Abstract
Aim: To identify lifestyle factors associated with healthy aging in middle-aged and older Australian men.
Methods: A cross-sectional, population-based, computer-assisted telephone interview study explored self-reported health outcomes, and associated determinants for general and reproductive health (the Men in Australia Telephone Survey) in men aged 40 years and older (n = 5990). “Good health” was defined by self-reported health (excellent/very good) combined with absence of self-reported high blood pressure, heart disease, stroke, diabetes and depression symptoms. Categories of sexual activity frequency in the previous four weeks ranged from zero to 12+ times.
Results: “Good health” declined with increasing age with 17% of men over 70 years reporting “good health”. In multivariable logistic regression models, significant inverse associations were found between modifiable lifestyle factors – both underweight and overweight/obesity, physical inactivity, smoking and high alcohol consumption – and “good health”. Low-risk alcohol intake and living with a partner were positively associated with “good health”. Sexual activity was also positively associated with “good health” (p < 0.001) with elevated odds ratios (ORs) for each category of frequency of sexual activity (1–4, 5–8, 9–12 or 12+ times in the past 4 weeks) relative to zero frequency (ORs 1.68 to 2.16).
Conclusion: This study suggests that sexual activity is an important correlate of retaining good health in middle- and older-aged men, independent of other behavioral determinants.
Introduction
Nations with advanced or affluent economies increasingly recognize that the demographic shift in the age distribution to a progressively older population has significant health, social and economic impacts. In response, governments worldwide are implementing healthy aging services, policies and research agendas in attempts to address the functional decline associated with aging that leads to poorer health outcomes and increased disability, dependence and chronic disease [Citation1].
While many longitudinal studies aim to better understand the determinants of the decline in mental, social and physical function associated with aging, and provide robust evidence to inform healthy aging policy and best practice [Citation2,Citation3], there is little focus on the sexual health of older persons. The stereotypic image of older people as sexually inactive or lacking interest in sex still prevails [Citation4,Citation5], with government reports of the health of older Australians neglecting sexual activity as an important component of health and wellbeing [Citation1,Citation6]. However, studies have shown that despite declining sexual activity with age, many older people continue to be sexually active well into their 70s [Citation7,Citation8], and sexual activity is important to both men and women as they age [Citation7,Citation9]. Furthermore, strong associations have been demonstrated between healthy lifestyle behaviors (such as continuing physical activity) and sexual activity in later life [Citation10,Citation11]. Yet, little is understood about the predictors of healthy aging and particularly the contribution of sexual activity to an older person’s overall health and wellbeing.
Studies of gender differences in sexuality and aging report more sexual activity and interest in men than women and differing impacts of health status on sexual activity in men compared to women [Citation11–13]. We aimed to investigate the role of sexual activity in the context of other biomedical and behavioral factors associated with healthy aging in a representative sample of older Australian men. These data will contribute to health policy development, service provision, and community and professional education strategies targeted to the needs of the middle-aged and older male population.
Methods
The methods and initial findings from the Men in Australia Telephone Survey (MATeS) have been described previously [Citation14]. In summary, between September and December 2003, computer-assisted telephone interviews (CATI) of a representative sample of Australian men (aged 40 years and above) were undertaken. Respondents were recruited from across all states and territories by random selection of households from the electronic telephone directory (Electronic White Pages), with over-sampling in some age brackets and geographical regions to ensure proportional representation. A one-page invitation letter providing study details was sent to each household before telephone contact was made. Participation was voluntary and verbal consent was obtained before the start of the telephone interview. The study was approved by the Southern Health Human Research Ethics Committee, Melbourne, Australia.
Telephone survey instrument
The CATI included more than 90 questions focusing on socio-demographic, biomedical, and behavioral determinants, and knowledge and attitudes concerning male reproductive health and its disorders. The survey took an average of 17.5 min to complete. The full CATI is available at: www.andrologyaustralia.org/wp-content/uploads/MATeS_Methods_Manual_CATI.pdf
All information obtained from the interview was self-report with no check against medical records. Where available, questions from other validated instruments and those used in an Australian context were incorporated [Citation14].
“Good health” outcome variable
We defined “good health” using a combination of participant reported general health, using the single question (five possible responses) on perceived overall health status from the SF-12 [Citation15], including the responses “very good” and “excellent”, and the absence of major diagnosed chronic health conditions, that is, no reported high blood pressure, heart disease, stroke, diabetes or depression symptoms (defined by a positive response to the question “In the last 12 months, have you been depressed enough to interfere with daily living?”). The “good health” category included men who satisfied both criteria; those who did not satisfy both criteria were included in the “not good health” category.
Predictor variables
Body Mass Index (BMI) was classified as underweight (<20 kg/m2); normal (20.0–24.9 kg/m2); overweight (25.0–29.9 kg/m2); and obese (≥30 kg/m2). Waist circumference was classified as small (<94.0 cm); medium (94.0–101.9 cm); and large (≥102 cm). Cigarette (or other tobacco product) smoking, alcohol consumption and physical activity (assessed by recall of intensity, frequency and type in the last week) were classified according to the current Australian guidelines at the time of data collection [Citation16–18].
Sexual activity was defined as the reported frequency of orgasm or sexual climax in the previous four weeks, in categories ranging from zero to more than 12 times.
Statistical analysis
We stratified all analyses by age group, or adjusted for age, given the strong association between age and good health. Binary logistic regression was used to explore associations between “good health” as the dependent variable and each predictor variable, controlling for age in the first instance. Predictor variables included BMI categories, waist circumference categories, smoking status, alcohol intake, physical activity, vasectomy status, fatherhood status and frequency of sexual activity. Further logistic regression analyses were performed to assess adjusted associations of predictor variables with the “good health” outcome variable controlling for age as well as all other variables (fully-adjusted models). Only variables with p < 0.10 in age-adjusted models were included in the fully-adjusted models. Odds ratios (OR), 95% confidence intervals (95% CI) and p values are presented in the results.
This work was supported by the Australian Government Department of Health and Aging. The sponsor had no role in the design and conduct of the study, in the collection, analysis, interpretation of the data, or in the preparation, review or approval of the manuscript.
Results
From a total of 7636 randomly selected households with an eligible male, 5990 men (78%) agreed to participate in the study. Men were aged from 40 to 98 years (6% were above 80) with approximately equal numbers in four age strata: 40–49, 50–59, 60–69 and 70+.
The age-specific prevalence of “good health” was 46.4% (735/1585) in men aged 40–49, 39.6% (627/1584) in men aged 50–59, 28.3% (404/1428) in men aged 60–69 and 16.9% (235/1393) in men aged 70 or above.
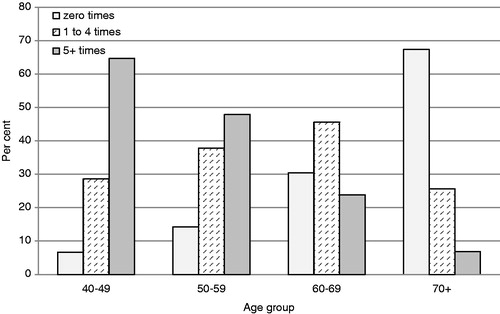
Frequency of sexual activity was inversely related to age () with 93% of 40–49-year-old men reporting sexual activity in the previous four weeks decreasing across age groups to 32% of men aged 70 years or older.
The distributions across age-groups of the variables potentially associated with good health (predictor variables) are presented in for groups defined according to the “good health” outcome. With the exception of BMI and physical activity measures, good health predictor variables tended to decrease in frequency across age-groups in both health outcome groups, and frequencies tended to be higher in the “good health” compared to the “not good health” group within each age-group.
Table 1. Health and behavioral determinants for men according to “good health” status and age-group.
To assess the strength of evidence for the associations of the predictors with the “good health” outcome, age-adjusted and fully-adjusted multivariable logistic regression models were done and results are reported in . “Good health” is inversely associated with increasing BMI, increasing waist circumference, smoking, and less than sufficient physical activity in multivariable models. Low-risk alcohol intake, living with a partner and all categories of sexual activity frequency (compared to no sexual activity) were positively associated with “good health” (odds ratios ranged from 1.68 to 2.16). Although having had a vasectomy was associated with “good health” in the age-adjusted models, it lost importance when adjusted for other predictors.
Table 2. Results from the multivariable logistic regression models (N = 4936).
Discussion
Our cross-sectional study of a nationally representative sample of middle-aged and older Australian men demonstrates that the frequency of sexual activity is positively associated with “good health”, independent of age and other known predictors of health in aging populations, and classified according to a robust outcome measure of the individual’s perceived level of health combined with absence of major chronic diseases. These data add to an emerging body of literature highlighting that sexual activity continues into older age [Citation7–9,Citation19], although the direct associations between sexual activity and other aspects of physical health and wellbeing are not so clearly articulated. Furthermore, to the best of our knowledge, this is the first report of a detailed frequency measure of sexual activity linked to “good health” in middle-aged and older men. An association between frequency of sexual activity and self-rated good health has been reported previously by Lindau and Gavrilova [Citation12], but our study has extended this finding to include a more stringent measure of good health with a more detailed frequency of sexual activity measure. Furthermore, rather than using sexual activity as an outcome in itself, as in several studies, we have assessed the role of sexual activity in “good health” in the context of other variables associated with health in older age, with sexual activity showing strong independent associations.
There are limitations to using self-reported data but computer-assisted telephone interviews are useful when exploring sensitive topics such as sexual activity and sexual health [Citation20]. Although self-reported data are subjected to possible information bias, the findings from this study are consistent with those from studies that have used face-to-face interviews and biomedical assessments to investigate general and reproductive health [Citation14].
This study confirms the associations between “good health” outcomes in middle-aged and older men and a range of conventional health and behavioral risk factors, such as smoking, alcohol intake, BMI, physical activity and depression symptoms, acknowledging that causality cannot be ascribed from observational studies. Similarly, despite the limitations of self-reported data, our “good health” measure, which includes both perceived health status and physical disease states, is consistent with findings using other health-related quality of life measures of the Australian population that demonstrate inverse associations with age and both high (overweight/obese) and low (underweight) BMI categories [Citation21]. Furthermore, the tendency towards decreasing odds ratios for “good health” with riskier behaviors highlights the robustness of the data despite the limitations of self-reported measures.
Our findings also highlight that sexual activity may be an indirect predictor of functional dependence and morbidity in community-dwelling middle-aged and older men. An American study supported this hypothesis where the main reason given for the lack of sexual activity by men and women who had a partner was the poor health of the man [Citation9]. Currently, definitions of healthy aging include a broad range of outcomes focusing on absence of major morbidity and disability, yet healthy aging also encompasses retaining a high level of functioning [Citation2] of which sexual health is an integral part. The lack of sexual health measures in healthy aging research primarily reflects “invisibility” and stereotyping of older people being sexually inactive [Citation22]. However, the associations between frequency of sexual activity and other health outcomes are consistent with the growing body of evidence that highlights the associations between erectile dysfunction and lifestyle determinants in a number of studies [Citation23–25] and previously confirmed in this cohort [Citation26]. With erectile dysfunction now considered an early-warning sign of more life-threatening disease due to the neuro-vascular physiological associations [Citation27], frequency of sexual activity, particularly in mid-life, may be an alternative measure of age-related decline of erectile function and potentially the extent of systemic vascular disease. The sensitivity of frequency measures of sexual activity may also provide subtleties that are not observed with blunt measures of erectile function. The inclusion of sexual activity frequency as an additional predictor in life-course epidemiological studies may further identify subsets of men who experience different functional status due to subtle vascular changes as they age and further enhance our understanding of the trajectories of healthy aging [Citation2].
Importantly, while advocating for sexual health measures to be included in the broader healthy aging research agenda, we need to carefully consider the concomitant evidence that overall sexual activity declines with age [Citation28]. Many older people may not have an opportunity for sexual activity (for example, with the loss of a partner) and the importance of sex may decrease with age. Consequently, while frequency of sexual activity may act as a potentially valuable but largely overlooked predictor of healthy aging, such measures may be a cause, consequence or independent but parallel association of progressive ill-health with age. Future research could assess the potential of other more comprehensive measures of sexuality that may better describe sexual experience of aging men [Citation29] and longitudinal studies to determine the direction of associations will inform policy and clinical practice.
Declaration of interest
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that: CAH and VRC are supported by the Australian Government Department of Health and Aging though its funding of Andrology Australia; CAH received support for a practice nurse men's health education workshop (2011) from Pfizer. The authors received no other support from any organization for the submitted work; have no financial relationships with any other organizations that might have an interest in the submitted work in the previous three years; and have no other relationships or activities that could appear to have influenced the submitted work.
The Andrology Australia project is supported by funding from the Australian Government under the Health System Capacity Development fund, and is administered by Monash University. We thank the Australian Department of Health and Aging for the financial support needed to undertake the study; the Hunter Valley Research Foundation, NSW for help with survey administration and data collection and the Centre for Clinical Effectiveness, Monash Institute of Health Services Research for assistance with identifying validated tools for the survey instrument.
Acknowledgements
We thank all the men who participated in this study.
References
- Australian Institute of Health and Welfare (AIHW). Older Australia at a glance. 4th ed. Canberra: AIHW; 2007
- Kivimäki M, Ferrie JE. Epidemiology of healthy aging and the idea of more refined outcome measures. Int J Epidemiol 2011;40:845–7
- Logie H, Hogan R, Peut A (Australian Institute of Health and Welfare). Longitudinal studies of aging: implications for future studies. Canberra: AIHW; 2004
- Andrews CN, Piterman L. Sex and the older man – GP perceptions and management. Aust Fam Physician 2007;36:867–9
- Gott M, Hinchliff S, Galena E. General practitioner attitudes to discussing sexual health issues with older people. Soc Sci Med 2004;58:2093–103
- Australian Institute of Health and Welfare (AIHW). Australia's health 2010. Canberra: AIHW; 2010
- Hyde Z, Flicker L, Hankey GJ, et al. Prevalence and predictors of sexual problems in men aged 75-95 years: a population-based study. J Sex Med 2012;9:442–53
- Holden CA, McLachlan RI, Cumming R, et al. Sexual activity, fertility and contraceptive use in middle-aged and older men: Men in Australia, Telephone Survey (MATeS). Hum Reprod 2005;20:3429–34
- Lindau ST, Schumm LP, Laumann EO, et al. A study of sexuality and health among older adults in the United States. N Engl J Med 2007;357:762–74
- Christensen BS, Gronbaek M, Osler M, et al. Associations between physical and mental health problems and sexual dysfunctions in sexually active Danes. J Sex Med 2011;8:1890–902
- Christensen BS, Gronbaek M, Pedersen BV, et al. Associations of unhealthy lifestyle factors with sexual inactivity and sexual dysfunctions in Denmark. J Sex Med 2011;8:1903–16
- Lindau ST, Gavrilova N. Sex, health, and years of sexually active life gained due to good health: evidence from two US population based cross sectional surveys of aging. BMJ 2010;340:c810
- Yee L. Aging and sexuality. Aust Fam Physician 2010;39:718–21
- Holden CA, McLachlan RI, Pitts M, et al. Men in Australia Telephone Survey (MATeS): a national survey of the reproductive health and concerns of middle-aged and older Australian men. Lancet 2005;366:218–24
- Ware Jr J, Kosinski M, Keller SD. A 12 Item Short Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220–33
- Australian Institute of Health and Welfare (AIHW). Indicators of health risk factors: the AIHW view. Canberra: AIHW; 2003
- National Health and Medical Research Council (NHMRC). Australian alcohol guidelines: health risks and benefits. Canberra: NHMRC; 2001
- Armstrong T, Bauman A, Davies JS (Australian Institute of Health and Welfare). Physical activity patterns of Australian adults. Results of the 1999 National Physical Activity Survey. Canberra: AIHW; 2000
- Beckman N, Waern M, Gustafson D, Skoog I. Secular trends in self reported sexual activity and satisfaction in Swedish 70 year olds: cross sectional survey of four populations, 1971–2001. BMJ 2008;337:a279
- Smith AM, Rissel CE, Richters J, et al. Sex in Australia: the rationale and methods of the Australian Study of Health and Relationships. Aust N Z J Public Health 2003;27:106–17
- Norman R, Church J, van den Berg B, Goodall S. Australian health-related quality of life population norms derived from the SF-6D. Aust N Z J Public Health 2013;37:17–23
- Kleinplatz PJ. Sexuality and older people. BMJ 2008;337:a239
- Chew K, Earle C, Stuckey B, et al. Erectile dysfunction in general medicine practice: prevalence and clinical correlates. Int J Impot Res 2000;12:41–5
- Kratzik CW, Schatzl G, Lunglmayr G, et al. The impact of age, body mass index and testosterone on erectile dysfunction. J Urol 2005;174:240–3
- Esposito K, Ciotola M, Giugliano F, et al. Effects of intensive lifestyle changes on erectile dysfunction in men. J Sex Med 2009;6:243–50
- Holden CA, McLachlan RI, Pitts M, et al. Determinants of male reproductive health disorders: the Men in Australia Telephone Survey (MATeS). BMC Public Health 2010;10:96
- Thompson IM, Tangen CM, Goodman PJ, et al. Erectile dysfunction and subsequent cardiovascular disease. JAMA 2005;294:2996–3002
- Laumann E, Gagnon J, Michael R, Michaels S. The social organization of sexuality: sexual practices in the United States. Chicago: University of Chicago Press; 1994
- Potts A, Grace VM, Vares T, Gavey N. ‘Sex for life'? Men's counter-stories on ‘erectile dysfunction', male sexuality and aging. Sociol Health Illness 2006;28:306–29