Abstract
Background: Colorectal cancer screening in the form of faecal occult blood (FOB) testing can significantly reduce the burden of this disease and has been used as early as the 1970s. Effective involvement of GPs along with reminding physicians prior to seeing a patient may improve uptake. Objective: This article is a systematic review of published literature examining the uptake of FOB testing after physician reminders as part of the colorectal cancer screening process. Methods: Electronic databases were searched from January 1975 to October 2010. All studies comparing physician reminders (Rem) with controls (NRem) were identified. A meta-analysis was performed to obtain a summary outcome. Results: Five comparative studies involving 25 287 patients were analyzed. There were 12 641 patients were in the Rem and 12 646 in the NRem group. All five studies obtained a higher percentage uptake when physician reminders were given. However, in only two of the studies were the percentage uptake significantly higher. There was significant heterogeneity among trials (I2 = 95%). The combined increase in FOB test uptake was not statistically significant (random effects model: risk difference = 6.6%, 95% CI: −2–14.7%; z = 1.59, P = 0.112).
Conclusion: Reminding physicians about those patients due for FOB testing may not improve the effectiveness of a colorectal cancer screening programme. Further studies are required and should focus on areas where there is a lower baseline uptake and areas with high levels of deprivation.
Introduction
Colorectal cancer is the second leading cause of cancer mortality in the UK with over 35 000 cases and 16 000 deaths in 2004 (Citation1). Colorectal cancer screening in the form of faecal occult blood (FOB) testing can significantly reduce the burden of this disease and has been used as early as the 1970s (Citation2,Citation3). FOB testing has demonstrated reduction in mortality by detecting colorectal cancer at an early stage. It is acceptable and consistent with established screening principles (Citation4). Despite this important public health impact, uptake of FOB tests during the second pilot phase in England was only 52% and dropped to under 40% in people from areas of high deprivation (Citation5).
Many reasons exist for low uptake, from patient-specific barriers to physician perception and lack of communication (Citation6). Patients often suggest poor motivation, lack of awareness or recommendation from professionals as key factors for deciding not to undertake screening (Citation7). Currently general practitioners (GPs) are not directly involved in the colorectal screening programme in the UK. Some reports suggest that due to time pressures, physician-reminding systems may improve screening (Citation8). GPs are the first point of call for patients and have access to most of patients in the UK including the older population, which means that they must be an integral part of a screening programme. GPs are also the primary source of information regarding screening processes (Citation9–11). Furthermore, we know that the uptake is higher amongst patients when a physician recommends screening as seen in other settings (Citation12–15). GPs already have an intrinsic role in prompt diagnosis and investigation along with counselling patients on benefits and pitfalls of a particular screening program (Citation16,Citation17). Effective involvement of GPs along with reminding physicians prior to seeing a patient may improve uptake (Citation18).
There are various ways of delivering reminders to physicians and we focused on any mechanism (e.g. electronic or memorandum) that would highlight or ‘flag-up’ to a doctor that a patient was due for screening. Primary care tools such as a coordinated reminding system to undertake this may require careful national cooperation but benefits have been seen in other settings (Citation19). The focus of UK screening programmes has been reliant on FOB especially since the ScHARR report, which demonstrated effectiveness of FOBT for reducing mortality as well as being the least expensive and safest modality available (Citation20–22). If implemented appropriately, this intervention may reduce mortality by approximately 16% for those participating in screening at least once and detect cancers at an earlier stage (Citation23).
The objective of this systematic review is to examine whether the use of reminders to physicians increases the uptake of FOB testing.
Methods
Searching and selection
All studies comparing reminders to physicians (Rem) with controls (NRem) between January 1970 and October 2010 were identified. We searched the MEDLINE, EMBASE and CINAHL databases available through the NHS National Library of Health website, the Cochrane library and PubMed available online. The text words ‘faecal occult blood,’ ‘screening,’ ‘reminders,’ ‘physician reminders,’ ‘physician role,’ ‘colon cancer’ and ‘rectal cancer’ were used in combination with the medical subject heading ‘mass screening’ and ‘colorectal cancer.’ Two authors excluded irrelevant articles, reviews and meta-analyses evident from the titles and abstracts (MRSS and KK). Relevant articles referenced in these publications were obtained and the references of identified studies were searched to identify any further studies. No language restriction was applied. A third researcher (MSS) confirmed study selection. Only comparative studies looking at Rem versus NRem relating to the uptake of colorectal cancer screening were included. We excluded studies not fulfilling our inclusion criteria, those that did not focus on FOB uptake and those that did not give specific data or individual patient data.
Data extraction
Each included article according to our selection criteria (comparative studies examining FOB testing for colorectal cancer screening in any language involving patients of any age and sex—) was critically reviewed by two researchers using a double extraction method for eligibility. This was performed independently and if any conflict arose resolution was through discussion with the authors prior to analysis.
Table I. Inclusion criteria.
Our outcome variable was the uptake of FOB after introducing reminders to doctors seeing patients in a hospital clinic or in a primary care setting.
Quality assessment
The methodological quality of included trials is explained comprehensively in . Assessment was based on a combined system using Chalmers et al. and Jadad et al. criteria, and was performed by two authors independently (MRSS & MSS) (Citation24–27).
Table II. Modified quality score for randomized controlled trials, Jadad et al. (Citation27) Chalmers et al. (Citation26).
Data synthesis
A senior statistician using Microsoft Excel 2003 performed statistical analysis. We reported our outcome as risk differences and combined studies using the Mantel-Haenszel method under the fixed effects model and the DerSimonian and Laird method under the random effects model (Citation28). A forest plot was used for the graphical display. A P-value less than 0.05 was deemed to indicate a statistically significant difference. Heterogeneity of the studies was assessed according to Q and I2. If the heterogeneity was significant a random effects method was used otherwise a fixed effects method was utilized. The decision to use a random effects model if heterogeneity existed, and continue with a quantitative analysis rather than a qualitative one, was that we expected a degree of heterogeneity due to different reminding techniques. However, the agreement amongst the authors was that any reminding mechanism should give the same direction effect but that the effect size may differ. Pooling of the studies was thus still considered valid.
Results
Search results
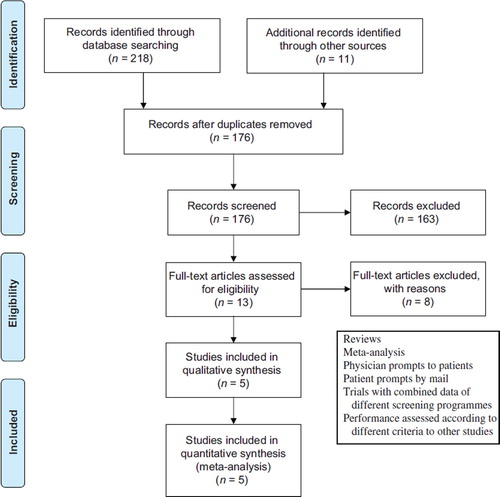
A flow chart of the literature search is shown in . Twelve trials comparing Rem with NRem were retrieved from the electronic databases (Citation29–40). Five prospective randomized studies on 25 287 patients met the inclusion criteria and qualified for the review () (Citation36–40). Seven trials were excluded due to unusable data or if they investigated individual primary care practices and physicians (Citation29–35). Some data was given as a proportion increase in uptake but gave no baseline, and hence data could not be used for meta-analysis (Citation32,Citation34) (). The studies we included incorporated both hospital clinic and primary care visits by adult patients.
Table III. Excluded trials.
Characteristics of included trials
outlines the individual characteristics for each trial. Sequist et al., used electronic reminders to physicians during office visits with their patients who were overdue for screening (Citation38). Physicians were able to view the reminder at any time (passive) and were actively reminded when attempting to place an electronic order (active). The study by Vinker et al., used a note placed in the patient file to remind physicians of the need to suggest screening, in addition patients were also reminded using a letter or phone call (Citation37). Ornstein et al., and Becker et al., used memorandums, which may be attached to the patient's file to remind physicians (Citation36,Citation40). Weingarten et al., used a computerized system where a list was displayed on screen to highlight the need for screening (Citation39).
Table IV. Reminder protocols for trials.
Results of quality assessment
The results of quality assessment can be found in . Generally the articles available in the literature were not of excellent quality. Sequist et al. had the most robust methodology describing a double blind randomized trial with inclusion and exclusion criteria (Citation38). The methodology was weakened by lack of sample size calculation and no mention of whether there was any missing post intervention data or not. Three studies all stated their inclusion criteria, study period and had obvious quantitative endpoints (Citation36,Citation39,Citation40). Furthermore, Becker et al., described their study as double blind and gave exclusion criteria (Citation36). Vinker et al. was the weakest paper and only stated inclusion criteria, statistical analyses performed and that it was a randomized trial (Citation37). The methodological strength of this paper was that it performed an analysis according to the intention to treat basis, which was missing in three of the other studies.
Uptake of FOB testing
There were 12 641 patients in the Rem group and 12 646 in the NRem group. Data on FOB testing was extracted and tabulated as shown in . All five studies included in the meta-analysis obtained a higher percentage uptake when physician reminders were given. However, in only two of the studies (Vinker et al. and Ornstein et al.) were the percentage uptake significantly higher (Citation37, Citation40). Using the Mantel-Haenszel method, there was significant heterogeneity among trials (Q = 104.5, df = 4, P < 0.001, I2 = 0.007, I2 = 95%) and, therefore, the fixed effects model was inappropriate (Citation36–40). Using the DerSimonian and Laird method, the combined increase was not statistically significant (random effects model: risk difference = 6.6%, 95% CI: −2–14.7%; z = 1.59, P = 0.112; ).
Table V. Outcome variables.
Discussion
The focus of UK screening programmes has been reliant on FOB especially since the ScHARR report, which demonstrated effectiveness of FOBT for reducing mortality as well as being the least expensive and safest modality available (Citation20–22). If implemented appropriately, this intervention may reduce mortality by approximately 16% for those participating in screening at least once and detect cancers at an earlier stage (Citation23).
Main findings
This systematic review suggests that prompting physicians does not lead to improvement to the uptake of FOB testing. These reminders to physicians were in the form of a computerized message or memorandum placed on the front of the case notes. Our finding is contrary to some reports suggesting that physicians pay more attention to adherence of colorectal screening guidelines as a result of reminders (Citation18). Our results are supported by the most recent study (Citation38). However, Sequist et al. suggest that the number of patient visits has a role to play in whether reminders to physicians increase FOB uptake (Citation38).
Strengths of review
The main strength of this review is its systematic approach and inclusion of the study by Sequist et al. It highlights the paucity of literature on this intervention and the move towards a multi-intervention approach to increase the uptake in screening.
Limitations
At study level and outcome level. Different insurance levels and health care systems may lead to varying uptakes because of presence or lack of incentives for doctors (Citation37). Some patients due for screening did not attend their primary care practitioner and the ‘reminding mechanism’ did not take place.
The main source of heterogeneity was the paper by Vinker et al., displaying a significantly favourable outcome in the Rem group and may relate to the age group analyzed, the use of a memorandum attached to the patients file as a reminder or a population in which the baseline uptake of FOB testing was low (Citation37). Baseline uptake in the Vinker study was <2% (increasing to 16% uptake with intervention) whilst baseline for studies such as Ornstein et al., was 18% and the intervention group had an increase of 5% uptake (Citation40). The proportional increase in uptake suggests that a lower baseline rate may result in greater uptake. This hypothesis has been observed in other screening settings such as breast screening (Citation41). Furthermore, earlier studies had a lower baseline-screening rate, which may impact on overall increase in uptake (Citation32,Citation42,Citation43). These trials may not be applicable to societies where screening rates are reasonably high (Citation38).
The mean age ranged between 40 and 60 with one study just commenting on the comparable nature between control and intervention (Citation36–40). Vinker et al. showed that the greater the age the higher the compliance and this may contribute to heterogeneity (Citation37). Race may affect susceptibility of any proposed intervention (Citation40). Vinker et al. found a different uptake rate amongst older as compared to younger patients (Citation37). Another difference was that they followed up patients with a telephone call effectively introducing another intervention (patient reminder) and this may also contribute to the large increase in uptake.
The studies included in this meta-analysis displayed significant heterogeneity and may result from different reminder techniques (computerized versus non-computerized). Sequist et al. and Weingarten et al. used computerized systems, whereas the other three studies did not (Citation38,Citation39). Furthermore Weingarten et al. used the computer system as a method of documentation rather than an active reminder system whereas Sequist et al. used computers actively and passively to remind physicians for the test. Physicians were also educated prior to the intervention in 2 studies and this may affect the motivation and outcome of FOB uptake by patients (Citation38, Citation40). Sequist et al. identified that patient education had a greater impact on increased screening rates (Citation38). Time pressures during brief clinic visits may pose a challenge as well as different physician choices of first line screening tests (colonoscopy versus FOB testing) (Citation38).
At review level. The weaknesses of this systematic review are the limited number of studies, heterogeneity and exclusion of some studies, which showed an increase in FOB uptake after reminders but could not be included due to lack of data. These studies showed uptake increased by 11–14% with use of reminders (Citation32,Citation34). Furthermore, there were differences in quality between studies and a re-meta-analysis should be performed when better quality trials are available.
Other limitations to our study include the use of assessments of papers according to set criteria. Whilst this may give an indication to study strength it may not highlight other potential weaknesses such as detailed inter-study differences. Although all were randomized, there were significant weaknesses in all but Sequist et al. (Citation38). Vinker et al. showed a markedly positive result despite being the weakest study (Citation37). However, with inclusion of this paper, the risk difference does not achieve significance. This is in contrasts with Sequist et al. (Citation38) (highest quality score), which showed no difference. This interstudy difference may be because of the quality differences. Other reasons could be due to the higher baseline screening levels and the fact that about a third of patients in the trial by Sequist et al. did not attend their primary care practice (Citation38).
Interpretation in the context of other literature
Some non-comparative studies contradict our findings (12% uptake in one study) whilst other articles suggest increased uptake using different types of physician prompts such as checklists or flow-sheets (Citation30–32, Citation44,Citation45). Two meta-analyses conducted on computer-based reminders and FOB combined with other screening tests other than FOB testing suggest a positive role of reminding physicians (Citation42,Citation43) and is consistent with other individual studies excluded from this meta-analysis reporting 11–14% uptake after incorporation of a computer reminder system (Citation32,Citation34). One review looked at computerized reminders to physicians only and indicated an increased uptake of 20% in FOB testing (Citation46). However, most of these studies were conducted before well-established screening programmes and further trials need to be conducted within this context.
Implications for further studies and primary healthcare
Our results may be supportive of the idea that a multi-intervention process is required to improve the uptake of screening and also suggests work is required to examine the impact of reminding physicians, who see specific patient sub-sets evident from the individual studies. These trials should focus on people from areas of high deprivation, age, sex and populations, in which there is a lower baseline uptake to establish a threshold where reminders may no longer be needed.
In the UK, the baseline uptake is 40% in people from areas of high deprivation. Therefore, using reminders may improve this situation. The role of these reminders and subsequent uptake of screening may also be affected by the type of health care provision (National or Private) (Citation40). In the UK, increasing screening rates to 60% or 80% may lead to 13–17% and 12–15% reduction in mortality in men and women respectively (Citation47). A Cochrane review is currently underway exploring all potential interventions leading to improved screening rates (Citation48). Other ways of improving uptake may include patient reminders, public health campaigns and physician reminders to patients.
Summary
All the analysed trials were randomized and the summative outcome suggests the use of prompts does not increase FOB test uptake. Further randomized trials, are required to identify clearly whether there is a benefit of reminders in certain population groups.
Conclusion
Reminding physicians about those patients due for FOB testing may not improve the effectiveness of a colorectal cancer screening programme however, further studies focusing on people from areas of high deprivation, age, sex and populations, in which there is a lower baseline uptake are required.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Parkin DM, Olsen AH, Sasieni P. The potential for prevention of colorectal cancer in the UK. Eur J Cancer Prev. 2009;18:179–90.
- Towler B, Irwig L, Glasziou P, Kewenter J, Weller D, Silagy C. A systematic review of the effects of screening for colorectal cancer using the faecal occult blood test, hemoccult. Br Med J. 1998;317:559–65.
- Holt DC, Simpson RG. Occult blood in faeces. Lancet 1970;1:39.
- Wilson JM, Jungner YG. Principles and practice of mass screening for disease. Bol Oficina Sanit Panam. 1968;65: 281–393.
- Weller D, Coleman D, Robertson R, Butler P, Melia J, Campbell C, . The UK colorectal cancer screening pilot: Results of the second round of screening in England. Br J Cancer 2007;97:1601–5.
- Kelly KM, Phillips CM, Jenkins C, Norling G, White C, Jenkins T, . Physician and staff perceptions of barriers to colorectal cancer screening in Appalachian Kentucky. Cancer Control 2007;14:167–75.
- Klabunde CN, Vernon SW, Nadel MR, Breen N, Seeff LC, Brown ML. Barriers to colorectal cancer screening: A comparison of reports from primary care physicians and average-risk adults. Med Care 2005;43:939–44.
- Stone EG, Morton SC, Hulscher ME, Maglione MA, Roth EA, Grimshaw JM, . Interventions that increase use of adult immunization and cancer screening services: A meta-analysis. Ann Intern Med. 2002;136:641–51.
- Bulpitt CJ, Fletcher AE. The role of the physician in geriatric medicine in the ageing society. Screening in the community. Age Ageing. 1994;23 Suppl. 3:S18–21.
- Borum ML, Shafa S, Hatara MC, Paulsen J. The primary care physician may have a more critical role in colorectal cancer screening in African Americans when compared to non-African Americans. J Natl Med Assoc. 2009;101:734.
- Christie J, Itzkowitz S, Lihau-Nkanza I, Castillo A, Redd W, Jandorf L. A randomized controlled trial using patient navigation to increase colonoscopy screening among low-income minorities. J Natl Med Assoc. 2008;100:278–84.
- MacDowell NM, Nitz-Weiss M, Short A. The role of physician communication in improving compliance with mammography screening among women ages 50–79 in a commercial HMO. Manag Care Q. 2000;8:11–9.
- Ferrante JM, Gonzalez EC, Pal N, Roetzheim RG. Effects of physician supply on early detection of breast cancer. J Am Board Fam Pract. 2000;13:408–14.
- Campbell RJ, Ramirez AM, Perez K, Roetzheim RG. Cervical cancer rates and the supply of primary care physicians in Florida. Fam Med. 2003;35:60–4.
- Roetzheim RG, Pal N, Gonzalez EC, Ferrante JM, Van Durme DJ, Ayanian JZ, . The effects of physician supply on the early detection of colorectal cancer. J Fam Pract. 1999;48:850–8.
- Grunfeld E. Cancer survivorship: A challenge for primary care physicians. Br J Gen Pract. 2005;55:741–2.
- Miser WF. Cancer screening in the primary care setting: The role of the primary care physician in screening for breast, cervical, colorectal, lung, ovarian, and prostate cancers. Prim Care 2007;34:137–67.
- Litzelman DK, Dittus RS, Miller ME, Tierney WM. Requiring physicians to respond to computerized reminders improves their compliance with preventive care protocols. J Gen Intern Med. 1993;8:311–7.
- White MJ, Stark JR, Luckmann R, Rosal MC, Clemow L, Costanza ME. Implementing a computer-assisted telephone interview (CATI) system to increase colorectal cancer screening: A process evaluation. Patient Educ Couns. 2006; 61:419–28.
- UK CRC Screening Pilot Examination Team. Evaluation of the UK colorectal cancer screening pilot. Edinburgh: National Health Service; 2003.
- Tappenden P, Eggington S, Nixon R, Chilcott J, Sakai H, Karnon J. Colorectal cancer screening options appraisal: Cost-effectiveness, cost-utility and resource impact of alternative screening options for colorectal cancer. Report to the English Bowel Cancer Screening Working Group, September 2004. http://www.cancerscreening.org.uk/bowel/scharr.pdf
- Chorost MI, Datta R, Santiago RC, Lee B, Bollman J, Leitman IM, . Colon cancer screening: Where have we come from and where do we go? J Surg Oncol. 2004;85: 7–13.
- Hewitson P, Glasziou P, Irwig L, Towler B, Watson E. Screening for colorectal cancer using the faecal occult blood test, Hemoccult. Cochrane Database Syst Rev. 2007:CD001216.
- Rangel SJ, Kelsey J, Colby CE, Anderson J, Moss RL. Development of a quality assessment scale for retrospective clinical studies in pediatric surgery. J Pediatr Surg. 2003; 38:390–6.
- SIGN guidelines. Available from: http://www.sign.ac.uk/guidelines/fulltext/50/checklist3 (accessed 20 March 2009);
- Chalmers TC, Smith H, Jr, Blackburn B, Silverman B, Schroeder B, Reitman D, . A method for assessing the quality of a randomized control trial. Control Clin Trials 1981;2:31–49.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, . Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials 1996;17:1–12.
- Egger M, Smith GD, Altman DG. Systematic reviews in healthcare. London: BMJ Publishing; 2006.
- Williams RB, Boles M, Johnson RE. A patient-initiated system for preventive health care. Arch Fam Med. 1998;7: 338–45.
- Turner BJ, Day SC, Borenstein B. A controlled trial to improve delivery of preventive care: Physician or patient reminders? J Gen Intern Med. 1989;4:403–9.
- McPhee SJ, Bird JA, Jenkins CN, Fordham D. Promoting cancer screening. A randomized, controlled trial of three interventions. Arch Intern Med. 1989;149:1866–72.
- McPhee SJ, Bird JA, Fordham D, Rodnick JE, Osborn EH. Promoting cancer prevention activities by primary care physicians. Results of a randomized, controlled trial. JAMA 1991;266:538–44.
- McDonald CJ, Hui SL, Simith DM, Tierney WM, Cohen SJ, Weinberger M, . Reminders to physicians from an introspective computer medical record. Ann Int Med. 1984;100: 130–8.
- Frame PS, Zimmer JG, Werth PL, Hall WJ, Eberly SW. Computer-based vs manual health maintenance tracking. A controlled trial. Arch Fam Med. 1994;3:581–8.
- Fordham D, McPhee SJ, Bird JA, Rodnick JE, Detmer WM. The cancer prevention reminder system. MD Comp. 1990; 7:289–95.
- Becker DM, Gomez EB, Kaiser DL, Yoshihasi A, Hodge RH, Jr. Improving preventive care at a medical clinic: How can the patient help? Am J Prev Med. 1989;5:353–9.
- Vinker S, Nakar S, Rosenberg E, Kitai E. The role of family physicians in increasing annual fecal occult blood test screening coverage: A prospective intervention study. Isr Med Assoc J. 2002;4:424–5.
- Sequist TD, Zaslavsky AM, Marshall R, Fletcher RH, Ayanian JZ. Patient and physician reminders to promote colorectal cancer screening: A randomized controlled trial. Arch Intern Med. 2009;169:364–71.
- Weingarten MA, Bazel D, Shannon HS. Computerized protocol for preventive medicine: A controlled self audit in family practice. Fam Prac. 1989;6:120–4.
- Ornstein SM, Garr DR, Jenkins RG, Rust PF, Arnon A. Computer-generated physician and patient reminders. Tools to improve population adherence to selected preventive services. J Fam Pract. 1991;32:82–90.
- Lewis CL, Brenner AT, Griffith JM, Pignone MP. The uptake and effect of a mailed multi-modal colon cancer screening intervention: A pilot controlled trial. Implement Sci. 2008; 3:32.
- Balas EA, Weingarten S, Garb CT, Blumenthal D, Boren SA, Brown GD. Improving preventive care by prompting physicians. Arch Intern Med. 2000;160:301–8.
- Shea S, DuMouchel W, Bahamonde L. A meta-analysis of 16 randomized controlled trials to evaluate computer-based clinical reminder systems for preventive care in the ambulatory setting. J Am Med Inform Assoc. 1996;3:399–409.
- Prislin MD, Vandenbark MS, Clarkson QD. The impact of a health screening flow sheet on the performance and documentation of health screening procedures. Fam Med. 1986; 18:290–2.
- Davidson RA, Fletcher SW, Retchin S, Duh S. A nurse-initiated reminder system for the periodic health examination. Implementation and evaluation. Arch Intern Med. 1984;144:2167–70.
- Dexheimer JW, Sanders DL, Rosenbloom ST, Aronsky D. Prompting clinicians: a systematic review of preventive care reminders. AMIA Annu Symp Proc. 2005:938.
- Parkin DM, Tappenden P, Olsen AH, Patnick J, Sasieni P. Predicting the impact of the screening programme for colorectal cancer in the UK. J Med Screen. 2008;15:163–74.
- Flight IHK, Wilson CL, Griffiths L, Myers RE. Interventions for improving uptake of population-based screening for colorectal cancer using faecal occult blood testing. Cochrane Database of Systematic Reviews. 2004:CD005035.