Abstract
Background: Conflicting data on the diagnostic and prognostic value of auscultation abnormalities may be partly explained by inconsistent use of terminology.
Objectives: To describe general practitioners use of chest auscultation abnormality terms for patients presenting with acute cough across Europe, and to explore the influence of geographic location and case mix on use of these terms.
Methods: Clinicians recorded whether ‘diminished vesicular breathing’, ‘wheezes’, ‘crackles’ and ‘rhonchi’ were present in an observational study of adults with acute cough in 13 networks in 12 European countries. We describe the use of these terms overall and by network, and used multilevel logistic regression to explore variation by network, controlling for patients’ gender, age, comorbidities, smoking status and symptoms.
Results: 2345 patients were included. Wheeze was the auscultation abnormality most frequently recorded (20.6% overall) with wide variation by network (range: 8.3–30.8%). There was similar variation for other auscultation abnormalities. After controlling for patient characteristics, network was a significant predictor of auscultation abnormalities with odds ratios for location effects ranging from 0.37 to 4.46 for any recorded auscultation abnormality, and from 0.25 to 3.14 for rhonchi.
Conclusion: There is important variation in recording chest auscultation abnormalities by general practitioners across Europe, which cannot be explained by differences in patient characteristics. There is a need and opportunity for standardization in the detection and classification of lung sounds.
KEY MESSAGE:
Accurate and reliable interpretation of chest auscultation is important to quality clinical care, for example in implementing clinical prediction rules and treatment guidelines.
There is a large variation across Europe in the recording of auscultation abnormality terms for patients presenting with acute cough.
This variation cannot be accounted for by variation in case mix; suggesting that there is inconsistency in the way these terms are used.
INTRODUCTION
Chest auscultation has been a central part of the diagnostic examination in patients with acute cough/lower respiratory tract infections (LRTI), since the technique was first described by Laënnec in 1819 (Citation1).
However, there is conflicting evidence about the predictive value of auscultation findings in the diagnosis of pulmonary diseases, for instance whether auscultation helps differentiate patients with pneumonia from those who do not have this disease. Crackles on chest auscultation, a finding that strongly influences general practitioners to diagnose pneumonia, is recorded only slightly more frequently in patients with radiographic pneumonia compared to patients with other respiratory tract infections, with likelihood ratios ranging from 1.6 to 3.7 (Citation2,Citation3). Furthermore, auscultation abnormalities do not predict prognosis in patients with LRTI, or differentiate viral from bacterial LRTI (Citation4,Citation5).
Despite limited evidence that patients with acute cough who have auscultation abnormalities have a worse prognosis, abnormal findings on auscultation commonly are associated with clinicians’ decisions to prescribe antibiotics (Citation6–9). This is important because unnecessary prescription of antibiotics drives antibiotic resistance. If auscultation abnormalities are weak predictors of benefit from antibiotics, then clinicians should take this into account in their management decisions and thus reduce unnecessary antibiotic prescribing.
Conflicting data on the diagnostic and prognostic value of auscultation abnormalities may be explained by variation in chest auscultation skills and variation in the terms used to describe auscultation findings. Much of the confusion stems from errors in the translation of the terms used by Laennec, leading to different uses of the terms ‘rales’, ‘crackles’, ‘rhonchi’ and ‘crepitations’. Various attempts have been made to develop a standardized nomenclature (Citation10–13). However, use of terminology still may vary from clinician to clinician and between countries, but the extent of this variation is unknown. Lack of standardization of reporting clinical findings is likely to hamper the implementation of international clinical guidelines promoting improved standards of care. Similarly, the conduct of clinical research and interpretation of research findings will not be uniform when the use of terms for clinical signs varies by the clinician and setting. Understanding variation is a prerequisite to developing and implementing interventions aimed at reducing unhelpful variation.
We set out to: (Citation1) describe the epidemiology of auscultation abnormality terms used by primary care clinicians in the assessment of adults with acute cough in European primary care research networks; and (Citation2) investigate the influence of network location and case mix on the use of these terms.
METHODS
Study design
We conducted a prospective observational study as part of the Genomics to combat Resistance against Antibiotics in Community-acquired lower respiratory tract infections in Europe (GRACE) (http://www.grace-lrti.org) Network of Excellence.
Selection of study subjects
We recruited adult patients presenting to their general practitioner between October and November 2006 and from late January to March 2007, in 14 primary care networks located in 13 European countries, with an illness where an acute or worsened cough was the dominant symptom or whose clinical presentation suggested a LRTI. The study has been described in detail elsewhere (Citation14–22).
Measurements
Clinicians completed a case report form (CRF) for each eligible patient, which asked whether they performed chest auscultation and if so, to record their findings using four categories, namely the presence or absence of diminished vesicular breathing, wheezes, crackles, and rhonchi. Clinicians also recorded the patient's temperature and the presence or absence of symptoms, including phlegm production; shortness of breath; wheezing (as experienced by the patient); fever during illness; chest pain; and feeling generally unwell on the CRF. Patients were also given a symptom diary to complete. In addition to asking about the daily presence or absence of a range of symptoms and medication use, participants were asked about their smoking status. Case report forms and patient diaries were translated into local languages by the research teams in each network (). A primary care clinician in each network conducted or supervised the translation, and all documents were back translated by an independent translator and assessed for accuracy by the research team in Cardiff. For one network (Balatonfured), concerns were raised about the accuracy of the translation of auscultation abnormality terms and so this network has been excluded from the analysis, leaving 13 networks in 12 European countries. Patients who had an auscultation performed and results recorded in a CRF and who returned their symptom diary were included in this study.
Table 1. Auscultation abnormality terms used in each country.
Outcomes and analysis
We recorded the number of patients, overall and by the network, with each auscultation abnormality and any one of the four auscultation abnormalities. Multilevel (patients nested within clinicians) logistic regression models were used to identify significant predictors of the four auscultation findings listed above, and of ‘any auscultation abnormality.’ These models controlled for clinical presentation by including information on patient's gender, age (whether they were over 65 years of age or not), presence of respiratory, heart or diabetic comorbidities, presence of each of the symptoms listed above, smoking status (classified as non-smoker, current smoker and ex-smoker), and the network where the patient presented as covariates in the models. Associations between these covariates and each of the four auscultation findings, as well as ‘any auscultation finding’ were summarized using odds ratios, 95% confidence intervals.
RESULTS
Study population
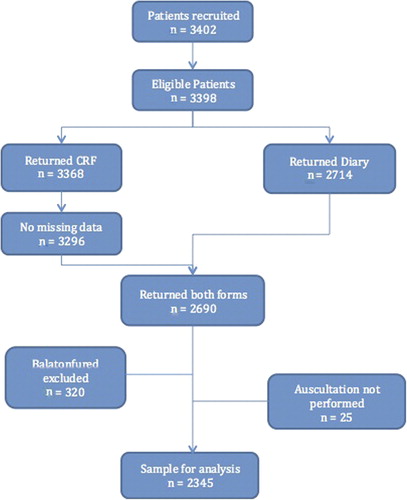
We recruited 3398 eligible patients and 2345 met the inclusion criteria for the analysis (). The mean age of participants was 49 years and 64.4% were female. Pulmonary comorbidity was registered in 15.6% (n = 365), cardiovascular co-morbidity in 9.0%, and diabetes in 4.8%. The frequency of current smoking and reported symptoms both varied considerably between networks ().
Table 2. Participant characteristics by primary care network.
Outcomes
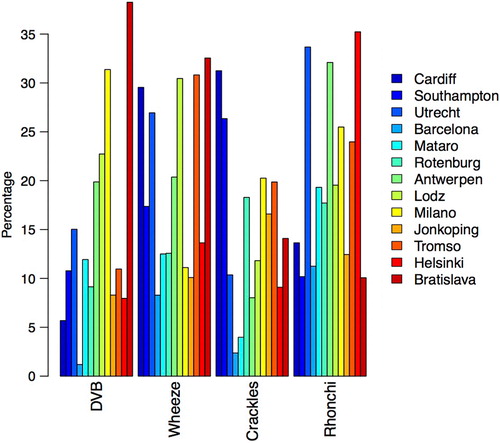
One or more of the four categories of abnormal findings on chest auscultation was recorded in 46.6% (n = 1093) of participants overall, with considerable variation between networks. Wheeze was the most frequent finding overall, occurring in 20.6% patients overall. However, use of this term varied from 8.3% of patients in the Barcelona network to 30.8% in the Tromsø network. Rhonchi, diminished vesicular breathing, and crackles were recorded in 19.1%, 16.2% and 14.8% of all patients, respectively. Diminished vesicular breathing was the term with most variation in use, ranging from 1.2% in the Barcelona network to 38.3% in the Bratislava network ().
After investigating patient characteristics, network was found to predict the presence of auscultation abnormalities. The odds ratios for network effect on any chest finding varied between 0.37 (95% CI = [0.19, 0.71]) (the Mataro Network) and 4.46 (95% CI = [2.55, 7.82]) (the Bratislava Network). The network differences in predictive value were most pronounced for ‘diminished vesicular breathing,’ from OR = 0.09 (95% CI = [0.01, 0.63]) (the Barcelona Network) to OR = 15.90 (95% CI = [7.54, 33.55]) (the Bratislava network) ().
Table 3. Association between network and patient factors with the recording of auscultation abnormalitiesa.
Patient characteristics that most strongly predicted ‘any auscultation abnormality’ in the multivariable analyses, were respiratory comorbidity (OR = 2.60, 95% CI = [1.89,3.57]) and current smoking (OR = 1.85, 95% CI = [1.42,2.42]), whereas the strongest predictors among the symptoms were (self-reported) wheezing (OR = 3.23, 95% CI = [2.55,4.11]), shortness of breath (OR = 2.02, 95% CI = [1.58,2.59]), and phlegm production (OR = 1.83, 95% CI = [1.40, 2.40]) ().
DISCUSSION
Main findings
In this international observational study of the presentation, management and outcome of adults presenting with acute cough in general practice, wide variation was found between primary care research networks in 12 European countries in the recording of diminished vesicular breathing, wheezes, crackles and rhonchi. It was shown that network (location) remained a significant predictor of clinician's recording of auscultation abnormality after controlling for patient characteristics.
strengths
This large multinational observational study provided an ideal opportunity to describe the recording of auscultation abnormalities by GPs in patients presenting with acute cough in situations of pragmatic clinical care. As far as we are aware, it is the first international observational study of the recording of lung auscultation abnormalities to be conducted in primary care. The observational nature of the study helped ensure that these patients were representative of patients presenting in primary care, and we were able to control for patient characteristics and symptoms in our analyses.
Restricting clinicians’ options to four categories of abnormality on the CRF is a potential limitation of this study. Providing a greater range of options might have allowed us to draw further conclusions about the frequency with which a greater range of terms are used.
Problems with translation of the auscultation abnormality terms may have contributed to some of the variation in use found in this study. Translation is an inevitable challenge in any multinational study describing the use of terminology. A process of translation and back translation was used to assess the accuracy of translation and this process identified errors in the Balatonfüred (Hungary) network, and patients from this network were subsequently removed from the analysis. No such errors were identified in the translation of study materials in other networks. However, we cannot be certain that translation issues did not contribute to variations in the interpretation of the auscultation abnormality terms used in different networks. A list of the auscultation abnormality terms used can be found in .
Previous studies on the reliability of lung sound recordings have been based on clinicians examining the same patients or recordings of the same sounds (Citation23). We have no objective data on what lung sounds were actually present (for example, audio recordings or time expanded waveforms), and only one examiner examined each study participant. We are, therefore, unable to comment on the accuracy of assessments or inter-rater reliability. However, the purpose of this study was to explore variation in the use of terms for auscultation abnormalities by clinicians in everyday clinical practice, not to draw conclusions about the accuracy of their assessments.
Interpretation of the study findings in relation to existing literature
Variation in the frequency with which auscultation abnormality terms were recorded between different networks may reflect both different thresholds for reacting to uncertain auscultation abnormalities, and different labelling of the sounds heard. How GPs instruct patients about the depth and the speed of respiration during auscultation is also important, because the loudness of the breath sounds is highly correlated with airflow in the bronchial tree, and inspiration from residual volume rather than tidal volume can yield abnormal auscultation abnormalities in up to half of normal subjects (Citation24,Citation25).
In 1997, groups linked to the International Lung Sounds Association (ILSA) presented new definitions based on computerized respiratory sound analysis (Citation26). They included the terms wheeze (‘a continuous sound having a musical character’), crackles (‘discontinuous, explosive sound occurring usually during inspiration’) and rhonchi (‘low-pitched wheeze containing rapidly damping periodic waveforms’) as recommended terms for adventitious lung sounds. However, differences in interpretation persist. Previous studies have found that the term “rhonchi” is used with less precision than other terms (Citation27,Citation28). When 277 North American physicians described eight different sound samples, the term ‘rhonchi’ was used to describe coarse crackles and pleural friction rub, as well as true rhonchi. More than half the respondents labelled the expiratory rhonchus inaccurately, and some sounds were labelled as ‘crackles’, ‘rales’ and ‘rhonchi’ with similar frequency. Although defined as low-pitched continuous sounds, rhonchi often have an uneven and noisy (rather than musical) quality, which makes confusion with crackles more likely. ‘Wheeze’ and ‘rhonchi’ were also, but to a lesser degree, used for the same sounds in Wilkins’ study. When the quality of rhonchi is musical, distinction from wheezes may be perceived as arbitrary, and it has been suggested that term wheezes is used for both sounds (Citation10).
That pulmonary comorbidity and current smoking were independent predictors of ‘any auscultation abnormality’ was not surprising. Abnormal lung sounds are well known features of obstructive lung diseases (Citation26). The symptoms of wheezing, shortness of breath, and phlegm production were also independent predictors of abnormal lung sounds. They are all commonly found in lung disorders (Citation29).
Implications for research and clinical practice
Chest auscultation continues to be part of a thorough clinical assessment, which is an important component of providing patients with reassurance and can help in the diagnosis of community acquired pneumonia (Citation30,Citation31). However, auscultation abnormalities seem to be interpreted differently between clinicians and countries, and the results of this study call into question the results of studies evaluating their diagnostic and prognostic value in primary care settings. Therefore, two interdependent challenges have to be addressed: obtaining valid knowledge about the predictive value of lung sounds in diagnosis and prognosis, and ensuring reliability in the assessment and labelling of lung sounds.
There is some evidence that the teaching of auscultation skills could be improved. Pulmonary auscultation skills was taught by only 10% of American family medicine programmes in the early 1990s, and there was no significant increase in this by the late 1990s (Citation32). In addition, trainee doctors have been shown to identify correctly less than half of respiratory sounds, performing no better than medical students (Citation33). Digital technology to visualize the waveform and spectrum of lung sounds may be helpful in this quality improvement. Interactive web-based training may be the most cost-effective and efficient method of providing relevant training. However, training and assessment in clinical skills needs to emphasize competence in the complete examination of the chest, including inspection, palpation and percussion, as auscultation should not be used in isolation. Application of electronic stethoscopes may aid in the detection of auscultation abnormalities using amplification and filtering, and can allow for the recording of lung sounds, which enables clinicians to share auscultation experiences.
There is also a need for further standardization of the nomenclature and classification of lung auscultation abnormalities. Agreement on terminology describing the most common sounds should be a first priority. A simplification of the current system of terms may be needed, if the consistency of auscultation abnormality detection cannot be improved with further training. The great variation found in the use of the term rhonchi suggests a redefinition may be beneficial.
Conclusion
There is wide variation across Europe in clinicians’ use of terms to describe auscultation abnormalities in patients presenting with acute cough. This variation cannot be explained by variation in case mix and, therefore, is likely to be due to inconsistency in use of these terms. Greater uniformity in the use of the terms for abnormal clinical findings will support efforts to improve common standards of clinical diagnosis internationally. Conduct and interpretation of research on respiratory illness and the development and implementation of clinical algorithms and guidelines are also likely to be enhanced.
ACKNOWLEDGEMENTS
The authors should like to thank all patients, clinicians, and networks that participated in the GRACE-01 study. The authors acknowledge the entire GRACE team for their expertise, hard work, and enthusiasm. The GRACE study was funded by the 6th Framework Programme of the European Commission.
Funding
This work was supported by the 6th Framework Programme of the European Commission (reference: LSHM–CT–2005–518226) and the South East Wales Trials Unit is funded by the Wales Office for Research and Development. The Antwerp Primary Care Network was supported by the Research Foundation—Flanders (G.0274.08N).
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Laënnec RTH. De l'auscultation médiate ou traité du diagnostic des maladies des poumons et du coeur (on mediate auscultation or treatise on the diagnosis of the diseases of the lungs and heart). Paris: Brosson & Chaudé; 1819.
- Metlay JP, Fine MJ. Testing strategies in the initial management of patients with community-acquired pneumonia. Ann Intern Med. 2003;138:109–18.
- Melbye H, Straume B, Aasebø U, Dale K. Diagnosis of pneumonia in adults in general practice. Relative importance of typical symptoms and abnormal chest signs evaluated against a radiographic reference standard. Scand J Prim Health Care 1992;10:226–33.
- Hopstaken RM, Stobberingh EE, Knottnerus JA, Muris JW, Nelemans P, Rinkens PE, et al. Clinical items not helpful in differentiating viral from bacterial lower respiratory tract infections in general practice. J Clin Epidemiol. 2005;58:175–83.
- Hopstaken RM, Coenen S, Butler CC, Nelemans P, Muris JW, Rinkens PE, et al. Prognostic factors and clinical outcome in acute lower respiratory tract infections: A prospective study in general practice. Fam Pract. 2006;23:512–9.
- Macfarlane J, Lewis SA, Macfarlane R, Holmes W. Contemporary use of antibiotics in 1089 adults presenting with acute lower respiratory tract illness in general practice in the UK: Implications for developing management guidelines. Respir Med. 1997;91:427–34.
- Hopstaken RM, Butler CC, Muris JW, Knottnerus JA, Kester AD, Rinkens PE, et al. Do clinical findings in lower respiratory tract infection help general practitioners prescribe antibiotics appropriately? An observational cohort study in general practice. Fam Pract. 2006;23:180–7.
- Coenen S, Michiels B, Van Royen P, Van der Auwera JC, Denekens J. Antibiotics for coughing in general practice: a questionnaire study to quantify and condense the reasons for prescribing. BMC Fam Pract. 2002;3:16.
- Coenen S, Michiels B, Renard D, Denekens J, Van Royen P. Antibiotic prescribing for acute cough: the effect of perceived patient demand. Br J Gen Pract. 2006;56:183–90.
- Robertson AJ, Coope R. Rales, rhonchi, and Laënnec. Lancet 1957;270:417–23.
- Pulmonary terms and symbols. A report of the ACCP-STS Joint Committee on Pulmonary Nomenclature. Chest 1975;67:583–93.
- American Thoracic Society Committee on Pulmonary Nomenclature. Pulmonary Nomenclature. American Thoracic Society News. 1977;3:6.
- Mikami R, Murao M, Cugell DW, Chretien J, Cole P, Meier-Sydow J, et al. International symposium on lung sounds. Synopsis of proceedings. Chest 1987;92:342–5.
- Butler CC, Hood K, Verheij TJ, Little P, Melbye H, Nuttall J, et al. Variation in antibiotic prescribing and its impact on recovery in patients with acute cough in primary care: Prospective study in 13 countries. Br Med J. 2009;338:b2242.
- Butler CC, Hood K, Kelly MJ, Goossens H, Verheij T, Little P, et al. Treatment of acute cough/lower respiratory tract infection by antibiotic class and associated outcomes: A 13 European country observational study in primary care. J Antimicrob Chemother. 2010;65:2472–8.
- Butler CC, Kelly MJ, Hood K, Schaberg T, Melbye H, Serra-Prat M, et al. Antibiotic prescribing for discoloured sputum in acute cough/LRTI. Eur Respir J. 2011;38:119–25.
- Stanton N, Hood K, Kelly MJ, Nuttall J, Gillespie D, Verheij T, et al. Are smokers with acute cough in primary care prescribed antibiotics more often, and to what benefit? An observational study in 13 European countries. Eur Respir J. 2010;35:761–7.
- Jakobsen KA, Melbye H, Kelly MJ, Ceynowa C, Molstad S, Hood K, et al. Influence of CRP testing and clinical findings on antibiotic prescribing in adults presenting with acute cough in primary care. Scand J Prim Health Care 2010;28:229–36.
- Wood J, Butler CC, Hood K, Kelly MJ, Verheij T, Little P, et al. Antibiotic prescribing for adults with acute cough/lower respiratory tract infection: Congruence with guidelines. Eur Respir J. 2011;38:112–8.
- Francis NA, Cals JW, Butler CC, Hood K, Verheij T, Little P, et al. Severity assessment for lower respiratory tract infections: Potential use and validity of the CRB-65 in primary care. Prim Care Respir J. 2012;21:65–70.
- Francis NA, Gillespie D, Nuttall J, Hood K, Little P, Verheij T, et al. Antibiotics for acute cough: An international observational study of patient adherence in primary care. Br J Gen Pract. 2012;62:e429–37.
- Francis NA, Gillespie D, Nuttall J, Hood K, Little P, Verheij T, et al. Delayed antibiotic prescribing and associated antibiotic consumption in adults with acute cough. Br J Gen Pract. 2012;62:e639–e46.
- Benbassat J, Baumal R. Narrative review: Should teaching of the respiratory physical examination be restricted only to signs with proven reliability and validity? J Gen Intern Med. 2010;25:865–72.
- Thacker RE, Kraman SS. The prevalence of auscultatory crackles in subjects without lung disease. Chest 1982;81:672–4.
- Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. J Am Med Assoc. 1997;278:1440–5.
- Pasterkamp H, Kraman SS, Wodicka GR. Respiratory sounds. Advances beyond the stethoscope. Am J Respir Crit Care Med. 1997;156:974–87.
- Wilkins RL, Dexter JR, Murphy RL, DelBono EA. Lung sound nomenclature survey. Chest 1990;98:886–9.
- Wipf JE, Lipsky BA, Hirschmann JV, Boyko EJ, Takasugi J, Peugeot RL, et al. Diagnosing pneumonia by physical examination: relevant or relic? Arch Intern Med. 1999;159:1082–7.
- Medbø A, Melbye H. What role may symptoms play in the diagnosis of airflow limitation? A study in an elderly population. Scand J Prim Health Care 2008;26:92–8.
- Greene G, Hood K, Little P, Verheij T, Goossens H, Coenen S, et al. Towards clinical definitions of lower respiratory tract infection (LRTI) for research and primary care practice in Europe: An international consensus study. Prim Care Respir J. 2011;20:299–306.
- Cals JW, Francis NA. Acute cough in adults. Br Med J. 2010;340:c574.
- Mangione S. The teaching of chest auscultation during primary care training: Has anything changed in the 1990s? Chest 2003;124:1430–6.
- Mangione S, Nieman LZ. Pulmonary auscultatory skills during training in internal medicine and family practice. Am J Respir Crit Care Med. 1999;159:1119–24.