Abstract
Introduction: Several studies have indicated that erectile dysfunction (ED) patients also suffer from lower urinary tract symptoms (LUTS). We investigated a group of men with LUTS and assessed their sexual function with the aim of being able to predict ED risk factors and introduce ED treatments earlier for this patient group.
Methods: International Prostate Symptom Score (IPSS), Overactive Bladder Symptoms Score (OABSS) and Sexual Health Inventory for Men (SHIM) score were obtained from 236 men with LUTS at their first out-patients visit. Clinical parameters such as body mass index, prostate volume, residual urine volume and prostate specific antigen were also evaluated. The relationship between the SHIM score and other clinical data was analyzed.
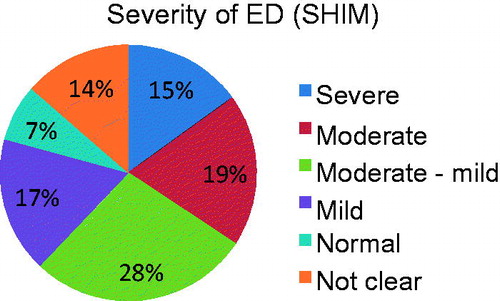
Results: According to the SHIM score, ED in men with LUTS was severe 15%, moderate 19%, moderate to mild 28%, mild 17%, normal 7% and data was incomplete in 14%. Based on the results of a multivariate analysis, aging (p < 0.001) and OAB severity (p = 0.024) were significantly correlated to severe and moderate ED. Furthermore, among OAB symptoms score items, urge urinary incontinence was a risk factor for severe and moderate ED (p = 0.005).
Conclusion: Aging and OAB (notably urinary urge incontinence) are risk factors for severe and moderate ED in men with LUTS.
Introduction
Patients with erectile dysfunction (ED) and late onset hypogonadism (LOH) often suffer from male lower urinary tract symptoms (LUTS) simultaneously [Citation1–2]. Treatment with phosphodiesterase type 5 (PDE 5) inhibitors and testosterone replacement is reported to be effective in alleviating male LUTS in these patients [Citation2–4]. Our study investigated the existence of male LUTS in ED and LOH patients.
LUTS is a very common in elderly men [Citation5–7], and there is a well-established relationship between LUTS and increased BMI and low testosterone [Citation7]. However, some men with LUTS, and especially those in Japan, are hesitant to complain about any sexual dysfunctions. In patients with LUTS, the detection of ED at an earlier stage may allow a successful treatment regime and therefore improves the patient’s well-being.
Aim
To identify the risk factors for ED in male patients with LUTS.
Methods
Two hundred and thirty-six men who attended our outpatient clinic for evaluation of LUTS between April 2011 and March 2013 were assessed. At their first visit they were evaluated by history, physical examination, clinical parameters and questionnaires prior to any treatment for LUTS. The patients in this study had never been administered any LUTS medications, such as alpha-1 blockers, OAB agents, 5 alpha reductase inhibitors or PDE5 inhibitors. Consent was collected from all participants and the study was approved by the institutional ethics committee. The Clinical parameters included body mass index (BMI), prostate volume, residual urine volume and prostate specific antigen (PSA). The patients with prostate cancer, urinary tract infection and neurogenic bladder were excluded from this study.
BMI was calculated as body weight (kg) / height (m)2. Degree of obesity was defined based on the BMI: underweight < 18.5, normal 18.5 – 24.9, overweight 25 – 29.9, and obese ≥30.
Total prostate volume, prostate adenoma volume and residual urine volume were evaluated by trans-rectal and/or trans-abdominal ultrasonography (prosoundalpha 7 R, Hitachi Aloka Medical, Mitaka, Tokyo Japan).
Serum PSA levels were measured using Lumipulse PrestoR PSA (Fujirebio, Tokyo, Japan). The normal range is <4.0 ng / mL.
The International Prostate Symptom Score (IPSS), Over Active Bladder Symptoms Score (OABSS) and Sexual Health Inventory for Men (SHIM) was also obtained. We then compared the results obtained from the questionnaires with the clinical data.
Main outcome measures
To investigate ED risk factors for male LUTS, the relationship between SHIM score and the other clinical data was evaluated. The data and statistical significance were analyzed using SPSS Statistics for Windows, version 22.0 (IBM, Armonk, NY). P < 0.05 indicated statistical significance.
Results
Two hundred and thirty-six men who consecutively presented at the outpatient clinic with LUTS were included in the study. They had a mean age of 69.6 (range 41–88; SD 8.7) years. The distribution of patients with respect to decade of life was 40–49 years 2%; 50–59 years 11%; 60–69 years 36%; 70–79 years 39%; and 80–89 years 12%. Seventy-five percent of the patients were between 60–79 years.
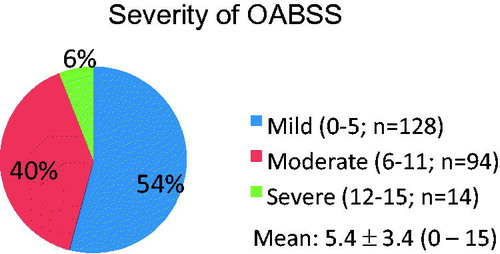
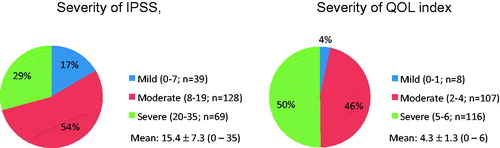
The IPSS in patients indicated mild symptoms 17%, moderate symptoms 54% and severe symptoms in 29%. The quality of life (QOL) index demonstrated mild symptoms 4%, moderate symptoms 46% and severe symptoms in 50%. There was incomplete data from the QOL index in five patients ().
Figure 1. Severity of international prostate symptom score (IPSS) and quality of life (QOL) index in 236 men with LUTS. Mean ± standard deviation of IPSS and QOL index were 15.4 ± 7.3 and 4.3 ± 1.3, respectively. There was incomplete data from the QOL index in five patients.
The OABSS revealed mild symptoms 54%, moderate symptoms 40% and severe symptoms in 6% ().
Severity scores of ED based on the SHIM in men with LUTS were severe 15%, moderate 19%, moderate to mild 28%, mild 17%, normal 7% and incomplete data in 14% ().
Figure 3. Erectile dysfunction severity based on sexual health inventory for men score in 236 men with LUTS.
BMI data showed 5% of the men were underweight (BMI < 18.5), 68% were normal (BMI 18.5 – 24.9), 22% were overweight (BMI 25 – 29.9) and 5% were obese (BMI ≥ 30).
Total prostate volume and prostate adenoma volume evaluated by ultrasonography was 26.5 ± 16.0 (7.0 – 121.0) mL and 11.1 ± 10.0 (1.2 – 92.0) mL, respectively. Total prostate volumes were less than 50.0 mL in 92% of subjects.
Residual urine volume was 31.1 ± 48.5 (0.0 – 225.4) mL and 14% of patients had more than 50.0 mL residual urine volume.
Mean PSA level was 3.7 ± 6.8 (0.13 – 67.4) ng/mL. Patients with high serum PSA levels were referred for further examination and those who were diagnosed with prostate cancer were subsequently excluded from this study.
Univariate analysis (logistic regression analysis) of the relationship between SHIM score and the clinical data of men suggested that age and storage symptoms in IPSS and the OABSS were considered to be severe and moderate ED risk factors (). Furthermore, multivariate analysis with logistic regression analysis showed that age (p < 0.001) and overactive bladder (OAB) (p = 0.024) were considered to be significant risk factors for severe and moderate ED (). In addition, in a multivariate sub-analysis of data for the four OABSS items, age (p < 0.001) and urge urinary incontinence (p = 0.005) were risk factors for severe and moderate ED according to the SHIM score ().
Table 1. Risk factors for a moderate to severe score of ED (SHIM in a univariate analysis).
Table 2. Risk factors for a moderate to severe score of ED (SHIM in a multivariate analysis).
Table 3. Risk factors for a moderate to severe score of ED (SHIM in OABSS items in a multivariate analysis).
Discussion
The aging male suffers from several symptoms, including physiological, psychological and sexually related symptoms that are identified as LOH symptoms [Citation6,Citation7]. Aging, intra-pelvic surgery, diabetes mellitus, LUTS and hypertension have been identified as risk factors for ED [Citation1]. It has also been reported that ED and LOH patients can also suffer from male LUTS [Citation2,Citation4,Citation6,Citation7]. Furthermore, treatments for ED and LOH, including PDE 5 inhibitors and testosterone replacement can also be effective at alleviating male LUTS [Citation2–4]. Therefore, it is crucial to investigate the relationship of male LUTS in ED and LOH patients.
Elderly men with LUTS also often suffer from ED. Their chief complaint to clinicians is urinary disturbances. However, many men with LUTS hesitate to complain about sexual dysfunction.
Several common pathological mechanisms of ED and LUTS have been reported, including a decrease of nitric oxide production, hyperactivity of Rho-A/Rho-kinase (ROCK), hyperactivity of autonomic nerves, arteriosclerosis and ischemia of intra-pelvic vessels [Citation8,Citation9]. The more common treatments for ED and LUTS are PDE 5 inhibitors and alpha-blockers. PDE 5 inhibitors affect urethral and bladder smooth muscle, resulting in improvement of male LUTS [Citation10,Citation11], and alpha-blockers may also improve ED [Citation12,Citation13].
There are two main aspects of male LUTS, voiding and storage symptoms. Some reports have shown a relationship between ED and voiding symptoms [Citation2,Citation14,Citation15], whereas others have indicated that ED and storage symptoms are associated [Citation16–18]. Nocturia has also been reported to influence maintenance of sexual function in elderly men with benign prostate hyperplasia [Citation19].
The current study showed that age (p < 0.001) and OAB (p = 0.024) were significantly correlated to moderate and severe ED. Irwin et al. [Citation20] also reported that an OAB was associated with ED. In addition, in a multivariate sub-analysis of the data for the four OABSS items, urge urinary incontinence was a risk factors of moderate and severe ED as determined by the SHIM score (p = 0.005).
Recently, the PDE5 inhibitor tadalafil has been used to improve male LUTS in benign prostate hypertrophy [Citation3]. OAB treatment with tolterodine has also been reported to be effective on sexual and emotional quality of life in sexually active women [Citation21]. However, the clinical efficacy of OAB treatment for ED has not been shown meaning that further investigation is required.
This present report is a transverse observational study and is limited in terms of identifying the common mechanism of ED and OAB and in examining the interaction efficacy between ED and OAB treatments. However, our data suggest that, among men with LUTS, those with OAB are at high risk for ED. Therefore, the older man who clinically presents with LUTS and urge incontinence should be evaluated for ED.
Conclusion
This questionnaire based study showed that age and OAB (especially urinary urge incontinence) are risk factors for moderate to severe ED in men with LUTS. Further studies are needed including a placebo controlled trial to confirm these findings.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Braun M, Wassmer G, Klotz T, et al. Epidemiology of erectile dysfunction: results of the ‘Cologne Male Survey’. Int J Impot Res 2000;12:305–11
- Amano T, Imao T, Takemae K, et al. Testosterone replacement therapy by testosterone ointment relieves lower urinary tract symptoms in late onset hypogonadism patients. Aging Male 2011;13:242–6
- Yokoyama O, Yoshida M, Kim SC, et al. Tadalafil once daily for lower urinary tract symptoms suggestive of benign prostatic hyperplasia:a randomized placebo-and tamsulosin-controlled 12-week study in Asian men. Int J Urol 2013;20:193–201
- Shigehara K, Sugimoto K, Konaka H, et al. Androgen replacement therapy contributes to improving lower urinary tract symptoms in patients with hypogonadism and benign prostate hypertrophy:a randomized controlled study. Aging Male 2011;14:53–8
- Lepor H. Pathophysiology of lower urinary tract symptoms in the aging male population. Rev Urol 2005;7:S3–11
- Lunenfeld B, Nieschlag E. Testosterone therapy in the aging male. Aging Male 2007;10:139–53
- Lunenfeld B, Mskhalaya G, Zitzmann M, et al. Recommendations on the diagnosis, treatment and monitoring of hypogonadism in men. Aging Male 2015;18:5–15
- McVary K. Lower urinary tract symptoms and sexual dysfunction:Epidemiology and pathophysiology. BJU Int 2006;97(2 suppl):23–8
- Gacci M, Eardley I, Giuliano F, et al. Critical analysis of the relationship between sexual dysfunctions and lower urinary tract symptoms due to benign prostate hyperplasia. Eur Urol 2011;60:809–25
- Morelli A, Filippi S, Comeglio P, et al. Acute vardenafil administration improves bladder oxygenation in spontaneously hypertensive rats. J Sex Med 2010;7:107–20
- Morelli A, Sarchielli E, Comeglio P, et al. Phosphodiesterase type 5 expression in human and rat lower urinary tract tissues and the effect of tadalafil on prostate gland oxygenation in spontaneously hypertensive rats. J Sex Med 2011;8:2746–60
- Lowe FC. Treatment of lower urinary tract symptoms suggestive of benign prostate hyperplasia:sexual function. BJU Int 2005;95:12–18
- Yan H, Zong H, Cui Y, et al. The efficacy of PDE5 inhibitors alone or in combination with alpha-blockers for the treatment of erectile dysfunction and lower urinary tract symptoms due to benign prostatic hyperplasia:a systemic review and meta-analysis. J Sex Med 2014;11:1539–45
- Braun MH, Sommer F, Haupt G, et al. Lower urinary tract symptoms and erectile dysfunction:Co-morbidity or typical “Aging Male” symptoms? Results of the “Cologne Male Survey”. Eur Urol 2003;44:588–94
- Ponholzer A, Temml C, Obermayr R, Madersbacher S. Association between lower urinary tract symptoms and erectile dysfunction. Urology 2004;64:772–76
- Frankel SJ, Donovan JL, Peters TI, et al. Sexual dysfunction in men with lower urinary tract symptoms. J Clin Epidemiol 1998;51:677–85
- Aslan G, Cavus E, Karas H, et al. Association between lower urinary tract symptoms and erectile dysfunction. Arch Androl 2006;52:155–62
- Leliefeld HH, Stoevelaar HJ, McDonnell J. Sexual function before and after various treatments for symptomatic benign prostate hyperplasia. BJU Int 2002;89:208–13
- Ishizuka O, Matsuyama H, Sasaki H, et al; the KING study group. Nocturia potentially influences maintenance of sexual function in elderly men with benign prostate hyperplasia. LUTS 2013;5:75–81
- Irwin DE, Milsom I, Reilly K, et al. Overactive bladder is associated with erectile dysfunction and reduced sexual quality of life in men. J Sex Med 2008;5:2904–10
- Rogers R, Bachmann G, Jumadilova Z, et al. Efficacy of tolterodine on overactive bladder symptoms and sexual and emotional quality of life in sexually active women. Int Urogynecol J 2008;19:1551–7