The paper by O’Toole et al.,[Citation1] provides a real-world example of the high morbidity among people attending primary care for opioid agonist treatment (OAT). We wish to highlight the accompanying high mortality rate in this population.
OAT has substantially changed the course of the drug use epidemic.[Citation2–4] Although noted to reduce morbidity and mortality of patients attending specialized treatment clinics, limited longitudinal information is available on cohorts of such patients. To explore the mortality rates, we conducted a prospective observational study through the Registrar of Births, Deaths and Marriages in Ireland and the Central Treatment List (CTL), which followed a cohort of patients (n = 98) recruited for a methadone treatment study in 1996. All patients attended specialist services for OAT and were randomly selected from those who did meet clinical criteria for transfer to general practice for continuing care.[Citation5] Research Ethics Committee of the Irish College of General Practitioners approved the study.
At baseline, the cohort was predominantly male (77%), with a mean age of 33 years (SD: 5.7) and a median school-leaving age of 15 years (range: 6–21). The average age of first heroin use was 17 years (SD 3.2), with a mean age of a first injection at 19 (SD: 4.0). Fifty (51%) participants had been in drug treatment on four or more occasions. The cohort had a mean of 5.1 treatments, including detoxification programmes, abstinence-oriented programmes, narcotics anonymous and previously attempted, unsuccessful methadone maintenance programmes. The average time spent in their current methadone programme was 3.3 years (SD: 1.5), mean dose 60.8 mg (SD: 20.2).
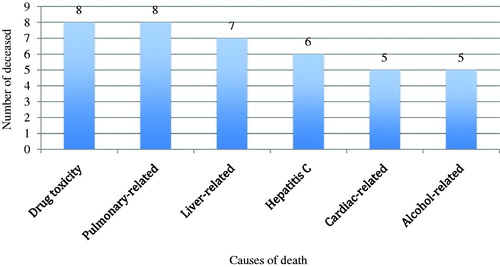
At follow-up in 2013, 27 (27.6%) of the 98 participants had died in Ireland and had relevant entries in the Register of Deaths, 19 (19.4%) were currently in OAT and the status of the remaining 52 (53%) was ‘alive,’ as per the Irish death registry. The 52 patients ‘alive’ had left the (CTL) register, but no further CTL information was available on their status. The death certificates recorded multiple causes for most patients who had died; only six had a single cause. Drug toxicity and/or overdose were the most commonly listed causes of death (see ).
Figure 1. The six most common causes of death in the cohort of people attending opioid agonist treatment who were recruited the study in 1996 (n = 27). Causes are in order of ranking in the overall cohort. The number of deceased within each category does not add up to 27 because most death certificates noted several causes of death.
Our results are biased by the small sample size, non-probabilistic sampling framework, study location and data source and the possibility that some patients may have died outside Ireland. Our inability to establish the interval data for the retention in treatment is a significant study limitation, but the overall retention of 19 out of the surviving 71 patients is comparable to previous research.
Our longitudinal follow-up study documents a minimum mortality rate of 27% in a cohort of relatively young adults followed from 1996 to 2013, demonstrating the much higher mortality rates observed among drug users. As OAT programmes develop, our findings point to an urgent need to improve the structure of addiction treatment to engage more users, reduce the mortality of drug users, and improve their quality of life.
Acknowledgements
The authors wish to thank Deirdre Langton from Coombe Family Practice and staff at the Registry of Deaths and Central Statistics Office for help with data collection. The authors also thank Catherine Anne Field, Davina Swan, Helen Tobin, Leslie Daly, Mairead Egan for their assistance during the initial phases of the project.
Funding
JK’s and GB’s work on this project was supported by the MERIT grant; JK’s and WC’s work was supported by Grant ID: HRA-HSR-2012-14. JK’s time was partly funded by grant ID ELEVATEPD/2014/6. AK was supported by student research stipend, University College Dublin.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- O’Toole J, Hambly R, Cox A-M, O’Shea B, Darker C. Methadone-maintained patients in primary care have higher rates of chronic disease and multimorbidity, and use health services more intensively than matched controls. Eur J Gen Pract. 2014;20; 4:275–280.
- Cullen W, O’Brien S, O’Carroll A, O’Kelly FD, Bury G. Chronic illness and multimorbidity among problem drug users: A comparative cross sectional pilot study in primary care. BMC Fam Pract. 2009;10:25.
- Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Dat Syst Rev. 2014;2:CD002207.
- Bauer SM, Loipl R, Jagsch R, et al. Mortality in opioid-maintained patients after release from an addiction clinic. Eur Addict Res. 2008;14:82–91.
- Langton D, Hickey A, Bury G, Smith M, O’Kelly F, Barry J, et al. Methadone maintenance in general practice: Impact on staff attitudes. Ir J Med Sci. 2000;169:133–136.
