Abstract
Aim: The high prevalence of diseases and disabilities in the elderly will therefore impose major future challenges for governments, particularly in social security, health system and social care.
Methods: Nine hundred and seventy-one men, 40 years or older referred for low urinary tract symptoms (LUTS) evaluation who underwent full urodynamic investigation, were reviewed. Urodynamic parameters were obtained, such as Uroflowmetry, those of Filling Cystometry and those of pressure flow study (PFS).
Results: Mean age was of 66.1 years old. Most the patients included in the analysis were categorized as Schafer score 2–4. Correlation analysis of uroflowmetry parameters revealed statistically significant decrease in voided volume (p = 0.013), Qmax (p = 0.023) with aging. Cystometric parameters revealed significant age-related decrease in bladder capacity (p < 0.001) and bladder compliance (p = 0.004). PFS revealed significant decrease in voiding efficiency (p = 0.029), voided volume (p < 0.001), Qave (p = 0.008) and Qmax (p = 0.048) with progressing age. Age subgroup analyses showed significant differences in voiding efficiency (KW, p = 0.032), voided volume (KW, p < 0.001) and Qave (KW, p = 0.036).
Conclusions: Age-related changes in voiding function might not be a result of impaired detrusor contractility or increased outflow obstruction, intrinsic causes must be suspected. Changes in the storage function of the bladder represent specific pathophysiological mechanisms influenced by aging.
Introduction
Over the past two centuries life expectancy has increased linearly [Citation1]. The high prevalence of diseases and disabilities in the elderly will therefore impose major future challenges for governments, particularly in social security, health system and social care [Citation1]. Among those conditions, voiding dysfunction is an independent predictor of health status deterioration as well as poorer health-related quality of life [Citation2]. Furthermore, it bears socioeconomic impact due to its high prevalence [Citation3] and associated conditions, such as increased risk of falls [Citation4], depression [Citation5] and deterioration of sleep patterns [Citation6] and instrumental daily living activities [Citation2].
The prevalence and severity of low urinary tract symptoms (LUTS) increase significantly with age, as well as the dissatisfaction with them [Citation2,Citation3]. It has been estimated that 15–60% of men older than 40 years have LUTS and up to 70% of men older than 80 years may be affected [Citation2,Citation3,Citation7,Citation8]. In the European and Korean UrEpik Study, the prevalence of male moderate to severe symptoms increased 10% per decade from 40 to 79 years of age [Citation7].
Voiding dysfunction of the elderly is almost always a multifactorial condition, strongly influenced by comorbidities, concurrent medication and physiological particularities of this population [Citation9]. Bladder outlet obstruction (BOO) due to benign prostate enlargment (BPE) is a major cause of male LUTS [Citation6]. Aproximately half of all men with BPE experience moderate to severe LUTS [Citation6]. In addition to obstruction, the process of aging itself can also evoke alterations in the structure, innervation and function of the bladder. These changes can lead to LUTS, but it is difficult to separate the effects of obstruction from those of aging [Citation10].
Most studies on bladder function of men with LUTS agree that urinary flow, bladder capacity and compliance decrease with advancing age, and it is also generally accepted that there is an age-related increase in the incidence of overactive bladder [Citation10]. The well-established age-related reduction on urinary flow could be influenced by an increase in the degree of obstruction or impairment of detrusor contractility. However, most series have demonstrated that the degree of obstruction is not affected by aging [Citation11–14]. On the other hand, regarding detrusor contractility, the issue still is controversial.
Previous authors have studied the impact of age on bladder function. Even though some age-related urodynamic changes are unanimously described, others, such as detrusor contractility, are still a matter of debate. Additionally, most of those studies evaluated men with LUTS regardless of the degree of outflow obstruction. Therefore, the aim of our investigation was to evaluate age-related changes in bladder function of untreated men with urodynamically proven BOO.
Materials and methods
This project has the approval of the Ethics Committee of Federal University of São Paulo, Brazil.
Data from 971 men, 40 years or older referred for LUTS evaluation who underwent full urodynamic investigation during a period of four years, were reviewed. Only men who were able to void at least 100 mL during the pressure flow study (PFS) were eligible. Exclusion criteria were urinary retention, urinary tract infection, previous surgery of the LUT (prostate, bladder and urethra), abnormal neurologic status, neurogenic bladder dysfunction, diagnosed prostate cancer and use of medication with major effect on voiding function (alpha-receptor blockers, 5 alpha-reductase inhibitors and anticholinergic agents). Patients with no urodynamic obstruction, as defined by a linear passive urethral resistance relation (Schäfer obstruction score) less than 2, were also excluded. A total of 255 men with urodynamically proven BOO were included in the study after fulfilling these criteria.
Urodynamic procedures were performed on an outpatient basis in the urodynamic clinic of Federal University of Sao Paulo following the International Continence Society (ICS) guidelines of “Good Urodynamic Practices” [Citation15]. Machine calibration, reference levels, quality control and trace interpretation conformed to the recommendations of the ICS [Citation15–19]. All the original traces were available for manual reading and artifacts were immediately excluded. Urinary sediment and microbiological analysis were negative at investigation and patients had no signs or symptoms of urinary tract infection at the occasion of the urodynamic evaluation.
Study design and statistical analyses
The correlations between age and urodynamic parameters were calculated by the Spearman’s rank correlation test. The coefficient of correlation (r) was graded as very weak (0–0.19), weak (0.2–0.39), moderate (0.4–0.69), strong (0.7–0.89) and very strong (0.9–1.0) correlations.
To obtain a more detailed insight into the age-related changes, a sub-analysis was performed with the urodynamic parameters that reached statistically significant correlation with age. Patients were grouped according to decades of life. Age subgroup analyses were performed by nonparametric tests, since the assumption of normal distribution was rejected. For quantitative variables subgroup analyses were assessed by the Kruskal–Wallis (KW) test with multiple paired comparisons by the Dunn's test. For qualitative variables the Chi-Square (χ2) test was performed to evaluate the homogeneity of age subgroups and for linear trend analyses.
Comparisons between means were performed by Student’s t-test.
Two-tailed statistical significance was defined as p < 0.05.
Results
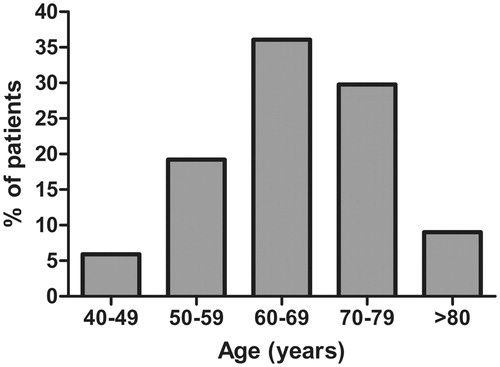
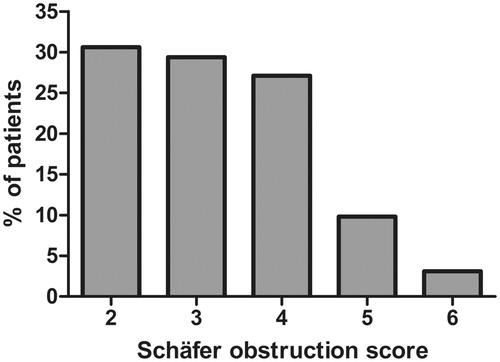
Age was almost normally distributed with a peak in the seventh decade of life and mean of 66.1 ± 9.9 years. The age range covered five decades of life, from 41 to 87 years (). The majority of the patients included in this analysis were categorized as Schafer obstruction score 2–4 ().
Noninvasive uroflowmetry
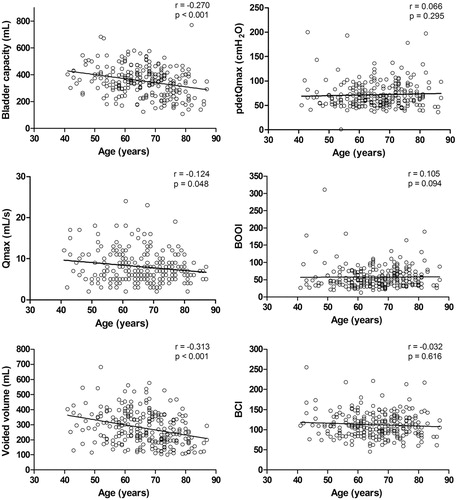
Correlation analysis of uroflowmetry parameters revealed statistically significant decrease in voided volume (p = 0.013) and Qmax (p = 0.023) with progressing age. In contrast, no significant age-related correlations with Qave, flow time, time to Qmax and post-void residual (PVR) volume were found (). Subgroup analyses based on decades of life showed no statistically significant differences among age groups in any of the parameters evaluated ().
Table 1. Principal patient characteristics and correlation between age and urodynamic parameters.
Table 2. Age subgroup analyses of urodynamic parameters.
Filling cystometry
Correlation analysis of cystometric parameters revealed significant age-related decrease in bladder capacity (p < 0.001) and bladder compliance (p = 0.004) (, ). Regarding bladder capacity, the age subgroup analyses showed significant differences (KW, p < 0.001). Beyond 70 years old, the bladder capacity was significantly lower than that in men 40–49 and 60–69 years old (Dunn, p < 0.05) (). In parallel, bladder compliance was constantly lower over decades of life with a trend towards significance (KW, p = 0.053). Reduced bladder compliance (<10 mL/cm H2O) was seen in 15.3% of patients. As expected, the occurrence of reduced bladder compliance was progressively higher throughout age subgroups with statistical significance (χ2trend, p = 0.006) ().
Figure 3. Correlation between age and urodynamic parameters. Line fitted by simple linear regression analysis is shown along with correlation coefficient (r value) calculated by Spearman’s rank correlation test (p value). Qmax = maximum flow rate; PdetQmax = detrusor pressure at maximum flow; BOOI = bladder outlet obstruction index; BCI = bladder contractility index.
Detrusor overactiviy (DO) was seen in 63.1% of patients and its occurrence was constantly higher over decades of life with statistical significance (χ2trend, p = 0.0012) (). Patients with DO were significantly older than those with stable bladder with mean ages of 67 ± 9 years and 64 ± 10 years, respectively (Student's t-test, p = 0.008). No significant age-related correlations with DO pressure or the volume of DO occurrence were found ().
DO incontinence was seen in 23.1% of patients and its occurrence was progressively higher throughout age subgroups with statistical significance (χ2trend, p < 0.001) (). No significant age-related correlation with detrusor leak point pressure (DLPP) was demonstrated ().
Pressure flow study
Correlation analysis of PFS revealed significant decrease in voiding efficiency (p = 0.029), voided volume (p < 0.001), Qave (p = 0.008) and Qmax (p = 0.048) with progressing age (, ). Age subgroup analyses showed significant differences in voiding efficiency (KW, p = 0.032), voided volume (KW, p < 0.001) and Qave (KW, p = 0.036). Voiding efficiency of patients 80 years or older was significantly lower than for those younger (Dunn, p < 0.05). Beyond 80 years old, voided volume and Qave were significantly lower compared to those in men younger than 70 years (Dunn, p < 0.05). In parallel, Qmax was constantly lower over decades of life, yet statistically insignificant (KW, p = 0.071) ().
In contrast, no significant age-related correlations with flow time, time to Qmax, PVR volume, detrusor pressure at maximum flow (PdetQmax), maximum detrusor pressure (PdetMax), Schäfer obstruction score, bladder outlet obstruction index (BOOI) and bladder contractility index (BCI) were noted (, ).
Discussion
The impact of age on bladder function has already been studied by previous series, but most of them evaluated men with LUTS regardless of the degree of obstruction. Additionally, even though some age-related urodynamic changes are unanimously described, others, such as detrusor contractility, are still a matter of debate. Therefore, we aimed to evaluate age-related changes in bladder function of untreated men with urodynamically proven BOO, besides providing further evidence to controversial issues.
Changes in the structure, metabolism and innervation of the bladder may occur with BOO and aging itself. These changes lead to voiding dysfunction, but it is difficult to distinguish the effects of BOO from those of aging, since both can trigger similar pathological processes and outcomes [Citation10]. Recent studies have demonstrated that storage LUTS increase with age in both men and women, with little correlation with underlying disease processes, such as benign prostate enlargement, suggesting it may be at least partly regarded to the aging process itself [Citation20].
Previous authors have shown reduction in bladder capacity and compliance with progressing age [Citation11,Citation21–23]. Accordingly, we observed significant age-related decrease in both parameters, and the occurrence of reduced bladder compliance was also progressively higher throughout age subgroups. Animal studies have demonstrated that atherosclerosis-induced chronic ischemia leads to detrusor fibrosis, which decreases bladder compliance [Citation20]. Less compliant bladder tends to activate tension receptors earlier, leading to decreased functional bladder capacity [Citation10,Citation20,Citation24].
DO is found at urodynamic investigation in about 25–75% of patients with LUTS and it is generally accepted that its incidence increases with age [Citation10–14,Citation21–23,Citation25,Citation26]. Similarly, in our study, DO was seen in 63.1% of patients and its occurrence was constantly higher over decades of life. DO incontinence, seen in 23.1% of the patients, also showed a progressively higher occurrence throughout age subgroups; what might be explained by the higher age-related DO occurrence previously described, since neither DO pressure increased nor DLPP decreased with age. The underlying pathological mechanisms leading to this phenomenon still require additional enlightenment. Elbadawi et al. [Citation24] conducted a comprehensive study regarding ultrastructural changes related to geriatric voiding dysfunction. The author demonstrated partial detrusor denervation related to normal aging, what was also observed in overactive bladders, leading to increased activation of LUT afferent pathways [Citation10,Citation20,Citation24]. Atropine resistance and additional purinergic activation in the unstable aged bladder may also contribute to the changes in bladder function in the elderly [Citation20]. Furthermore, pelvic ischemia may play a role in this process, by inducing damage to the urothelium with possible chronic exposure of the underlying tissue and nerves to the urine. The suburothelial space, containing afferent nerve fibers and interstitial cells, presents a variety of neurotransmitter interactions, which are essential for bladder sensation. Imbalances within this suburothelial complex have been indicated as significant contributors to storage LUTS, along with abnormalities of central function [Citation20].
In accordance with other studies, reduction of urinary flow rate and voided volume with advancing age was also demonstrated in our study by both uroflowmetry and PFS, as well as an age-related decrease in voiding efficiency [Citation11,Citation14,Citation21,Citation27]. However, these changes were probably not resultant of increased outflow obstruction or impaired detrusor contractility, since, in our series, these parameters seemed not to be influenced by age. This lack of correlation between age and degree of obstruction assessed by either the Schäfer obstruction score or the BOOI finds support in previous studies [Citation11–14].
On the other hand, the influence of age on detrusor contractility is still controversial. A review about aging bladder concluded that detrusor contractility does decrease with age [Citation10]. According to the author, this might be due to myogenic or neurogenic changes, which might be related to pelvic ischemia [Citation10]. A cohort of untreated obstructed men also demonstrated a small but significant reduction in detrusor contractility in a 10-year follow-up [Citation14]. In contrast, others failed to demonstrate age-related changes in detrusor function or contractility parameters [Citation11,Citation12,Citation21,Citation27,Citation28]. According to Al-Hayek et al. [Citation28], there is no evidence that detrusor contractility declines with long-term BOO and surgical relief does not improve bladder contractility. The authors state that underactive detrusor tends to remain underactive, but does not worsen with time, what indicates that it may have a congenital basis instead of resulting from aging itself [Citation28]. Our findings are consistent with the last ones, since no significant correlations were found between age and PdetQmax, PdetMax or BCI, in the present study.
Degenerative changes in detrusor muscle and intrinsic nerves have been associated with detrusor contractility impairment [Citation24], but Brierly et al. [Citation29] showed no correlation between age and the amount of these degenerated cells. Moreover, an in vitro study about contractile properties of human detrusor smooth muscle concluded that neither there is no evidence for a decline of contractility or excitability as a function of age, nor any gender or pathology [Citation30].
The relative contributions of motor, sensory and biomechanical dysfunctions to impaired voiding performance associated with aging still need future insights. Well-controlled prospective studies in older subjects involving urodynamic, ultrastructural and biochemical assessment are essential for better characterization of the effects of aging on bladder function.
The retrospective nature of the current study leads to a number of potential shortcomings, in particular being prone to selection biases. Despite having been set strict inclusion and exclusion criteria in order to minimize those, the study design does not permit to control this condition. Therefore, we must emphasize, as in all such studies, that extrapolation of data to the community should be performed with caution.
In concludion, changes in bladder capacity, compliance, DO and DO incontinence were more prominent with aging and might represent specific pathophysiological mechanisms, such as increased activation of LUT afferent pathways. Age negatively influenced voided volume, urinary flow rate and voiding efficiency; however, these changes were probably not a result of impaired detrusor contractility or increased outflow obstruction as it would be expected, since these parameters were not related to age.
Conclusions
Advancing age is not necessarily associated with worsening of the degree of obstruction or deterioration of detrusor contractility in men with untreated BOO. Therefore, age-related changes in voiding function might not be a result of impaired detrusor contractility or increased outflow obstruction, and intrinsic causes must be suspected. On the other hand, changes in the storage function of the bladder might represent specific pathophysiological mechanisms influenced at least in part by aging.
Declaration of interest
The authors report no conflicts of interest.
References
- Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet 2009;374:1196–208
- Taylor BC, Wilt TJ, Fink HA, et al. Prevalence, severity, and health correlates of lower urinary tract symptoms among older men: the MrOS study. Urology 2006;68:804–9
- Parsons JK, Wilt TJ, Wang PY, et al. Progression of lower urinary tract symptoms in older men: a community based study. J Urol 2010;183:1915–20
- Parsons JK, Mougey J, Lambert L, et al. Lower urinary tract symptoms increase the risk of falls in older men. BJU Int 2009;104:63–8
- Engstrom G, Henningsohn L, Steineck G, Leppert J. Self-assessed health, sadness and happiness in relation to the total burden of symptoms from the lower urinary tract. BJU Int 2005;95:810–15
- Committee AUAPG. Aua guideline on management of benign prostatic hyperplasia (2003). Chapter 1: diagnosis and treatment recommendations. J Urol 2003;170:530–47
- Boyle P, Robertson C, Mazzetta C, et al. The prevalence of lower urinary tract symptoms in men and women in four centres. The UrEpik study. BJU Int 2003;92:409–14
- Parsons JK, Bergstrom J, Silberstein J, Barrett-Connor E. Prevalence and characteristics of lower urinary tract symptoms in men aged >=80 years. Urology 2008;72:318–21
- DuBeau CE. The aging lower urinary tract. J Urol 2006;175:S11–15
- Nordling J. The aging bladder – a significant but underestimated role in the development of lower urinary tract symptoms. Exp Gerontol 2002;37:991–9
- Madersbacher S, Klingler HC, Schatzl G, et al. Age related urodynamic changes in patients with benign prostatic hyperplasia. J Urol 1996;156:1662–7
- Eckhardt MD, van Venrooij G, Boon TA. Interactions between prostate volume, filling cystometric estimated parameters, and data from, pressure-flow studies in 565 men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Neurourol Urodyn 2001;20:579–90
- Vesely S, Knutson T, Fall M, et al. Clinical diagnosis of bladder outlet obstruction in men with lower urinary tract symptoms: reliability of commonly measured parameters and the role of idiopathic detrusor overactivity. Neurourol Urodyn 2003;22:301–5
- Thomas AW, Cannon A, Bartlett E, et al. The natural history of lower urinary tract dysfunction in men: minimum 10-year urodynamic follow-up of untreated bladder outlet obstruction. BJU Int 2005;96:1301–6
- Schafer W, Abrams P, Liao LM, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 2002;21:261–74
- Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: report from the of the International Standardisation Sub-Committee Continence Society. Neurourol Urodyn 2002;21:167–78
- Gilmour RF, Churchill BM, Steckler RE, et al. A new technique for dynamic analysis of bladder compliance. J Urol 1993;150:1200–3
- Abrams P. Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: three simple indices to define bladder voiding function. BJU Int 1999;84:14–15
- Schafer W. Analysis of bladder outlet function with the linearized passive urethral resistance relation, LinPURR, and a disease specific approach for grading obstruction – from complex to simple. World J Urol 1995;13:47–58
- Roosen A, Chapple CR, Dmochowski RR, et al. A refocus on the bladder as the originator of storage lower urinary tract symptoms: a systematic review of the latest literature. Eur Urol 2009;56:810–19
- Madersbacher S, Pycha A, Schatzl G, et al. The aging lower urinary tract: a comparative urodynamic study of men and women. Urology 1998;51:206–12
- Madersbacher S, Pycha A, Klingler CH, et al. Interrelationships of bladder compliance with age, detrusor instability, and obstruction in elderly men with lower urinary tract symptoms. Neurourol Urodyn 1999;18:3–13
- Ameda K, Koyanagi T, Nantani M, et al. The relevance of preoperative cystometrography in patients with benign prostatic hyperplasia – correlating the findings with clinical-features and outcome after prostatectomy. J Urol 1994;152:443–7
- Elbadawi A, Yalla SV, Resnick NM. Structural basis of geriatric voiding dysfunction. I. Methods of a prospective ultrastructural urodynamic study and an overview of the findings. J Urol 1993;150:1650–6
- Knutson T, Edlund C, Fall M, Dahlstrand C. BPH with coexisting overactive bladder dysfunction – an everyday urological dilemma. Neurourol Urodyn 2001;20:237–47
- Oelke M, Baard J, Wijkstra H, et al. Age and bladder outlet obstruction are independently associated with detrusor overactivity in patients with benign prostatic hyperplasia. Eur Urol 2008;54:419–26
- Prieto Chaparro L, Sánchez Díaz A, Salinas Casado J. Effect of aging on detrusor function in males. Arch Esp Urol 1997;50:579–83
- Al-Hayek S, Thomas AW, Abrams P. Natural history of detrusor contractility – minimum ten-year urodynamic follow-up in men with bladder outlet obstruction and those with detrusor underactivity. Scand J Urol Nephrol 2004;38:101–8
- Brierly RD, Hindley RG, McLarty E, et al. A prospective controlled quantitative study of ultrastructural changes in the underactive detrusor. J Urol 2003;169:1374–8
- Fry CH, Bayliss M, Young JS, Hussain M. Influence of age and bladder dysfunction on the contractile properties of isolated human detrusor smooth muscle. BJU Int 2011;108(2 Pt 2):E91--6 (Epub. 2010, Nov)