Abstract
Objectives: To study the effectiveness and safety of combined standard-dosed Solifenacin and Trospium for management of symptoms of overactive bladder (OAB) in elderly patients after the treatment with Tamsulosin.
Patients and methods: A total of 417 men over 50 years of age (average age 57.9 (8.3)) with diagnosed prostatic obstruction (score 8–19 according to I-PSS), who had not taken Tamsulosin before, were enrolled in the study. I-PSS questionnaire (from 8 to 19 – moderate) and Awareness Tool questionnaire for evaluating OAB symptoms (total score for OAB symptoms over 8) were used at the beginning and at the end of the observation. Also, urodynamic parameters were examined.
Result: Percentage of patients with prevalent symptoms of obstruction of urethra decreases after the treatment with Tamsulosin and then rises again (36.2%), but absolute number of patients remains smaller than initial data. Percentage of patients with relative prevalence of symptoms of overactive bladder slightly increases against administration of Tamsulosin and reaches initial values at the time of administration of anti-muscarinic drugs with absolute decrease in number of such patients.
Conclusion: Combination of Trospium and Solifenacin is an effective way to manage residual symptoms of hyperactive bladder during treatment of early obstruction of urinary bladder.
Introduction
Benign prostatic obstruction (BPO) is a pretty widespread abnormal state in men over 50 years old, and its frequency increases in association with ageing [Citation1–3]. Symptoms of BPO can be very troublesome for people over 50 years old and affect quality of their lives [Citation4]. Besides urethra obstruction affects urodynamics of lower urinary tract (LUT), and results in onset of symptoms of overactive bladder (OAB) [Citation5,Citation6]. BPO, as a rule, is treated with α1-blockers which are pretty effective and safe drugs managing the abnormal symptoms by enlarging prostatic part of the urethra. But they are not always effective for treating symptoms of ОАВ [Citation7]. If patients have strong concomitant symptoms of OAB, strategy of substitution of α1-blocker with anti-cholinergic agent, additional simultaneous prescription of anti-muscarinic drug and substitution of α1-blocker with other drug of the same group is used [Citation8,Citation9]. Sixth International Consultation On New Developments in Prostate Cancer and Prostate Diseases [Citation10] and some special studies [Citation11] adopted recommendations on combined administration of α1- blocker and anti-cholinergic drugs as a rational therapy for obstruction of urethra in prostatic gland area associated with symptoms of OAB. But according to available references, nowadays this problem still is of current interest because of big number of patients who report on disturbing symptoms of OAB after combined therapy. Analysis of main medical databases, such as PubMed, PubMed Central, Scopus, Synapse, CrossRef let us to conclude that effectiveness of different combinations of anti-muscarinics and α1-blockers in patients over 50 years old with steady symptoms of ОАВ is not sufficiently researched [Citation12,Citation13].
Tamsulosin HCL, which has high selectiveness for receptors of α1A subtype, is one of the most thoroughly studied and effective drugs, and because of its selective action on receptors of prostatic gland and weak action on receptors of aorta is pretty safe for patients over 50 years old [Citation14]. Previously, we studied use of combined action of anti-muscarinic drugs Solifenacin and Trospium on symptoms of OAB with different severity in patients over 50 years old and came to conclusion that combination of these drugs is very effective and does not increase the risk of developing side effects in patients over 50 years old [Citation15–17]. Based on this assumption in this article, we aimed at studying effectiveness and safety of combined standard-dosed Solifenacin and Trospium for management of symptoms of OAB, which remained in patients over 50 years old after the treatment with Tamsulosin.
Patients and methods
This double-blinded longitudinal randomized study was performed from January to December 2012 on the basis of Urological Department of Gerontological Hospital (Vladivostok city, Russian Federation). A total of 417 men over 50 years of age (average age 57.9 (8.3)) with diagnosed prostatic obstruction (score 8–19 according to I-PSS) and residual volume less than 100 ml, who had not taken Tamsulosin before, were enrolled in the study.
Working hypothesis
Considerable part of patients suffering BPO gets rid of specific symptoms of urethra damage after course of Tamsulosin, but retains symptoms of OAB. Probably, a short course of treatment with combination of Trospium and Solifenacin (acting mainly on different spectrum of bladder receptors) could be efficient means of OAB symptoms suppression for such patients.
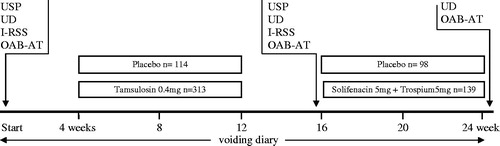
On the assumption of such idea, a protocol of examination, treatment and case follow-up () was worked out. At the beginning of the study, all possible participants of experiment were tested with the help of questionnaires IRSS and OAB Awareness Tool, each one underwent urodynamic examinations and ultrasound of the prostate. Then all patients whose BPO presence was confirmed were randomly divided into treatment and control groups. Within 2 months, treatment group of patients took Tamsulosin 0.4 mg/d, control group – placebo in identical coating. A month after the end of Tamsulosin course, all diagnostics procedures were repeated, it allowed detecting LUT function. On the basis of this study, a group of patients who did not reveal symptoms typical for BPO and OAB symptoms appeared to be apparent to different extent was formed. Such group comprised 139 persons (45.8% from initial group). All such persons were prescribed Solifenacin 5 mg + Trospium 5 mg which they were taking for 2 months. Group of persons taking placebo remained the same. During the whole study, patients were keeping urination diaries; upon the end of the course, state of LUT was examined with the help of urodynamic examination and OAB Awareness Tool. So, the first study endpoint was LUT function after the end of course of Tamsulosin, the second endpoint was the presence of OAB symptoms after protracted treatment by two anti-muscarinics.
Figure 1. Algorithm for the examination and treatment (n = 417). USP, ultrasound of the prostate; UD, urodynamics; I-RSS, international system of total symptom scores in prostate diseases; OAB-AT, OAB Awareness Tool – questionnaire to assess the symptoms of overactive bladder.
The first study endpoint is the study of presence and intensity of the whole spectrum of abnormal symptoms of LUT with the help of urodynamic examination, questionnaires I-RSS and OAB-AT and urination diaries a month after the end of course of Tamsulosin. On the basis of received data, a group of patients with absence of symptoms typical for BPO but with presence of symptoms of detrusor overactivity was formed. Other patients were excluded from study.
The second study endpoint is upon the end of 2-month course of Solifenacin and Trospium taking with the help of urodynamic examination, questionnaire OAB AT and urination diaries. Presence of detrusor overactivity symptoms was studied.
Design of the study is shown in . I-PSS questionnaire (from 8 to 19 – moderate) [Citation18] and Awareness Tool questionnaire for evaluating OAB symptoms (total score for OAB symptoms over 8) [Citation19–21] were used at the beginning and at the end of the observation. Also, such urodynamic parameters as postvoid residual urine volume (PVR), average and maximum flow rate (Qaver, Qmax) were examined at the beginning and at the end of the medication. To study dynamics of abnormal symptoms during all period of observation, patients were asked to fill in bladder diaries and record volume of urinations, information about urge episodes (UE), incontinence episodes (IE), episodes of night-time urination (ENU) [Citation22,Citation23]. Patients underwent ultrasound examination of prostatic gland before the study and after treatment with Tamsulosin [Citation24,Citation25].
In the first stage of study, all patients from treatment group (313 persons) were taking Tamsulosin 0.4 mg within 8 weeks [Citation26,Citation27]. Patients from control group (114 persons) were taking placebo. Then, after 1-month interval the LUT function was studied. Patients with presence of detrusor overactivity symptoms but with absence of BPO symptoms comprised treatment group for the second stage of observation. There were 139 persons. Each of them was every day treated with one dose of Solifenacin 5 mg and Trospium 5 mg per day within 4 weeks. Control group (98 persons) was taking placebo.
At the time of assignment to groups, patients with severe or complicated prostatic obstruction, infection of urinary tract, cancer, severe-associated chronic diseases of cardiovascular system or nervous system, kidney or liver failure were excluded from the study.
This study was carried out with the approval of the local ethics committee and with the full informed consent of patients.
Data were processed with program JMP SAS Statistical Discovery 8.0.2 (SAS Institute, Cary, NC). Wilcoxon test and Kruskal–Wallis rank test were used to compare data in the groups. Spearman’s correlation coefficient was applied to study dependence between processes. Standard deviation p values of <0.05 were considered statistically significant.
Results
I-PSS scoring for changes observed in patients after the treatment courses and results of examination of prostatic volume (in ml) are shown in . Frequency of feeling of incomplete emptying in patients after the treatment with Tamsulosin decreased insignificantly and after the treatment with Solifenacin and Trospium decreased significantly. Frequency of such symptom as intermittency, evaluated by score, also decreased a little bit, but insignificantly after both courses. Straining at urination disturbed fewer patients; changes were significant even after the first course of the treatment.
Table 1. Change in I-PSS and prostate volume at the start and after treatment (in scores).
Median of prostatic volume had no significant differences. The group of patients, who received placebo, did not demonstrate differences from initial data.
Results of study concerning frequency of symptoms of LUT disorder according to OAB-AT score and some urodynamic indices at the start of examination and after the treatment with Tamsulosin and combined anti-muscarinics are shown in . Number of complaints for frequent urinations during daytime after both treatments decreased insignificantly, but the same index during night time became significantly different from initial data after the treatment with Solifenacin and Trospium. Frequency of complaints for urgency significantly decreased only after the treatment with anti-muscarinics. The most significant dynamics was observed for such specific symptom as urgency incontinence – number of complaints after the treatment with anti-muscarinics decreased almost by three times. Residual volume remained the same after the treatment with Tamsulosin and significantly increased after the treatment with anti-muscarinic drugs. Average urine flow rate significantly increased only after the treatment with combined anti-muscarinics, although index of peak flow rate was higher than initial data already after the treatment with Tamsulosin. Changes in control group were not observed.
Table 2. Change in OAB-AT and urodynamic symptoms at the start and after treatment.
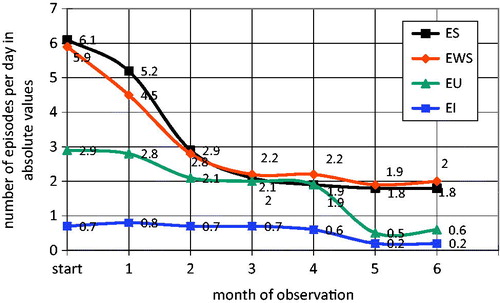
shows monthly changes in frequency of symptoms of OAB in absolute values against two treatment regimens. Frequency of episodes of weak stream tension, which was noted by patients in their bladder diaries, begins to decrease already at the first month of the treatment with Tamsulosin, at second and third month this decrease slows down and then frequency of these symptoms remains almost the same. Frequency of urge episodes and incontinence episodes, on the contrary, remains constant against the treatment with Tamsulosin and significantly decreased against treatment with anti-muscarinic drugs.
Figure 2. Changing some parameters of state off LUTs patients during treatment with tamsulosin and combination anti-muscarinic drugs. ES, episodes of straining; EWS, episodes of weak stream; EU, episodes of urgency, episodes of urgency incontinence (per day).
At the beginning of the second stage, patients with BPO symptoms in the group were absent. During the final study of LUT function upon the end of the course of anti-muscarinics treatment, it has been found out that 69 (49.6%) patients of 139 had no abnormal symptoms. Among other patients (70) 13 persons (9.3%) revealed detrusor overactivity symptoms, 25 (17.9%) revealed BPO symptoms, and 31 (22.3%) patients revealed mixed abnormal symptoms.
In other words, half of patients after a cycle of anti-muscarinics treatment had no any abnormal symptoms, overactivity symptoms was observed in small number of patients; however, abnormal symptoms returned to considerable number of patients (56 persons – 40.3%). Eleven patients from the main group (seven patients due to intolerably dry mouth, two patients due to dizziness, one patient due to high blood pressure, and one patient without any explanations of reasons) and 13 patients from control group (two patients due to headache, two patients due to high blood pressure, and nine due to absence of any effect) discontinued their participation in the clinical study.
Discussion
The problem of residual symptoms of OAB after effective treatment with α1-blockers is still not fully researched, despite of studies performed by different authoring teams. We made attempt to study influence of combination of standard-dosed Trospium and Solifenacin on residual symptoms of OAB and obstruction of urethra after the treatment with Tamsulosin.
Comparison of results of examination of patients with initial prostatic obstruction according to the I-PSS scale let us to conclude that comparatively fast improvement was observed in the symptoms specific for luminal narrowing of urethra. Frequency of symptoms of OAB, which was measured by I-PSS scale, significantly decreased only after the second course of the treatment (combined anti-muscarinics).
At the time of the study concerning frequency of specific symptoms of LUT disorder according to OAB-AT scale, we noted absence of significant dynamics after the treatment with Tamsulosin and appearance of improvements after the treatment with anti-muscarinics. Average urine flow rate increased substantially but not significantly after administration of α1-blocker, and after the treatment with anti-muscarinics values of this index were significantly different from initial data. Value of peak flow rate was significantly different already after the first administration of Tamsulosin.
Analysis of diaries of urinary incontinence, which were filled by patients during all the study, let us to observe trend in changes of symptoms under treatment with drugs of different groups. Frequency of specific symptoms of OAB almost does not change against administration of Tamsulosin and synchronously decrease under the treatment with combined anti-muscarinic drugs (r = 0.82, p ≤ 0.01). Frequency of symptoms of obstruction dramatically declined under administration of Tamsulosin (r = 0.75, p ≤ 0.05) and has almost no response to anti-muscarinics.
Study of dynamics of percentage of patients against performed treatment did not allow us to find out any common trend except monthly decrease of absolute number of patients with abnormal symptoms and some increase in percentage of patients with prevalent symptoms of obstruction at the end of the study.
Probably obtained affect can be explained by restoration of innervation of urethra and bladder, which was disordered due to prostatic hyperplasia, as a result of activation of specific receptors of detrusor. It is known that one of the courses for onset of symptoms of OAB together with weakening function of M2 and M3 receptors is an occurrence of so-called “afferent noise” due to dysfunction of peripheral vegetative nervous system. We cannot exclude that occurrence of such dysfunctions is caused by negative effect of prostatic hyperplasia on surrounding afferent fibers. In this case, influence of anti-muscarinic drugs compensates this dysfunction and provides good clinical effect. We suppose that this issue requires further study.
Conclusion
Symptoms of OAB are common complication associated with early obstruction of urinary bladder in patients over 50 years of age, and to reverse these symptoms anti-muscarinic drugs are necessary.
Combination of Trospium and Solifenacin is an effective way to manage residual symptoms of hyperactive bladder during treatment of early obstruction of urinary bladder.
Declaration of interest
The authors of this study have no conflict of interest.
References
- Vignozzi L, Rastrelli G, Corona G, et al. Benign prostatic hyperplasia: a new metabolic disease? J Endocrinol Invest 2014. [Epub ahead of print]
- Pöyhönen A, Auvinen A, Häkkinen JT, et al. Outcomes of medical and surgical treatment for lower urinary tract symptoms (benign prostatic obstruction) – a population-based cohort study. Int J Clin Pract 2014;68:349–55
- Kaplan SA. Re: intravesical prostatic protrusion can be a predicting factor for the treatment outcome in patients with lower urinary tract symptoms due to benign prostatic obstruction treated with tamsulosin. J Urol 2014;191:157–8
- Kahokehr A, Gilling PJ. Enucleation techniques for benign prostate obstruction: which one and why? Curr Opin Urol 2014;24:49–55
- Bozkurt IH, Yalcinkaya F, Sertcelik MN, et al. A good alternative to indwelling catheter owing to benign prostate hyperplasia in elderly: memotherm prostatic stent. Urology 2013;82:1004–7
- Spångberg A, Dahlgren H. Benign prostatic hyperplasia with bladder outflow obstruction. A systematic review. Lakartidningen 2013;110:682–5
- Liu N, Chen M, Chen S, et al. Preventive administration of antibiotics to patients with benign prostatic hyperplasia before urodynamic examination. Zhonghua Nan Ke Xue 2013;19:996–8
- Masumori N, Tsukamoto T, Horita H. α1-blocker tamsulosin as initial treatment for patients with benign prostatic hyperplasia: 5-year outcome analysis of a prospective multicenter study. Int J Urol 2013;20:421–8
- De Mey C. Alpha1-blocker therapy for lower urinary tract symptoms suggestive of benign prostatic obstruction: what are the relevant differences in randomised controlled trials? Eur Urol 2000;38:25–39
- Abrams P, Chapple C, Khoury S, et al. Evaluation and treatment of lower urinary tract symptoms in older men. J Urol 2009;181:1779–87
- Oelke M, Bachmann A, Descazeaud A. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 2013;64:118–40
- Kaplan SA, He W, Koltun WD, et al. Solifenacin plus tamsulosin combination treatment in men with lower urinary tract symptoms andbladder outlet obstruction: a randomized controlled trial. Eur Urol 2013;63:158–65
- Masumori N, Tsukamoto T, Yanase M. The add-on effect of solifenacin for patients with remaining overactive bladder after treatment with tamsulosin for lower urinary tract symptoms suggestive of benign prostatic obstruction. Adv Urol 2010;2010:205251
- Shalaby E, Ahmed AF, Maarouf A, et al. Randomized controlled trial to compare the safety and efficacy of tamsulosin, solifenacin, and combination of both in treatment of double-j stent-related lower urinary symptoms. Adv Urol 2013;2013:752382
- Kosilov K, Loparev S, Ivanovskaya MA, et al. Management of overactive bladder (OAB) in elderly men and women with combined, high-dosed antimuscarinics without increased side effects. UroToday Int J 2013;6:art 47
- Kosilov K, Loparev S, Ivanovskaya MA, et al. Elderly men with overactive bladder: maintenance of satisfactory therapeutic effect of administration of combined high-dosed antimuscarinics. UroToday Int J 2013;6:art 67
- Kosilov K, Loparev S, Ivanovskaya MA, et al. Maintenance of the therapeutic effect of two high-dosage antimuscarinics in the management of overactive bladder in elderly women. Int Neurourol J 2013;17:1–6
- Ruffion A, Marionneau N, Taïeb C, et al. Comparison of the response to I-PSS according to the mode of administration of the questionnaire: by the doctor or self-assessment by the patient. Prog Urol 2005;15:1080–4
- Coyne KS, Zyczynski T, Margolis MK, et al. Validation of an overactive bladder awareness tool for use in primary care settings. Adv Ther 2005;22:381–94
- Coyne KS, Margolis MK, Bavendam T, et al. Validation of a 3-item OAB awareness tool. Int J Clin Pract 2011;65:219–24
- Basra RK, Cortes E, Khullar V, et al. A comparison study of two lower urinary tract symptoms screening tools in clinical practice: the B-SAQ and OAB-V8 questionnaires. J Obstet Gynaecol 2012;32:666–71
- Thüroff JW, Abrams P, Andersson KE, et al. EAU guidelines on urinary incontinence. Eur Urol 2011;59:387–400
- Gurpreet S, Malcolm L, Lucia D, et al. Minimum standards for urodynamic practice in the UK. Neurol Urodyn 2010;29:1365–72
- Wooten WJ III, Nye JA, Schuster DM, et al. Accuracy evaluation of a 3D ultrasound-guided biopsy system. Proc SPIE 2013;8671
- Yang SL, Tang KQ, Bai WK, et al. Effects of low-frequency ultrasound combined with microbubbles on benign prostate hyperplasia. Can Urol Assoc J 2013;7:E681–6
- Milicevic S. Tamsulosin efficiency in treatment of benign prostatic hyperplasia evaluated by determining bladder weight. Med Arh 2012;66:391–5
- Eghbali K, Shayegan MR, Kianoush S. Investigating the effect of tamsulosin on the measurement of bladder wall thickness and International Prostate Symptom Score in benign prostatic hyperplasia. Can Urol Assoc J 2013;7:E317–21
