Abstract
Objectives: We evaluated the effect of lifestyle modifications and glycemic control on the efficiency of sildenafil citrate in patients with type-2 diabetes (T2DM) and erectile dysfunction (ED).
Methods: Eighty-three men with ED due to T2DM were included in the study. The Group 1 (n = 41) patients received lifestyle modifications (diet and exercise), and medical treatment for intensive glycemic control. In Group 2 (n = 42), in addition to the intensive glycemic control, the patients were given sildenafil citrate® 100 mg for 2–3 per weeks. The changes in ED were compared between the two groups after three months of treatment.
Results: The mean age was 54.9 ± 9.1 (26–75) years. An increase in the IIEF-5 scores was observed in 23 of 41 patients in Group 1 (44.2%) and 29 of 42 in Group 2 (55.8%). When the changes of the IIEF-5 scores were evaluated, the mean increase was 2.5 in Group 1, and 5.0 in Group 2 (p = 0.012). The mean IIEF changes according to the duration of diabetes were 4.8 in <5 years, 3.6 in 5–10 years and 1.6 in >10 years (p = 0.021).
Conclusions: Glycemic control and lifestyle changes are not solely adequate for a better sexual function in ED due to diabetes, and sildenafil citrate should be used additionally.
Introduction
Erectile dysfunction (ED) is defined as the continuous failure in initiating and maintaining the necessary erection needed for a satisfactory sexual performance [Citation1]. ED has hormonal, vascular, neurogenic and psychogenic causes [Citation2]. Many pathophysiologic mechanisms were defined that can cause ED in patients with diabetes. When compared to the normal population, ED is seen 1.9–4 times more in diabetics [Citation3].
The number of patients particularly with type-2 diabetes mellitus (T2DM) is increasing worldwide [Citation4]. The inadequacy of oral pharmacotherapies in this patient group raises the need for novel therapeutic approaches. Lifestyle changes are recommended as first-line therapies for patients with both diabetes and ED [Citation5,Citation6].
Patients with poor glycemic control are more exposed to the micro and macro vascular complications of diabetes [Citation7]. In addition, it has been reported that poor glycemic control decreases with the efficiency of the phosphodiesterase 5 inhibitor (PDE5i) used for the ED treatment in these patients [Citation1]. Even though the outcomes of the poor glycemic control are widely known, there is no definitive knowledge about how ED progresses when the glycemic control is improved [Citation8].
In the current study, we aimed to investigate the effect of lifestyle changes and glycemic control on the efficiency of sildenafil citrate in patients with ED due to T2DM.
Materials and methods
This study was conducted with 83 men, referred to our outpatient clinic between January 2010 and January 2011 with a complaint of ED and T2DM. This study was approved by the Institutional Review Board (Registration #2010/43) and each patient’s consent for the use of their information was taken in a written form.
Patients that were excluded from the study were; those who were on certain medication that may cause ED (such as thiazide, 5 -α reductase inhibitors and β-blockers), treatments affecting erectile function (such as PDE5-I and testosterone replacement treatment), those who received nitrate or its derivatives, and those with urogenital system malignancy, high-risk cardiovascular disease, chronic liver or kidney failure and a previous history of pelvic surgery. In addition, patients who develop any complications due to the sildenafil medication (such as severe headache, dizziness and dyspepsia) were excluded in the study.
Patients' clinical information regarding the age, presence of HT, smoking status, the duration of diabetes and ED, and medication used for ED was obtained. In addition, weight, height, and the circumflexes of waist and hip were measured upon first admission, and the body mass index (BMI) was calculated dividing the weight by height squared. All patients were measured in the morning after fasting overnight, at iliac crest and umbilical level in the standing position. The severity of ED was evaluated using the first five-question version of International Index of Erectile Function (IIEF-5) [Citation9]. The serum samples obtained in the morning were tested for fasting blood glucose, total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglyceride (TG), glycosylated hemoglobin (HbA1c), total testosterone (TT) and free testosterone (fT).
Patients were randomized into two groups using the simple random sampling. Patients in Group 1 (n = 41) received lifestyle modifications and intense glycemic control. Lifestyle modification consisted of a moderate physical activity of 30–45 min for 3–5 days per week (walking or exercises that increase the movement in joints), and a Mediterranean diet that includes a low amount of saturated fats and red meat, and is rich in grains, dry legumes, green vegetables and fruits with olive oil being the oil source.
In addition to lifestyle modifications and intense glycemic control, Group 2 (n = 42) received oral PDE5i (Viagra®, Pfizer, Turkey) two or three times per week during 3 months. After 3 months, IIEF-5 was evaluated and the laboratory tests were performed again.
Statistical analyses
The Statistical Package for Social Sciences (SPSS) version 13.0 (SPSS Inc., Chicago, IL) was used for statistical analyses. Age, duration of diabetes and ED, BMI, HbA1c, TT and fT values and IIEF-5 scores were presented as mean ± standard deviation (SD), and compared with the values obtained from the t-test. The association between the duration of diabetes and IIEF scores was evaluated with the Kruskal–Wallis test, and temporal changes in IIEF-5 were evaluated using the paired sample t-test. The changes in the erectile functions of the groups were assessed using the χ2 test. p < 0.05 was considered statistically significant in statistical evaluations.
Results
The mean age of the patients was 54.9 ± 9.1 (26–75) years; 55.5 ± 8 years in Group 1, and 54.3 ± 10.1 years in Group 2 (p = 0.560). The mean duration of T2DM and ED, BMI, HbA1c levels and IIEF-5 scores were 94.6 ± 101.3 months, 30.1 ± 33.1 months, 26.9 ± 4.1 kg/m2, 8.0 ± 1.7 and 10.5 ± 7.5, respectively. Following the treatment, BMI, HbA1c levels and IIEF-5 scores were found to be 25.6 ± 3.2 kg/m2, 8.0 ± 1.7 and 10.5 ± 7.5, respectively. There were no differences between the groups regarding age, duration of T2DM and ED, BMI, and IIEF-5 scores and HbA1c levels before treatment ().
Table 1. General characteristics of the groups before treatment.
Hypertension (HT) was present in 39.8% (n = 33/83) of the patients, and 30.1% (n = 25/83) were smoking. When the groups were compared in terms of the presence of HT and smoking, no difference was found (p = 0.376, p = 0.151, respectively).
The mean IIEF-5 scores of patients on admission were 7.8 ± 6.0 in Group 1, and 5.8 ± 5.2 in Group 2 (p = 0.104). A significant increase was observed in the IIEF-5 scores of both groups over the treatment period (p < 0.001). The mean IIEF-5 scores in the follow-up evaluation were 10.2 ± 7.5 in Group 1, and 10.8 ± 7.6 in Group 2 (p = 0.723). When the patients were evaluated regarding the improvement in their IIEF-5 scores, 23 of 41 patients (44.2%) in Group 1 and 29 of 42 patients (55.8%) in Group 2 were found to have increased scores (p = 0.321). The evaluation of changes in the IIEF-5 scores revealed that the mean increase was 2.5 in Group 1, and 5 in Group 2, and the change in IIEF-5 scores were more significant in Group 2 (p = 0.012).
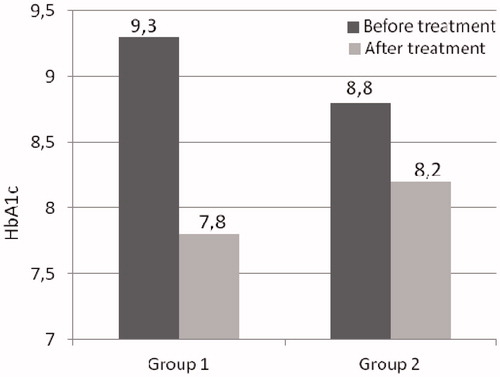
The mean HbA1c values decreased from 9.3 ± 2.9 to 7.8 ± 1.8 in Group 1, and from 8.8 ± 2.1 to 8.2 ± 1.5 in Group 2 (pGroup1 = 0.002, pGroup2 = 0.014, respectively; ) (p < 0.001). However, no difference was found between the groups in terms of the changes in HbA1c levels (p = 0.147).
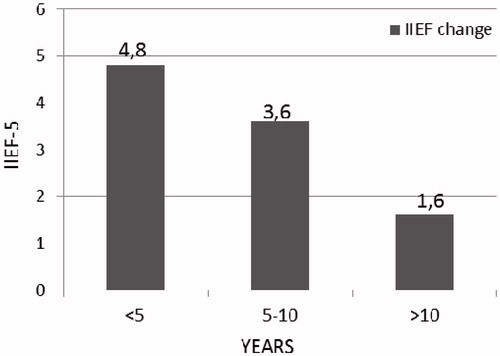
When the patients were evaluated according to the duration of diabetes, the mean IIEF changes were 4.8 in patients with diabetes for >5 years, 3.6 for 5–10 years and 1.6 for >10 years (p = 0.021, ).
Discussion
ED is a concern for 150 million men throughout the world [Citation2,Citation3]. In the Massachusetts Male Aging Study, the prevalence of ED was found to be 52% in men between the ages of 40 and 70 years [Citation10]. Akkus et al. [Citation11] determined the ED prevalence in the 40–70 years age group to be 69.4% in our country. In another study, ED prevalence was found to be 71.4% in 1412 healthy men [Citation12]. The variability of ED prevalence in these studies was reported as due to the methodological differences between the studies [Citation1].
One of the most important risk factors for ED is DM. The prevalence of ED in diabetic patients ranges between 20 and 85% [Citation13]. In addition, the presence of DM has been reported to increase the ED incidence by 3.9 times [Citation10]. Certain mechanisms for ED development have also been identified in diabetes. For example, endothelial damage due to macro/micro-vascular events and microangiopathy in cavernous arteries are more common in diabetic patients [Citation14]. In addition, corporal veno-occlusive dysfunction and autonomic neuropathy are two pathophysiologic causes of ED in these patients [Citation15].
PDE5i is the first-line treatment in patients with ED. Sildenafil citrate was reported to be effective in all subgroups of ED patients [Citation1]. In addition, sildenafil citrate has been reported to be more effective in non-diabetics compared with diabetic patients, and it is effective even in patients with poor glycemic control and patients with complications due to diabetes [Citation16–18]. Berardis et al. [Citation19] carried out a retrospective evaluation of 1456 diabetic patients and reported that the possibility of progression of ED increases with a longer duration of diabetes, poor glycemic control, insulin intake, and retinopathy, neuropathy, and micro/macroalbuminuria. Another study on the importance of glycemic control showed that the risk of ED is 2–5 times higher in DM patients with poor glycemic control compared to patients with good glycemic control [Citation20].
Glycemic control improves the endothelial functions in diabetic patients, and helps to prevent micro- and macro-vascular complications related to diabetes [Citation21]. Several published studies have demonstrated that lifestyle modifications, particularly weight loss and regular exercise improve erectile function, and increase the efficiency of PDE5i [Citation5,Citation18,Citation22]. Yaman et al. [Citation23] carried out a pilot study with 25 male patients, 8 with type-1 diabetes and 17 with T2DM, and found that the mean IIEF-5 scores increased from 16.6 to 17.3. However, in that study, it was reported that glycemic control did not significantly improve the erectile functions in the type-1 DM patients. When compared to the study by Yaman et al. [Citation23], the current study is significant in terms of the simultaneous application of lifestyle modifications and glycemic control. Lifestyle modifications that involve a Mediterranean diet are known to have a positive effect on the erectile functions [Citation22–24]. Therefore, in the current study, patients, in addition to their present treatment, were advised to go on a Mediterranean diet and undertake exercise to increase their physical activity. As a result, the mean IIEF-5 scores of the patients in the current study increased from 6.8 to 10.5 after treatment. The temporal changes in the IIEF-5 scores after treatment were more significant in the group receiving sildenafil citrate (2.5 in Group 1 and 5 in Group 2).
Rhoden et al. [Citation25] reported that the high levels of HbA1c are related with a severe ED in diabetic patients. The studies on diabetic patients showed that a 1% decrease in HbA1c levels reduces the diabetes-related deaths by 21%, the risk of myocardial infarcts by 14%, microvascular complications by 37% and the risk of peripheral vascular disease by 43% [Citation24,Citation25]. Khatana et al. [Citation26] applied cardiac risk lowering behavioral and pharmacologic treatment to 41 patients with T2DM and cardiovascular risk factors, and reported that the decreased blood pressure and HbA1c levels <7 are related with the increase in IIEF-5 scores. Similarly, in a study by Yaman et al. [Citation23], the mean HbA1c levels of patients decreased from 8.9 to 6.5 after treatment but no improvement was observed in erectile functions. In the current study, the mean HbA1c level was initially 9.0. After 3 months of treatment, the HbA1c levels were reduced to 8.0, but remained above the normal levels. The most significant difference between our study and the study by Yaman et al. [Citation23] is that we had a higher number of participants who were only T2DM patients.
Another important risk factor for the development of ED in diabetic patients is the duration of diabetes [Citation22,Citation25,Citation26]. It was reported that the mean time between the development of glucose intolerance and diagnosis was 4–7 years. When the exposure to diabetes increases, the vascular complications of diabetes also increase [Citation27]. When compared with patients that have had diabetes for <5 years, ED is seen three times more than in patients with diabetes for >10 years [Citation26]. A study found no association between the type (type 1 and 2) and duration of diabetes (<10 and ≥10 years) [Citation23]. According to our results, the highest increase in the mean IIEF-5 scores was 4.8 in patients with diabetes for <5 years, and the least increase was 1.6 in patients with diabetes for >10 years. In the light of these findings, it can be speculated that the lower percentage of improvement in diabetes-related ED in patients with longer duration of the disease can be attributed to the increased endothelial dysfunction over time.
The presence of obesity and BMI > 25 kg/m2 have been defined as independent risk factors for endothelial dysfunction [Citation28]. In addition, the increased waist circumflex and abdominal obesity are related with metabolic syndrome (MS), and the presence of MS is related with T2DM and insulin resistance [Citation29]. When the MS, T2DM and ED are considered together, decreasing the BMI of patients to a desired level can contribute to the glycemic control, and improve the erectile capacity by restoring the endothelial functions [Citation30].
Late-onset hypogonadism (LOH) is a clinical and biochemical syndrome occurring with decrease of androgen levels in the aging male [Citation31,Citation32]. Some authors have reported that hypogonadism should be accepted as a classic component of MetS [Citation33]. Almehmadi et al. [Citation34] reported that increased severity of ED within LOH patients correlated with an increased waist circumference, hyperglycemia, hypertriglyceridemia, hyperlipidemia and a history of diabetes mellitus. TRT may have other benefits on metabolic status in aging men with LOH and diabetes and or the MS [Citation35]. In our study, the mean BMI levels were reduced from 26.9 kg/m2 before treatment to 26.5 kg/m2 after treatment. However, the BMI levels of our patients only partially improved. This may be the result of patients’ inadequate compliance with the recommendations regarding the suggested Mediterranean diet and physical activity, or the short follow-up period of 3 months.
There are certain limitations to our study. First, since both lifestyle modifications and PDE5i treatment are known to have a positive effect on erectile functions, only determining the glycemic control efficiency would require one of the patient groups not to receive glycemic control. However, this is not ethically applicable. Second, the patients in the current study had very low IIEF scores before treatment, and the duration of diabetics was long (8–10 years). This may have resulted in poor and slow improvement in patients’ erectile functions. Therefore, we suggest that only lifestyle modifications and Mediterranean diet are not sufficient, and PDE5i therapy should be added to the treatment to improve the erectile functions and facilitate faster rehabilitation. Third, the follow-up of our study is short. However, due to the lack of similar studies in the literature, we believe that it can contribute to predict the success of treatment. Another limitation of our study is using short-acting PDE5-I (sildenafil). The use of long-acting PDE5-I such as tadalafil, could be more helpful.
Conclusions
In conclusion, we determined in our study that lifestyle modifications and glycemic control improved erectile functions in patients with ED due to T2DM. However, since it is not possible to ensure that patients fully comply with the recommended diet and lifestyle modifications, we suggest that PDE5i should be added to the recommendations for a better sexual functioning. We believe that our results should be confirmed by further studies that will be carried out on a higher number of patients with HbA1c and BMI values being decreased to normal levels after a longer duration of glycemic control.
Declaration of interest
The authors report no declarations of interest.
References
- Hatzimouratidis K, Eardley I, Giuliano F, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. European Association of Urology; 2014. Available from: http://uroweb.org/wp-content/uploads/EAU-Guidelines-2015-Male-Sexual-Dysfunction_LR.pdf[last accessed 22 Jul 2015]
- El-Sakka AI. Association of risk factors and medical comorbidities with male sexual dysfunctions. J Sex Med 2007;4:1691–700
- Lewis RW. Epidemiology of erectile dysfunction. Urol Clin North Am 2001;28:209–16
- Satman I, Yilmaz T, Sengül A, et al. The TURDEP Group, population-based study of diabetes and related risk characteristics in Turkey. Diabetes Care 2002;25:1551–6
- Derby CA, Mohr BA, Goldstein I, et al. Modifiable risk factors and erectile dysfunction: can lifestyle changes modify risk? Urology 2000;56:302–6
- Yokoyama Y, Barnard ND, Levin SM, Watanabe M. Vegetarian diets and glycemic control in diabetes: a systematic review and meta-analysis. Cardiovasc Diagn Ther 2014;4:373–82
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2004;27:5–14
- Lu CC, Jiann BP, Sun CC, et al. Association of glycemic control with risk of erectile dysfunction in men with type 2 diabetes. J Sex Med 2009;6:1719–28
- Rosen RC, Riley A, Wagner G, et al. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 1997;49:822–30
- Feldman HA, Goldstein I, Hatzichristou DG, et al. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol 1994;151:54–61
- Akkus E, Kadioglu A, Esen A, et al. Prevalence and correlates of erectile dysfunction in Turkey: a population-based study. Eur Urol 2002;41:298–304
- Braun M, Wassmer G, Klotz T, et al. Epidemiology of erectile dysfunction: results of the “Cologne Male Survey”. Int J Impot Res 2000;12:305–11
- Churdchomjan W, Kheolamai P, Manochantr S, et al. Comparison of endothelial progenitor cell function in type 2 diabetes with good and poor glycemic control. BMC Endocr Disord 2010;7:10–15
- Makimattilla S, Yki-Jarvinen H. Endothelial dysfunction in human diabetes. Curr Diab Rep 2002;2:26–36
- Chitaley K. Type 1 and type 2 diabetic-erectile dysfunction: same diagnosis (ICD-9), different disease? J Sex Med 2009;6:262–8
- El Saka AI. Efficacy of sildenafil citrate in treatment of erectile dysfunction: effect of type 2 diabetes. Eur Urol 2004;46:503–9
- Romeo JH, Seftel AD, Madhun ZT, Aron DC. Sexual function in men with diabetes type 2: association with glycemic control. J Urol 2000;163:788–91
- Esposito K, Giugliano F, Di Palo C, et al. Effect of lifestyle changes on erectile dysfunction in obese men: a randomized controlled trial. JAMA 2004;291:2978–84
- De Berardis G, Pellegrini F, Franciosi M, et al. Clinical and psychological predictors of incidence of self-reported erectile dysfunction in patients with type 2 diabetes. J Urol 2007;77:252–7
- Matfin G, Jawa A, Fonseca VA. Erectile dysfunction: interrelationship of metabolic syndrome. Curr Diabetes Rep 2005;5:64–9
- Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000;321:405–12
- Glina S, Sharlip ID, Hellstrom WJ. Modifying risk factors to prevent and treat erectile dysfunction. J Sex Med 2013;10:115–19
- Yaman Ö, Akand M, Gürsoy A, et al. The effect of diabetes mellitus treatment and good glycemic control on the erectile function in men with diabetes mellitus-induced erectile dysfunction: a pilot study. J Sex Med 2006;3:344–8
- Esposito K, Giugliano F, Maiorino MI, Giugliano D. Dietary factors, Mediterranean diet and erectile dysfunction. J Sex Med 2010;7:2338–45
- Rhoden EL, Riberio EP, Riedner CE, et al. Glycosylated heamoglobin levels and the severity of erectile function in diabetic men. BJU Int 2005;95:615–17
- Khatana SA, Taveria TH, Miner MM, et al. Does cardiovascular risk reduction alleviate erectile dysfunction in men with type 2 diabetes mellitus? Int J Impot Res 2008;20:501–6
- Spijkermen AM, Henry RM, Dekker JM. Prevalence of microvascular disease amongst type 2 diabetic patients detected by targeted screening and patients newly diagnosed in general practice: the Hoorn Screening study. J Intern Med 2004;256:429–36
- Wolczak MK, Lakhmandale N, Hodge MB, Guay AT. Prevalence of cardiovascular risk factor in erectile dysfunction. J Gend Specif Med 2002;5:19–24
- Aslan Y, Sezgin T, Tuncel A, et al. Is type 2 diabetes mellitus a cause of severe erectile dysfunction in patients with metabolic syndrome. Urology 2009;74:561–4
- Wing RR, Rosen RC, Fava JL, et al. Effects of weight loss intervention on erectile function in older men with type 2 diabetes in the Look AHEAD trial. J Sex Med 2010;7:156–65
- Wang C, Nieschlag E, Swerdloff RS, et al. ISA, ISSAM, EAU, EAA and ASA recommendations: investigation, treatment and monitoring of late-onset hypogonadism in males. Aging Male 2009;12:5–12
- Lunenfeld B, Mskhalaya G, Kalinchenko S, Tishova Y. Recommendations on the diagnosis, treatment and monitoring of late-onset hypogonadism in men – a suggested update. Aging Male 2013;16:143–50
- Makhsida N, Shah J, Yan G, et al. Hypogonadism and metabolic syndrome: implications for testosteron therapy. J Urol 2005;174:827–34
- Almehmadi Y, Yassin DJ, Yassin AA. Erectile dysfunction is a prognostic indicator of comorbidities in men with late onset hypogonadism. Aging Male 2015:1–9. [Epub ahead of print]. doi: 10.3109/13685538.2015.1046044
- Saad F, Yassin A, Almehmadi Y, et al. Effects of long-term testosterone replacement therapy, with a temporary intermission, on glycemic control of nine hypogonadal men with type 1 diabetes mellitus – a series of case reports. Aging Male 2015:1–5. [Epub ahead of print]. doi: 10.3109/13685538.2015.1034687