ABSTRACT
Background Ankle sprain is frequently encountered, both in primary care and in emergency departments. Since 1992, the Ottawa ankle rules (OAR) can assist clinicians in determining whether an X-ray should be performed to exclude a fracture. Several guidelines recommend the use of OAR based on a systematic review from 2003. Ten years later, one can wonder if this recommendation should be changed.
Objective To review systematically the current evidence on the most accurate method to assess the fracture risk after an ankle sprain in adults.
Methods A methodical search for systematic reviews, meta-analyses and primary studies was carried out in Medline, Cochrane Database of systematic reviews, Embase, Pedro, CINAHL, Medion and specific guideline search engines. At least two independent researchers performed selection, quality appraisal (with validated checklists) and data extraction.
Results One systematic review and 21 primary studies were selected. Sensitivity and specificity of the OAR range from 92–100% and from 16–51%, respectively. To improve the OAR specificity, other tools are proposed such as the Bernese ankle rules. Vibrating tuning fork test and ultrasound could be useful in patient with OAR positive to decrease the need for radiographs. No evidence was found in favour of the use of magnetic resonance imaging (MRI) or computed tomography (CT) in the acute phase of ankle sprain.
Conclusion The findings confirm the value of the OAR at ruling out fractures after an ankle sprain and propose other or additional tools to decrease the need for X-rays.
The Ottawa ankle rules remain of utmost importance in identifying X-ray eligible patients with acute ankle sprains.
The role of the Bernese ankle rules instead of the OAR and the added-value of the tuning fork test and ultrasound in patients with positive OAR are promising but should be confirmed.
KEY MESSAGES
Introduction
Ankle sprains: a frequent problem
Ankle sprains cover lesions of various gravities, from a mild sprain to a complete rupture of one or more ligaments supporting the ankle. The incidence estimates of reported ankle sprains in the general population are scarce. In the nineties, approximately 300 ankle sprains per 10 000 inhabitants per year were reported in the UK, in France and in the Netherlands.[Citation2–4] There is, unfortunately, a lack of data on incidence rates in primary care settings.
A diagnostic based on radiographs
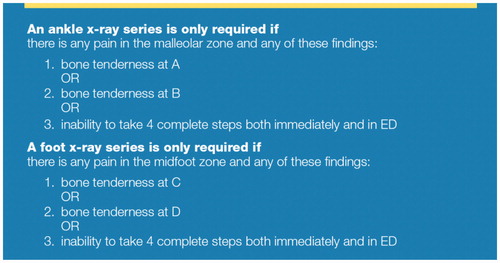
The likelihood of a fracture in an ankle injury varies from 1–4% in general practice to 15% in emergency departments.[Citation5] Despite this relatively low probability, most patients undergo radiography.[Citation1] To decrease the number of unnecessary radiographs, the Ottawa Hospital Research Institute published a set of guidelines ‘The Ottawa ankle rules’ in 1992 to assist physicians in deciding whether radiography is needed after ankle injury.[Citation6]
Since 1992, countries like Belgium, the Netherlands and the United States have included the Ottawa ankle rules in their guidelines.[Citation7–9] All these guidelines based their recommendations on the 2003 systematic review meta-analysis of Bachmann and colleagues.[Citation1]
More than ten years later, one can wonder whether new evidence is available and if the recommendations should be changed. Moreover, several questions have been raised about the utility of other imaging techniques such as ultrasound, magnetic resonance imaging (MRI) or CT-scans.
We conducted a systematic review to answer the following question: what is the most accurate method to assess the fracture risk after an ankle sprain in adults?
Methods
Search strategy
An electronic search for systematic reviews, meta-analyses and primary studies was performed in the Cochrane Database of systematic reviews, Medline, Embase, Pedro search database, CINAHL and Medion. A combination of a set of key terms was used combining three groups of words with ‘OR’ inside the groups and ‘AND’ between the groups:
Pathology: ankle sprain, OR ankle injury, OR ankle trauma;
Field of search (intervention): diagnosis. In Medline, a broad filter was used in order not to miss any articles about the Ottawa ankle rules. In Embase, the search was built on specific Emtree terms.
Type of reference (study design) included: (systematic) reviews, OR meta-analyses, OR guidelines, OR RCT’s, OR diagnostic trials, OR controlled clinical trials.
We also looked for guidelines as sources of systematic reviews and additional studies using the guidelines search engines of G-I-N, NICE, SIGN, National Guideline Clearinghouse, and New Zealand. The electronic search for systematic reviews, meta-analyses and guidelines covered the period from 1 January 2000 to 6 December 2011. The languages were Dutch, English, German and French. More details are available online at https://kce.fgov.be/sites/default/files/page_documents/KCE_197C_2011-02-GCP_Ankle%20sprain_0.pdf
Inclusion and exclusion criteria
To be included papers had to cover acute inversion sprain in adults. Age younger than 16 years, tendinopathy, acute and chronic non-traumatic ankle pain, chronic ankle instability and any other ankle trauma were reasons for exclusion. The inclusion and exclusion criteria according to the PICO framework (population, intervention, comparator, outcome) are available in .
Table 1. Inclusion and exclusion criteria according to the PICO framework (population, intervention, comparator, outcome).
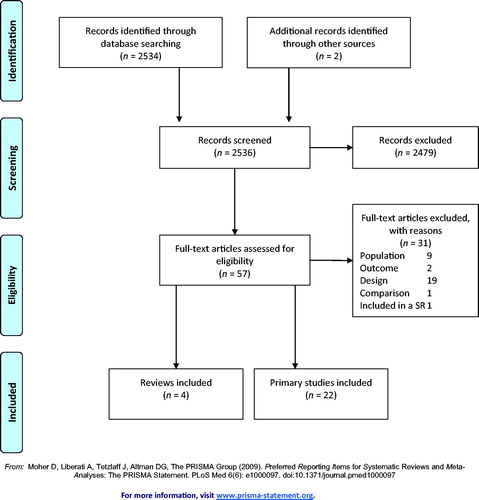
Selection of studies ()
Study selection was conducted by two groups of two researchers (TW & PR and RDR & PR), first on the title and abstract and subsequently on the full-text basis. Manual searching of additional articles was based on the reference lists of all selected studies and guidelines. The search identified 2536 titles from which 57 were retrieved for full text evaluation. Four guidelines were also identified.
Quality appraisal
The quality appraisal was performed by three researchers (TW, RDR, PR) using specific checklists (AMSTAR, Dutch Cochrane tool for assessing risk of bias, QUADAS and AGREE II) and was double-checked by another group of researchers (KH, LS, PJ). In case of disagreement, consensus was achieved through discussion.
Data analysis
Two groups of independent reviewers (TW & PR and RDR & PR) extracted the data, using a standard KCE template for evidence tables. The tables encompassed a description of the study type, its objective, the PICO, the results and the level of evidence.
The analysis followed a hierarchical approach:
Extraction of the data from the systematic reviews and meta-analyses.
Search for the most recent primary studies to update the evidence found in the previous step (randomized and prospective controlled trials).
Results
Four guidelines and 26 publications were selected (four systematic reviews and 22 primary studies.[Citation1,Citation4,Citation7,Citation10–15,Citation36] Among them, three systematic reviews were excluded because of their low quality and one article because it was a summary of a retained guideline.[Citation12–14,Citation20] The final selection contains one systematic review and 21 primary studies.[Citation1,Citation15–19,Citation21–36] A description of these studies is available in and . The paucity of data and their heterogeneity prevented us from conducting a meta-analysis.
Table 2. Description of included systematic review.
Table 3. Description of included primary studies.
Among the 21 primary studies, 16 are from a European country (seven from the Netherlands) and only two are RCTs.
Ottawa ankle rules
Many trials evaluate the validity of the Ottawa ankle rules (OAR) for excluding fractures of the ankle in patients with an ankle sprain:
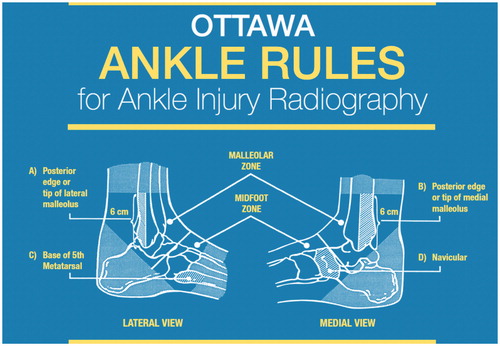
The meta-analysis of Bachmann, with a moderate risk of bias, summarizes the accuracy of the OAR from 1990 to 2002.[Citation1] The authors selected 27 studies describing 15 581 patients. The results show that pooled sensitivities, and the median of non-pooled specificities are 98% (95% CI: 96–99) and 40% (95% CI: 28–48), respectively for the assessment of the ankle.
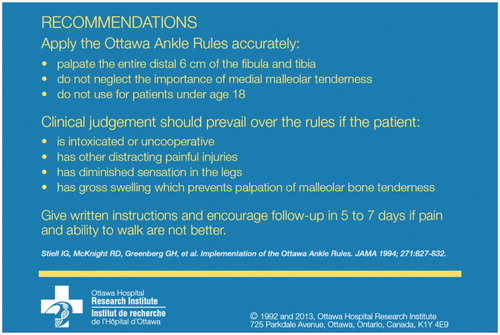
Eight studies published after the meta-analysis assess the validity of the OAR.[Citation17,Citation18,Citation22,Citation25,Citation28,Citation29,Citation33,Citation36] Most of them are prospective studies, with low to moderate risk of bias. Many studies use X-rays as a reference but some also use clinical evaluation.[Citation28,Citation29,Citation36] Clinical heterogeneity is noted between the studies in terms of setting (emergency department and primary care), patient characteristics (sometimes children are included), timing of OAR application (within 48 h to 10 days), type of provider (not only physicians) and characteristics of the test itself (OAR versus Buffalo malleolar rules). As the difference between Buffalo malleolar rule and OAR is minor (a change in the original area of palpation from the posterior borders of the malleoli to the midcrests of the malleoli, away from the ligament attachments), both tests are further considered as one. These studies show sensitivities and specificities of OAR ranging from 92–100% and from 16–51% respectively (). Three studies showed a sensitivity lower than 100%.[Citation22,Citation25,Citation28] In each study, the number of missed fractures were very low, and they were considered of little clinical significance.
A difference in specificity is quoted by some authors between specifically trained and non-trained professionals.[Citation17,Citation28,Citation33]
The aim of the OAR is to avoid unnecessary X-rays; but estimates on the reduction of radiographs vary broadly, ranging from 13% to more than 40%.[Citation17,Citation33,Citation36]
It is difficult to specify the best timing for the OAR in the management of acute ankle sprain because most studies [Citation17,Citation18,Citation22,Citation25,Citation28,Citation29,Citation33,Citation36] consider the application of the OAR within 7–10 days after the ankle injury. One meta-analysis showed higher sensitivities when the OAR were applied within 48 h than later after injury but no recent study confirms this result.[Citation1]
One study compared the patients’ self-assessment when applying the OAR with the evaluation by the clinician and concluded that no evidence promotes this approach.[Citation15]
Table 4. Diagnostic indicators performance of the OAR in identifying fracture.
Rules derived from OAR or additional tests to OAR
Several rules and diagnostic processes have been developed to improve the specificity of the OAR and to assist clinicians in the decisions on whether or not to perform an X-ray. Five studies were identified in recent literature on this topic ().[Citation23,Citation24,Citation26,Citation31,Citation35]
An additional vibrating tuning fork test in patients with positive OAR test may lead to a marked reduction in ankle radiographs. The specificity reached 95% if the tuning fork is applied on the distal fibula shaft compared to 61% on the tip of the lateral malleolus without any reduction in the sensitivity (both 100%).[Citation23]
The Bernese ankle rules (Box 1a) applied instead of the Ottawa ankle rules show a sensitivity of 100% and a specificity of 91% that could lead, if it is confirmed, to a reduction of false positive results and of unnecessary radiographs compared with OAR rules.[Citation24]
The Leiden and the Utrecht ankle rules (Box 1b) appear to have higher specificities and lower sensitivities than the OAR.[Citation26,Citation31,Citation35]
Table 5. Diagnostic indicators performance of different tests in identifying fracture.
Box 1 Detailed explanations concerning certain tests.
The Bernese ankle rules consist of three consecutive steps avoiding palpation on the injured region: indirect fibular stress (10 cm proximally to the fibular tip), direct medial malleolar stress, and compression stress of the mid- and hind foot (talus + calcaneus). Indirect forces are applied to the injured region by the flat of the hand or the whole area of the thumb (medial malleolus) instead of the fingertip.
The Leiden ankle rule uses a score derived from 13 weighted variables ordered in seven rows. It was developed on the basis of published likelihood ratios and personal experience of the investigators. The Utrecht ankle rules consist of 16 variables derived from the Leiden ankle rules and subsequently modified on the basis of the personal preferences of the researchers.
After the first missed fracture, the protocol was changed to scan the posterior edge and 10 cm above each malleoli (instead of 6 cm).
Imaging
This section focuses on the utility of imaging for excluding a fracture in the acute phase of the diagnosis. The diagnostic process needed in the presence of persistent symptoms, several days after an ankle injury, is not considered.
One study assessed whether the use of ultrasonography can detect foot and ankle fractures in patients with positive OAR. The results indicate that if ultrasonography (Box 1c) is employed prior to X-ray in OAR positive patients, the number of radiographs will decrease by approximately 80%. Two other studies focused on the role of ultrasound for evaluating the severity of the ligament tear and were inconclusive for our search question.[Citation19,Citation27,Citation34]
Concerning the magnetic resonance imaging, the two selected studies compared MRI with X-ray in the detection of the severity of the lesion and provided inconclusive results.[Citation16,Citation30] No studies were identified on the role of computed tomography in the assessment of fracture risk after ankle sprain.
Discussion
The present study offers an overview of the current evidence on the evaluation of risk fracture after an ankle sprain, a common reason for an encounter in general practice. To our knowledge, no recent systematic review has been published on this topic despite the high prevalence of this kind of injury and the relatively old references used to develop current guidelines. One recent guideline was published by the Royal Society for Physical Therapy [Citation40] and lead to similar conclusions to those of our review.
Main findings
The high sensitivity of the Ottawa ankle rules, previously underlined by the systematic review of Bachmann,[Citation1] is confirmed by recent studies: when the test is negative, a fracture can always almost be excluded. Only three studies reported sensitivity below 100% and the missed fractures were considered of little clinical significance. Moreover, as the OAR recommends repeating the clinical examination after a few days to ascertain the severity of the ankle sprain, this should allow identification of a missed fracture. The relative low specificity of the OAR remains a problem, leading to unnecessary X-rays. The benefit is poorly demonstrated for other tests as Leiden and Utrecht ankle rules, or needs to be confirmed for the Bernese ankle rules, although the first results are very encouraging. In patients with positive OAR, an additional step could increase the specificity. Two methods are promising but need further confirmation: the tuning fork test applied on the distal fibula shaft, and the ultrasound. There is no evidence to support the use of CT-scan or MRI.
Strengths and limitations
The main strength of this review is the sound methodology followed to identify the best available evidence as well as the tools used for its validation (i.e. GRADE). A limitation of this review is the great heterogeneity between the studies concerning the Ottawa ankle rules preventing the performance of a meta-analysis, even if the main conclusions of the studies are similar. The pragmatic approach chosen to select a good quality systematic review as the starting point of this review and then update the evidence with primary studies published after the systematic review could represent another limitation.
Figure 2. Ottawa ankle rules: Areas of palpation. Source: Ottawa Hospital Research Institute (http://www.ohri.ca/). Reprinted with permission of Ian Stiell of the Ottawa Hospital Research Institute.
Future direction
The paucity of high-quality evidence should lead to further research. The place of the tuning fork test and the ultrasound in addition to the OAR deserves to be assessed according to well design studies. The higher specificity of the Bernese ankle rules than the OAR in the assessment of ankle fracture risk also needs to be confirmed. It is, therefore, a broad domain that requires further exploration.
Research on the reasons why X-rays are still performed so often in spite of the very low probability of a fracture is also necessary. Some medical conditions of patients are known to hamper the applicability of the OAR as neurologic deficits, polytrauma, bone disease, pregnancy. The individual patient’s expression of pain can also influence the OAR performance. For example, a vivid expression of pain could result in higher false positive rates whilst stoicism could lead to higher false negative rates. It is important to take this aspect into account.
Fear of possible medico-legal consequences, insurance issues (e.g. sports accidents) or patient demands seem to be factors that jeopardize the applicability of the Ottawa ankle rules.[Citation5,Citation41] To improve the implementation of OAR in clinical practice, some propositions can be formulated, including leaflets and campaigns on unnecessary use of X-rays after a well-performed examination targeted to patients, or specific training programmes for health professionals. Furthermore, results of the OAR examination could be systematically registered in the patient medical record and a second examination for patients, if pain and walking ability do not improve after several days, should be proposed during the first consultation.
Conclusion
The present study confirms the central role of OAR as a first step towards the diagnosis of ankle sprain since this test allows selection of patients eligible for X-ray. Although a promising alternative test (the Bernese ankle rules) or additional tests (the tuning fork test and the ultrasound) to increase the OAR specificity are available, their added value should be confirmed.
Funding
The Belgian Health Care Knowledge Centre (KCE) is a publicly funded federal scientific research institution; its mission is to provide independent scientific advice. KCE as an institution and all individual KCE collaborators declare that they have no interests in commercial companies, healthcare organizations, professional interest groups or any other body on which the guidelines could have a positive or negative impact (financial or other). Every person having contributed to the elaboration of the Belgian guideline (as an expert, validator or stakeholder) has been requested to declare potentially conflicting interests. This information is published in the colophon pages of this guideline. https://kce.fgov.be/sites/default/files/page_documents/KCE_197C_2011-02-GCP_Ankle%20sprain_0.pdf
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Bachmann LM, Kolb E, Koller MT, et al. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. Br Med J. 2003;326:417–419.
- Bertini N, Bleichner G, Cannamela A, et al. L‘entorse de cheville au service d‘accueil et d‘urgence. Réan Urg. 1995;4:11.
- Hubbard TJ, Hicks-Little CA. Ankle ligament healing after an acute ankle sprain: an evidence-based approach. J Athl Train. 2008;43:523–529.
- Koninklijk Nederlands Genootschap voor Fysiotherapie (KNGF). Richtlijn Acuut lateraal enkelbandletsel. Amersfoort; 2011.
- Chevalier P. Les règles d‘Ottawa pour exclure une fracture de la cheville. Minerva. 2003;2:2.
- Alberta Medical Association. Toward optimized practice. Guidelines for the radiography of the ankle and foot (Ottawa Ankle Rules). Edmonton: Clinical Practice Guidelines Manager; 2007.
- Wyffels P, De Naeyer P, Van Royen P. Enkeldistorsie: aanbeveling voor goede medische praktijkvoering. 2001; Available at: http://www.domusmedica.be/documentatie/richtlijnen/overzicht/enkeldistorsie-horizontaalmenu-379.html (accessed October 2012).
- van der Wees PJ, Lenssen AF, Feijts YAEJ, et al. KNGF-richtlijn Enkelletsel; 2006.
- Bennett D, Daffner R, Weissman B, et al. ACR Appropriateness Criteria® suspected ankle fractures. 2008.
- Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. J Am Assoc. 1993;269:1127–1132.
- Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Am Fam Physician 2001;63:93–104.
- Seah R, Mani-Babu S, Koninklijk Nederlands Genootschap voor F. Managing ankle sprains in primary care: what is best practice? A systematic review of the last 10 years of evidence. Br Med Bull. 2011;97:105–135.
- Simpson P. Use of the Ottawa ankle rule by paramedics in the out-of-hospital setting. JEPHC. 2010;8:7.
- Smith M. Ankle sprain: a literature search. Emergency nurse: the journal of the RCN Accident and Emergency Nursing Association. 2003;11:12–16.
- Blackham JE, Claridge T, Benger JR. Can patients apply the Ottawa ankle rules to themselves? Emerg Med J. 2008;25:750–751.
- Breitenseher MJ, Trattnig S, Kukla C, et al. MRI versus lateral stress radiography in acute lateral ankle ligament injuries. J Comput Assist Tomogr. 1997;21:280–285.
- Broomhead A, Stuart P. Validation of the Ottawa ankle rules in Australia. Emerg Med (Fremantle) 2003;15:126–132.
- Can U, Ruckert R, Held U, et al. Safety and efficiency of the Ottawa ankle rule in a Swiss population with ankle sprains. Swiss Medical Weekly. 2008;138:292–296.
- Canagasabey MD, Callaghan MJ, Carley S. The sonographic Ottawa foot and ankle rules study (the SOFAR study). Emerg Med J. 2011;28:838–840.
- de Bie RA, Hendriks HJM, Lenssen AF, et al. KNGF-richtlijn Acuut enkelletsel. Ned Tijdschr Fysiother. 1998;108:1–23.
- Derksen RJ, Bakker FC, de Lange-de Klerk ES, et al. Specialized emergency nurses treating ankle and foot injuries: a randomized controlled trial. Am J Emerg Med. 2007;25:144–151.
- Derksen RJ, Bakker FC, Geervliet PC, et al. Diagnostic accuracy and reproducibility in the interpretation of Ottawa ankle and foot rules by specialized emergency nurses. Am J Emerg Med. 2005;23:725–729.
- Dissmann PD, Han KH. The tuning fork test—a useful tool for improving specificity in ‘Ottawa positive’ patients after ankle inversion injury. Emerg Med J. 2006;23:788–790.
- Eggli S, Sclabas GM, Zimmermann H, Exadaktylos AK. The Bernese ankle rules: a fast, reliable test after low-energy, supination-type malleolar and midfoot trauma. J Trauma. 2005;59:1268–1271.
- Fiesseler F, Szucs P, Kec R, Richman PB. Can nurses appropriately interpret the Ottawa ankle rule? Am J Emerg Med. 2004;22:145–148.
- Glas AS, Pijnenburg BA, Lijmer JG, et al. Comparison of diagnostic decision rules and structured data collection in assessment of acute ankle injury. CMAJ. 2002;166:727–733.
- Guillodo Y, Riban P, Guennoc X, et al. Usefulness of ultrasonographic detection of talocrural effusion in ankle sprains. J Ultrasound Med. 2007;26:831–836.
- Knudsen R, Vijdea R, Damborg F. Validation of the Ottawa ankle rules in a Danish emergency department. Dan Med Bull. 2010;57:A4142.
- Leddy JJ, Kesari A, Smolinski RJ. Implementation of the Ottawa ankle rule in a university sports medicine center. Med Sci Sports Exerc. 2002;34:57–62.
- Nikken JJ, Oei EHG, Ginai AZ, et al. Acute ankle trauma: value of a short dedicated extremity MR imaging examination in prediction of need for treatment. Radiology 2005;234:134–142.
- Pijnenburg AC, Glas AS, De Roos MA, et al. Radiography in acute ankle injuries: the Ottawa ankle rules versus local diagnostic decision rules. Ann Emerg Med. 2002;39:599–604.
- Spahn G. The ankle meter: an instrument for evaluation of anterior talar drawer in ankle sprain. Knee Surg Sports Traumatol Arthrosc. 2004;12:338–342.
- Springer BA, Arciero RA, Tenuta JJ, Taylor DC. A prospective study of modified Ottawa ankle rules in a military population. Interobserver agreement between physical therapists and orthopaedic surgeons. Am J Sports Med. 2000;28:864–868.
- Van Dijk C, Mol BW, Lim LS, et al. Diagnosis of ligament rupture of the ankle joint. Physical examination, arthrography, stress radiography and sonography compared in 160 patients after inversion trauma. Acta Orthop Scand. 1996;67:566–570.
- van Riet YE, van der Schouw YT, van der Werken C. Fewer X-rays while maintaining quality of clinical care using clinical protocols for physical diagnosis of ankle injuries. Ned Tijdschr Geneeskd. 2000;144:224–228.
- Wynn-Thomas S, Love T, McLeod D, et al. The Ottawa ankle rules for the use of diagnostic X-ray in after-hours medical centres in New Zealand. NZ Med J. 2002;115:U184.
- Vereniging voor Sportgeneeskunde (VSG). Richtlijn Acute inversie trauma van de enkel. Bilthoven; 2010.
- Cook CE, Hegedus EJ. Orthopedic physical examination tests. An evidence based approach. Upper Saddle River (NJ): Pearson Prentice Hall; 2012. Chapter 14, Physical examination tests for the lower leg, ankle, and foot.
- Young CC, Niedfeldt MW, Morris GA, Eerkes KJ. Clinical examination of the foot and ankle. Prim Care 2005;32:105–132.
- Kerkhoffs GM, van den Bekerom M, Elders LAM, et al. Diagnosis, treatment and prevention of ankle sprains: an evidence-based clinical guideline. Br J Sports Med. 2012;46:854–860.
- Vinck I, Paulus D, Van Brabandt H, Ramaekers D. Aspects médico-légaux des recommandations de bonne pratique médicale. Bruxelles: Centre fédéral d‘expertise des soins de santé (KCE) KCE reports 2006;26B. (Réf. D/2006/10.273/06).