarly, neither associated with sexual thoughts. Nocturnal erections are exquisitely dependent on androgens while other types of erections are less so [Citation10,Citation11]. There is further evidence that a state of hypogonadism has a deleterious effect on the anatomical structures involved in penile erection which is slowly restored by testosterone administration [Citation12,Citation13], maybe providing part of the explanation why effects of testosterone on other than nocturnal penile erections are somewhat slower to occur, though this is contradicted by the effects on morning erections which were quick to appear, but may be neurophysiologically of a different nature, though their final common pathway, erection of the penis is identical.
Testosterone exerts stimulatory effects on prostate secretory activity. In animal models this effect is restored within 1 week from androgen administration. Testosterone has also an effect on the neurovascular mechanism of ejaculation, related to restoration of nerve function. The latter may come about somewhat slow and explaining why ejaculatory activity reached a maximum only after 12 weeks. The sensation of ejaculation (expulsion of secretory products) might be a factor in sexual satisfaction explaining why this aspect ran a similar time course. The latter may have had an impact on seeking sexual sensations and thus have been a factor in the relatively slow increase in total number of erections. Upon testosterone treatment of erectile dysfunction the effects reach a maximum after 10–12 weeks which is consistent with our observation [Citation14–16].
Information on the timing of onset of behavioral effects after withdrawal of androgens is limited. With both naturally occurring and pharmacologically induced hypotestosteronemia, behavioral effects and a reduction in seminal emission become clear after 2 weeks and reach a maximum after 4 weeks or longer. A sexually active partner may be a factor in prolongation of sexual activity [Citation17]. In the majority of men, the ejaculatory capacity is profoundly decreased after androgen withdrawal, affecting sexual behavior in its own right [Citation17].
Restoration of testosterone effects is probably somewhat quicker, approximately over 1–2 weeks [Citation17]. We measured only at 3-week intervals and effects may have been present before the first assessment 3 weeks after starting testosterone administration. There may be a relationship with the duration of foregoing androgen deficiency [Citation17,Citation18]. In our study men had been withdrawn from any T treatment for at least 8 weeks before entering the study. Seven patients had not received testosterone therapy previously but the duration of their hypogonadal state is not known. The numbers were too limited to perform a subanalysis on these seven patients in relation to those men from whom testosterone had been withdrawn.
Timing of onset of administration of testosterone on parameters of mood have, to our knowledge, not been reported. In our study they appeared somewhat slower than on libidinous aspects of sexuality.
Subjects in our study were randomly assigned to treatment with TE or TU but the study was not blinded which was difficult because of the much higher frequency of administration of TE compared to TU. Though the pharmacokinetic profiles of TE (rapid increase/decrease of plasma testosterone levels with subnormal levels at the end of a 3-week injection interval) is very different from that of TU (a rather stable pattern of plasma testosterone within the physiological range), results of the two treatment modailites on the studied parameters were very similar. At times we found statistically significant differences between the two treatment modalities, with a more favorable outcome for TE, but these differences were quantitatively minor. It is further of note that, in spite of randomization, the initial psychometric scores were for some items more negative in the group treated with TE. So it is questionable whether these statistical differences represent biologically significant differences. The effects of testosterone administration on non-sexual variables may be related to the improvement of sexual variables. Improvement in mood may have been related to improvement in sexual functioning.
Similar to an earlier report on TU, we found no effects of either TE or TU on scores of aggressiveness [Citation19]. Such effects of testosterone have been reported in the literature but were found with much higher testosterone levels than achieved in our study or in men abusing sex steroids [Citation20]. Much of the confusion is semantic. In psychological jargon agression is a healthy attribute and lack of testosterone may be associated with lack of agression improving upon testosterone administration [Citation21].
A strong point in our study may have been that men included in the study had unambiguously hypogonadal plasma testosterone levels: <5 nmol/l (normal range, 10–30 nmol/l) and experienced a transition from a truly hypogonadal state to a state with circulating testosterone in a more normal range.
In summary: Upon administration of testosterone to hypogonadal men, libidinous aspects and morning erections were quick to appear reaching a maximum already after 3 weeks. Total number number of erections, ejaculations and satisfaction with sex life were slower and reached a maximum between 9 and 12 weeks. Psychological effects other than libidinous, reached, depending on the variable, their maximum between 3 and 12 weeks.
Declaration of interest: The authors declare no conflict of interest.
References
- Nieschlag E. Testosterone treatment comes of age: new options for hypogonadal men. Clin Endocrinol (Oxf) 2006;65:275–281.
- Saad F, Kamischke A, Yassin A, Zitzmann M, Schubert M, Jockenhel F, Behre HM, Gooren L, Nieschlag E. More than eight years' hands-on experience with the novel long-acting parenteral testosterone undecanoate. Asian J Androl 2007;9:291–297.
- Schubert M, Minnemann T, Hubler D, Rouskova D, Christoph A, Oettel M, Ernst M, Mellinger U, Krone W, Jockenhovel F. Intramuscular testosterone undecanoate: pharmacokinetic aspects of a novel testosterone formulation during long-term treatment of men with hypogonadism. J Clin Endocrinol Metab 2004;89:5429–5434.
- Behre HM, Abshagen K, Oettel M, Hubler D, Nieschlag E. Intramuscular injection of testosterone undecanoate for the treatment of male hypogonadism: phase I studies. Eur J Endocrinol 1999;140:414–419.
- Behre HM, Nashan D, Hubert W, Nieschlag E. Depot gonadotropin-releasing hormone agonist blunts the androgen-induced suppression of spermatogenesis in a clinical trial of male contraception. J Clin Endocrinol Metab 1992;74:84–90.
- Zerssen von D, Die Beschwerden-Liste. Weinheim, Germany: Beltz; 1976.
- Jahnke W, Debus G. Die Eigenschaftsworterliste EWL. Eine mehrdimensionale Methode zur Beschreibung von Aspekten des Befindens. Goettingen, Germany: Hogrefe; 1978.
- Hauptmann M, Wellmann J, Lubin JH, Rosenberg PS, Kreienbrock L. Analysis of exposure-time-response relationships using a spline weight function. Biometrics 2000;56:1105–1108.
- Bancroft J. Hormones and human sexual behavior. J Sex Marital Ther 1984;10:3–21.
- Bancroft J. The endocrinology of sexual arousal. J Endocrinol 2005;186:411–427.
- Bancroft J, Wu FC. Changes in erectile responsiveness during androgen replacement therapy. Arch Sex Behav 1983;12:59–66.
- Traish AM, Guay AT. Are androgens critical for penile erections in humans? Examining the clinical and preclinical evidence. J Sex Med 2006;3:382–404; discussion 404–407.
- Traish AM, Goldstein I, Kim NN. Testosterone and erectile function: from basic research to a new clinical paradigm for managing men with androgen insufficiency and erectile dysfunction. Eur Urol 2007;52:54–70.
- Greenstein A, Mabjeesh NJ, Sofer M, Kaver I, Matzkin H, Chen J. Does sildenafil combined with testosterone gel improve erectile dysfunction in hypogonadal men in whom testosterone supplement therapy alone failed? J Urol 2005;173:530–532.
- Yassin AA, Saad F. Treatment of sexual dysfunction of hypogonadal patients with long-acting testosterone undecanoate (Nebido). World J Urol 2006;24:639–644.
- Yassin AA, Saad F, Diede HE. Testosterone and erectile function in hypogonadal men unresponsive to tadalafil: results from an open-label uncontrolled study. Andrologia 2006;38:61–68.
- Bancroft J. Biological factors in human sexuality. J Sex Res 2002;39:15–21.
- Gooren LJ, Kruijver FP. Androgens and male behavior. Mol Cell Endocrinol 2002;198:31–40.
- O'Connor DB, Archer J, Wu FC. Effects of testosterone on mood, aggression, and sexual behavior in young men: a double-blind, placebo-controlled, cross-over study. J Clin Endocrinol Metab 2004;89:2837–2845.
- Pope HG, Jr, Kouri EM, Hudson JI. Effects of supraphysiologic doses of testosterone on mood and aggression in normal men: a randomized controlled trial. Arch Gen Psychiatry 2000;57:133–140; discussion 155–156.
- Zitzmann M. Effects of testosterone replacement and its pharmacogenetics on physical performance and metabolism. Asian J Androl 2008;10:364–372.