Abstract
Background: Many interventions aimed at improving the quality of antibiotic prescribing have been investigated, but more knowledge is needed regarding the impact of different intensity interventions.
Objectives: To compare the effect of two interventions, a basic intervention (BI) and intensive intervention (II), aimed to improve the adherence to recommendations on first-line antibiotics in patients with respiratory tract infections (RTIs).
Methods: General practitioners (GPs) from different regions of Spain were offered two different interventions on antibiotic prescribing. They registered all patients with RTIs during 15 days before (2008) and after (2009) the intervention. GPs in Catalonia were exposed to BI including prescriber feedback, clinical guidelines and training sessions focused on appropriate antibiotic prescribing. The other group of GPs was exposed to an II, which besides BI, also included training and access to point-of-care tests in practice.
Results: The GPs registered 15 073 RTIs before the intervention and 12 760 RTIs after. The antibiotic prescribing rate reduced from 27.7% to 19.8%. Prescribing of first-choice antibiotics increased after the intervention in both groups. In the group of GPs following the BI, first-line antibiotics accounted for 23.8% of antibiotics before the intervention and 29.4% after (increase 5.6%, 95% confidence interval (CI): 1.2–10%), while in the group of GPs following the II these figures were 26.2% and 48.6% (increase 22.4%, 95% CI: 18.8–26%), respectively.
Conclusion: Multifaceted interventions targeting GPs can improve adherence to recommendations for first-line antibiotic prescribing in patients with RTI, with intensive interventions that include point-of-care testing being more effective.
The more intensive an intervention aimed at improving the prescription of first-line antibiotics for respiratory tract infections is, the more effective it is.
INTRODUCTION
Overuse of antibiotics, in general, has contributed to the development of antimicrobial resistance (Citation1). Non-indicated use of antibiotics is further related to unnecessary exposure to adverse effects, increased costs and patient re-consultations (Citation2,Citation3). The vast majority of antibiotics are used by outpatients, mainly for respiratory tract infections (RTIs). For improving antibiotic use, general practitioners (GPs) are the main target for intervention. Many guidelines have been published for GPs on the appropriate treatment of RTIs. However, implementing guidelines into daily clinical practice is hampered by factors that include educational, administrative, personal, economic, and patient behaviour (Citation4–6).
Several strategies have been developed to improve drug use in the community with controversial results (Citation7–9). In general, interventions based on multiple initiatives have been found to be more effective than those focusing on only one initiative. According to a Cochrane review, interventions aimed at reducing overall antibiotic prescribing are less effective than those aimed at increasing the use of first-choice antibiotics (Citation7). However, other reviews have reported the opposite (Citation8). In general, multifaceted interventions have been associated with an average increased prescribing of first-choice antibiotics of approximately 10% (Citation8,Citation9). During the last decades, the use of broad-spectrum antibiotics has considerably increased in many countries, with amoxicillin-clavulanate and amoxicillin as the antibiotics most frequently prescribed by GPs in Spain (Citation10,Citation11). In the United States, Steinman et al., found that broad-spectrum antibiotics were prescribed in more than half of all cases of acute RTIs in adults, and that prescribing of these agents varied widely among GPs (Citation12). There is great concern due to the increased use of broad-spectrum antibiotics and the accompanied increase in the rate of antimicrobial resistance (Citation13,Citation14). Thus, quality indicators have been developed to limit the use of second-line and alternative antibiotic treatments (Citation15).
The Happy Audit project, an acronym for Health Alliance for Prudent Prescribing, Yield and Use of Antimicrobial Drugs in the Treatment of respiratory tract infections, was a study financed by the European Commission. The main objective was to strengthen the surveillance of RTIs in primary health care through the development of intervention programmes targeting GPs and changing people's habits towards prudent use of antimicrobial agents (Citation16). The study involved GPs and patients from six countries (Denmark, Sweden, Lithuania, Russia, Spain and Argentina). In the present study, focus was on the Happy Audit results from Spain, one of the highest antibiotic consuming countries in Europe. The Spanish GPs were allocated to two different interventions to investigate the adherence to recommendations for first-line antibiotics in patients with RTI. One group of GPs followed a basic intervention focusing on prescriber feedback to the GPs, guidelines for antibiotic prescribing and training courses. Another group followed a more intensive intervention consisting of the basic intervention plus training courses in point-of-care tests (Strep A and C-reactive protein) and access to point-of-care tests in practice. The objective of the study was to compare the effect of these two interventions on the adherence to recommendations for first-line antibiotic prescribing in patients with RTIs.
MATERIAL AND METHODS
Study design
GPs from different autonomous regions in Spain were included and exposed to two different interventions. For details about material and methods, we refer to the protocol published in BMC Family medicine (Citation16). Briefly, the GPs registered all contacts due to symptoms of RTIs during 15 days in January and February 2008 (pre- intervention) by filling out a template containing the following variables: age, sex, days of symptoms before encounter, signs and symptoms, suspected aetiology, assumed diagnosis, prescribed antibiotic, potential allergy to penicillin, antibiotic prescribed, GP's perception of patients’ demand for antibiotics, and potential referral to hospital. For both intervention groups, all the participating GPs received individual prescriber feedback based on their own registrations. All GPs participated in training courses focusing on appropriate antibiotic prescribing and they received guidelines for diagnosis and treatment of RTIs, posters for waiting rooms and patient information brochures. GPs allocated to the intensive intervention group were also invited to participate in workshops on point-of-care testing – rapid antigen detection tests for group A β-haemolytic streptococcus antigen and C-reactive protein rapid test – and they were provided access to both point-of-care tests in the consultation. GPs from Catalonia were offered the basic intervention (basic intervention group) as described above, while GPs from the rest of Spain were offered the intensive intervention (intensive intervention group), including access to point-of-care test in practice.
Guidelines on RTIs were based on the current evidence of best quality of antibiotic prescribing in patients with RTIs (). Training courses included a quiz on antibiotic use at the start of the session, a presentation by one of the local GP opinion leaders in infectious diseases, and an interactive group discussion based on several relevant cases from general practice. The two principal messages given were to avoid the use of antibiotics for suspected viral respiratory infections, such as the common cold, influenza, and acute bronchitis (Citation17–20); and, when the decision on antibiotic prescribing was taken, to choose the recommended first-line antibiotic according to the Happy Audit guidelines. Penicillin V was recommended as first-choice antibiotic for treatment of suspected streptococcal pharyngotonsillitis and amoxicillin was recommended for treatment of lower RTIs suspected to be caused by pneumococcal infections in patients otherwise not allergic to β-lactams (Citation21–23). Amoxicillin-clavulanate was only considered as first-choice antibiotic in patients with acute exacerbations of chronic bronchitis or chronic obstructive pulmonary disease and in patients over 65 years with pneumonia (Citation24,Citation25).
Table 1. Antibiotics recommended in different respiratory tract infections.
Outcomes
The primary outcome measure was the proportion of patients with RTIs treated with first-line antibiotics before and after the two different interventions. Secondary outcome measures were the proportion and the pattern of antibiotic prescribing for different RTIs before and after the intervention.
RESULTS
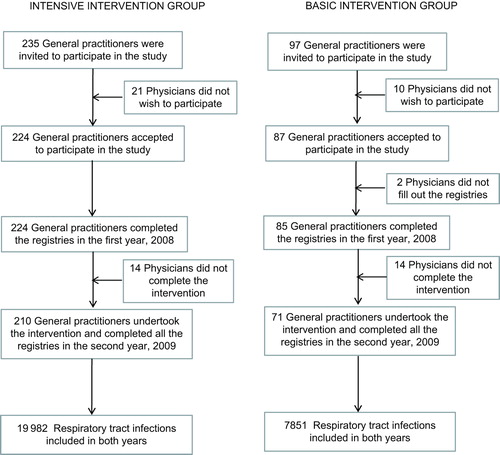
Out of a total of 309 primary care physicians who performed the first registry in 2008, 281 completed the intervention and the second registry (90.9%), of which 210 were assigned to the basic intervention group and 71 to the intensive intervention group (). A total of 11 686 patients were male, being slightly greater in the basic intervention group (45.1% before the intervention and 44.7% after versus 40.9% in the intensive intervention group before and 40.7% after). The mean age of the whole population was 44.8 years, being slightly greater in the intensive intervention group (46 before and 45.5 after) than in the basic intervention group (43.1 before and 42.5 after). The mean number of days with prior symptoms was also greater in the intensive intervention group (4.3 days before the intervention and 4.4 after) than in the basic intervention group (3.7 days before and 3.8 days after). GPs registered a total of 15 073 RTIs before the intervention (2008) and 12 760 after the intervention (2009). The infections most commonly reported were common cold (11 190 cases, 40.2%), followed by pharyngotonsillitis (6105 cases, 21.9%) and acute bronchitis (3286 cases, 11.8%). A total of 474 patients presented allergy to β-lactams (1.7%).
The antibiotic prescribing rate for all patients and both groups of GPs included reduced from 27.7% (95% CI: 27.0–28.4%) before the intervention to 19.8% (95% CI: 19.1–20.5%) after the intervention, a reduction of 7.9% (95% CI: 6.9–8.9%) (). This reduction was greater among GPs assigned to intensive intervention than among clinicians assigned to basic intervention (10.9% versus 0.5%). The type of antibiotic most commonly prescribed was amoxicillin-clavulanate, accounting for 35.8% of all the antibiotics prescribed, followed by amoxicillin (28.8%) (). Amoxicillin-clavulanate was the most frequently used antibiotic in both groups of GPs before the intervention, but after the intervention amoxicillin was the preferred antibiotic (34.7%) among GPs belonging to the basic intervention group. The choice of narrow spectrum penicillin (penicillin V) increased significantly after the intervention in both groups, but the highest increase was found among GPs assigned to the intensive intervention (from 5.3% in 2008 to 16.4% in 2009) ().
Table 2. Number and type of antibiotics prescribed by the 281 GPs who completed both registries, before and after the intervention.
Table 3. Type of antibiotics prescribed by the GPs participating related to the intensity of the intervention.
An improvement in the adherence to recommendations for appropriate antibiotic prescribing of RTIs was observed in both groups of GPs. As shown in , prescribing of first-choice antibiotics increased among GPs in the basic intervention group from 23.8% to 29.4%, (increase 5.6%; 95% CI: 1.2–10%) and in the intensive intervention group from 26.2% to 48.6%, (increase 22.4%; 95% CI: 18.8–26%). shows the antibiotic prescribing rates and percentage of first-line antibiotics for different types of RTIs before and after intervention. The highest increase in first-line antibiotic prescribing was found in patients with pharyngotonsillitis, and mainly in the group of GPs exposed to intensive intervention. In the group of GPs allocated to intensive intervention, the percentage of patients treated with the recommended antibiotic (penicillin V) increased from 16.3% (95% CI: 14–18.7%) before to 53.5% (95% CI: 48.9–58.2%) after the intervention. In the group of GPs exposed to basic intervention amoxicillin and amoxicillin-clavulanate were the dominating antibiotics used (prescribing rate 22% and 9.1%, respectively) and in the group of GPs exposed to intensive intervention penicillin V was the preferred antibiotic (prescribing rate 11.1%). The choice of first-line antibiotics also improved after the intervention in patients with acute otitis and acute sinusitis, but no significant difference was found between the two groups of intervention (). For patients with assumed pneumonia, GPs exposed to intensive intervention had a slightly higher adherence to recommendations of first-line antibiotics compared to GPs exposed to basic intervention. The intervention had a significant impact on the pattern on antibiotics prescribed in patients with suspected pneumonia. Macrolides were the most frequently used antibiotics among GPs exposed to basic intervention, accounting for 27.6% of all antibiotics. However, in the group of GPs exposed to intensive intervention amoxicillin-clavulanate was the most prescribed antibiotic, with 36.9% of the cases and macrolides were only used in 8.1% patients in patients with suspected pneumonia.
Table 4. Percentage of prescription of first-line antibiotics to patients not allergic to β-lactams with different respiratory tract infections before and after intervention (basic and intensive intervention).
DISCUSSION
Main findings
This pragmatic study in primary care showed that a multifaceted intervention targeting GPs can improve adherence to recommendations for first-line antibiotic prescribing in patients with RTI. Intensive interventions that included point-of-care testing were more effective than basic interventions only focusing on prescriber feedback, guidelines and training sessions.
Strengths and limitations
This study has some limitations. First, this was a study in which GPs participated voluntarily and probably their prescribing habits were not representative for all GPs in Spain, and this may have jeopardized the generalizability of the results. It is possible that the participating GPs were more prone to interventions aimed at behaviour change than their colleagues who did not participate. The associated comorbidity of the patients registered was not taken into account, which might have influenced the percentage and the type of antibiotic used. Another limitation of the study was that the clinical outcomes of the different interventions were not taken into account and thus, data regarding whether the percentage of complications or clinical failure differed between groups was lacking. Although health outcomes were not measured, the registry sheet included the referral of patients to hospital. This was not a clinical trial, since GPs were not randomly assigned to the different levels of intervention, constituting another weakness of this study. However, the greatest strength of this study was the large number of physicians included. In addition, less than 10% of the professionals who carried out the first registry abandoned. Another strength of the study was the involvement of lead GPs who were experts and opinion leaders in infectious diseases. Leadership by local health professionals was crucial for coordinating the medical education in this study and supplying credible and high-quality educational materials was essential to ensure that the main messages of the guidelines were accepted as valid and relevant.
Comparison with other studies
According to a Cochrane Review, audit and feedback is defined as a summary of health care performance over a specified period with or without recommendations for clinical action. Evidence from 140 randomized controlled trials indicated that audit and feedback resulted in a modest improvement in care (Citation26). Grimshaw et al., undertook a comprehensive review of the effects of using different strategies for implementing guidelines and found that audit and feedback alone or combined with educational meetings and materials resulted in a modest improvement in the implementation of guidelines in comparison to a non-intervention group (Citation5). Furthermore, studies assessing the effectiveness of printed educational materials indicated only a small impact on practice, but there was no reliable assessment of the cost effectiveness of such programmes (Citation27). In general, multifaceted interventions are more frequently effective than those using only one intervention (Citation7–9,Citation28–30). The level of change in antibiotic prescribing seen in this study is comparable to that described in other studies, which have attempted to modify prescribing for RTIs via interventions targeting health care professionals. In a Norwegian cluster randomized controlled study published recently, an intervention consisting of the presentation of clinical guidelines for antibiotic use and feedback reports on each GP's antibiotic prescribing profile showed a reduction in the prescription of non-penicillin V antibiotics (Citation31). In another study, physicians assigned to an intervention programme were 29% less likely to prescribe second-line antibiotics (Citation32). In a rural area in the United States, Rubin et al., observed a drastic reduction in the prescription of macrolides after a multifaceted intervention including repetitive use of printed diagnostic and treatment algorithms (Citation30). In this study, the reduction of macrolides after the intervention was also crucial and was greater than the reduction of β-lactams.
Conclusion
Changing prescriber behaviour is challenging and may require complex multilayered interventions. This study shows that a multifaceted intervention including audit and prescriber feedback, discussion of the results, dissemination of printed educational materials, meetings on RTI guidelines, and information brochures for patients, led to a slight increase of the percentage of first-line antibiotics and a reduction of otherwise broad-spectrum second-line antibacterials. However, the assignment of GPs to a more intense intervention, with the participation in workshops on point-of-care tests and the provision of these tests in the consultation, led to higher adherence to recommendations for first-choice antibiotics. Hence, it is important to identify interventions that are easy to implement to improve physician prescribing habits.
ACKNOWLEDGEMENTS
The authors should like to acknowledge the particular contribution of Carolina Pérez, Juan de Dios Alcántara, Manuel Gómez, Marina Cid, Gloria Guerra, Jesús Ortega, María Luisa Cigüenza, Vicenta Pineda, José Paredes, Juan Luis Burgazzoli, Silvia Hernández and Anders Munck and all physicians who have participated in the Happy Audit study.
FUNDING
This project is a Specific Targeted Research Project (STREP) funded by The European Commission: DG SANCO under the Programme Framework 6 (SP5A–CT–2007–044154). Contract Number 044154.
Declaration of interest: CL reports having a grant from the Fundació Jordi Gol i Gurina for a research stage at the University of Cardiff. He also reports receiving research grants from the European Commission (Sixth and Seventh Programme Framework), Catalan Society of Family Medicine, and Instituto de Salud Carlos III (Spanish Ministry of Health). The other authors do not have any conflict of interest.
REFERENCES
- Goossens H, Ferech M, van der Stichele R, Elseviers M; ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance: A cross-national database study. Lancet 2005;365:579–87.
- Barlett JG. Antibiotic-associated diarrhoea. N Engl J Med. 2002; 346:334–9.
- Moore M, Little P, Rumsby K, Kelly J, Watson L, Warner G, et al. Effect of antibiotic prescribing strategies and an information leaflet on longer-term reconsultation for acute lower respiratory tract infection. Br J Gen Pract. 2009;59:728–34.
- Wensing M, van der Weijden T, Grol R. Implementing guidelines and innovations in general practice: Which interventions are effective? Br J Gen Pract. 1998;48:991–7.
- Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8:1–72.
- Grol R, Grimshaw J. From best evidence to best practice: Effective implementation of change in patients’ care. Lancet 2003;362:1225–30.
- Arnold SR, Straus SE. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev 2005;4: CD003539.
- van der Velden AW, Pijpers EJ, Kuyvenhoven MM, Tonkin-Crine SK, Little P, Verheij TJ. Effectiveness of physician-targeted interventions to improve antibiotic use for respiratory tract infections. Br J Gen Pract. 2012;62:e801–7.
- Steinman MA, Ranji SR, Shojania KG, Gonzales R. Improving antibiotic selection: A systematic review and quantitative analysis of quality improvement strategies. Med Care 2006; 44:617–28.
- Llor C, Cots JM, Gaspar MJ, Alay M, Rams N. Antibiotic prescribing over the last 16 years: Fewer antibiotics but the spectrum is broadening. Eur J Clin Microbiol Infect Dis. 2009;28:893–7.
- Ministerio de Sanidad, Política Social e Igualdad y Agencia Española de Medicamentos y Productos Sanitarios. Uso de Antibióticos en España, 2010.
- Steinman MA, Landefeld CS, Gonzales R. Predictors of broad-spectrum antibiotic prescribing for acute respiratory tract infections in adult primary care. J Am Med Assoc. 2003; 289:719–25.
- Bronzwaer SL, Cars O, Buchholz U, Mölstad S, Goettsch W, Veldhuijzen IK, et al: European Antimicrobial Resistance Surveillance System. A European study on the relationship between antimicrobial use and antimicrobial resistance. Emerg Infect Dis. 2002;8:278–82.
- Laxminarayan R, Duse A, Wattal C, Zaidi AK, Wertheim HF, Sumpradit N, et al. Antibiotic resistance – the need for global solutions. Lancet Infect Dis. 2013;13:1057–98.
- Hansen MP, Bjerrum L, Gahrn-Hansen B, Christensen R, Davidsen JR, Munck A, et al. Quality indicators for treatment or respiratory tract infections? An assessment by Danish general practitioners. Eur J Gen Pract. 2013;19:85–91.
- Bjerrum L, Munck A, Gahrn-Hansen B, Hansen MP, Jarboel D, Llor C, et al. Health alliance for prudent prescribing, yield and use of antimicrobial drugs in the treatment of respiratory tract infections (HAPPY AUDIT). BMC Fam Pract. 2010;11:29.
- Kenealy T, Arroll B. Antibiotics for the common cold and acute purulent rhinitis. Cochrane Database Syst Rev 2013; 6: CD000247.
- Carrat F, Schwarzinger M, Housset B, Valleron AJ. Antibiotic treatment for influenza does not affect resolution of illness, secondary visits or lost workdays. Eur J Epidemiol. 2004; 19:703–5.
- Smith SM, Fahey T, Smucny J, Becker LA. Antibiotics for acute bronchitis. Cochrane Database Syst Rev 2014;3: CD000245.
- Llor C, Moragas A, Bayona C, Morros R, Pera H, Plana-Ripoll O, et al. Efficacy of anti-inflammatory or antibiotic treatment in patients with non-complicated acute bronchitis and discoloured sputum: Randomised placebo controlled trial. Br Med J. 2013; 347:f5762.
- van Driel ML, De Sutter AI, Keber N, Habraken H, Christiaens T. Different antibiotic treatments for group A streptococcal pharyngitis. Cochrane Database Syst Rev 2013;4: CD004406.
- Garbutt JM, Banister C, Spitznagel E, Piccirillo JF. Amoxicillin for acute rhinosinusitis: a randomized controlled trial. J Am Med Assoc. 2012;307:685–92.
- Venekamp RP, Sanders S, Glasziou PP, Del Mar CB, Rovers MM. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev 2013;1: CD000219.
- Cots JM, Monedero J, Arranz J, Gómez M, Mórato ML, Sánchez C (editors). Manual de enfermedades infecciosas en Atención Primaria 3ª ed. Barcelona: semFYC Ediciones; 2010.
- Wilson R, Sethi S, Anzueto A, Miravitlles M. Antibiotics for treatment and prevention of exacerbations of chronic obstructive pulmonary disease. J Infect. 2013;67:497–515.
- Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012;6: CD000259.
- Giguère A, Légaré F, Grimshaw J, Turcotte S, Fiander M, Grudniewicz A, et al. Printed educational materials: Effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012;10: CD004398.
- van Driel ML, Coenen S, Dirven K, Lobbestael J, Janssens I, Van Royen P, et al. What is the role of quality circles in strategies to optimise antibiotic prescribing? A pragmatic cluster- randomised controlled trial in primary care. Qual Saf Health Care 2007;16:197–202.
- De Santis G, Harvey KJ, Howard D, Mashford ML, Moulds RF. Improving the quality of antibiotic prescription patterns in general practice. The role of educational intervention. Med J Aust. 1994;160:502–5.
- Rubin MA, Bateman K, Alder S, Donnelly S, Stoddard GJ, Samore MH. A multifaceted intervention to improve antimicrobial prescribing for upper respiratory tract infections in a small rural community. Clin Infect Dis. 2005;40:546–53.
- Gjelstad S, Høye S, Straand J, Brekke M, Dalen I, Lindbæk M. Improving antibiotic prescribing in acute respiratory tract infections: Cluster randomised trial from Norwegian general practice (prescription peer academic detailing (Rx-PAD) study). Br Med J. 2013;347:f4403.
- Stewart J, Pilla J, Dunn L. Pilot study for appropriate anti-infective community therapy. Effect of a guideline-based strategy to optimize use of antibiotics. Can Fam Physician 2000;46:851–9.