Abstract
Context: Achillea wilhelmsii C. Koch (Asteraceae) is widely used in Iranian traditional medicine.
Objective: This in vivo study evaluates the hepatoprotective role of Iranian A. wilhelmsii oils against acetaminophen-induced oxidative damages in rats.
Materials and methods: The animals were divided into five groups: in negative control and control groups, the DMSO and 500 mg/kg acetaminophen were i.p. injected, respectively. In treatment groups, 100 and 200 mg/kg oils and 10 mg/kg BHT were given i.p. immediately after acetaminophen administration. Then, the hepatic oxidative/antioxidant parameters such as lipid peroxidation (LP), glutathione (GSH), superoxide dismutase (SOD), catalase (CAT), and ferric reducing ability of plasma (FRAP) were measured in time intervals (2, 4, 8, 16, and 24 h) after administrations confirmed by histophatological consideration at 24 h.
Results: The results indicated that acetaminophen caused a significant elevation in SOD activity (8–24 h) and LP and FRAP levels (4 h) paralleled with significant decline in GSH level (4 and 8 h). The apparent oxidative injury was associated with evident hepatic necrosis confirmed in histological examination. The presences of A. wilhelmsii oils (100 and 200 mg/kg) with acetaminophen mitigated significantly the rise in SOD, LP, and FRAP levels and restored the GSH compared with the group treated with acetaminophen. These were confirmed by histological examination indicating the hepatic necrosis reversal by the oils.
Discussion and conclusion: It can be concluded that concomitant administration of A. wilhelmsii oils with acetaminophen may be useful in reversing the drug hepatotoxicity.
Introduction
Acetaminophen or acetyl-para-aminophenol (APAP) is one of the most common medications found in households. It is used for the treatment of pain and to lower fever (Boyer & Rouff, Citation1971; Vermeulen et al., Citation1992). Because acetaminophen is the most widely used pharmaceutical analgesic and antipyretic agent in the world, it is reported by the American Association of Poison Control Centers to be one of the most common pharmaceuticals associated with both intentional and unintentional poisoning and toxicity. Acetaminophen toxicity is the most common cause of hepatic failure requiring liver transplantation (Hawkins et al., Citation2007; Khashab et al., Citation2007; Larson et al., Citation2005).
Recent studies indicate that oxidative stress and free radicals are involved in the phatophysiology of a variety of disorders including liver damage induced by acetaminophen (Dadkhah et al., Citation2006, Citation2007; Michael et al., Citation1999; Sener et al., Citation2003). In this regard, an extensive range of antioxidants, either synthetic or natural, have been presented for the treatment of disorders resulted from the disturbance in antioxidant/oxidative stress statue (Cesquini et al., Citation2003; Halliwell, Citation2000; Maxwell, Citation1995). Restriction on the use of synthetic antioxidants due to their probable side effects has increased the use of natural antioxidants (Gazzani et al., Citation1998; Souri et al., 2004).
Achillea wilhelmsii C. Koch (Asteraceae) widely used in Iranian traditional medicine possessed antioxidant, antimicrobial, immunomodulatory, antihypertensive, and antihyperlipidemia properties (Asgary et al., Citation2000; Bashi et al., Citation2012; Fathi et al., Citation2011; Sharififar et al., Citation2009). The reports indicated that the A. wilhelmsii essential oil also contains active components (Afsharypuor et al., Citation1996) with different biological properties such as anxiolytic (Majnooni et al., Citation2013), insecticide (Khani et al., Citation2012), cytotoxic, and anthelmintic potential (Ali et al., Citation2011). Our recent study indicated the in vitro antioxidant activity of A. wilhelmsii essential oils with the p-cymene, terpinolene, and α-thujene as the major compounds (Roshanaei et al., Citation2012). Continuing this, the present study, for the first time, indicates the protective effects of one natural antioxidant, i.e., A. wilhelmsii essential oils, in liver injury induced by acetaminophen. In this connection, the main oxidative/antioxidant parameters including superoxide dismutase (SOD), catalase (CAT), glutathione (GSH), ferric reducing ability of plasma (FRAP), and lipid peroxidation (LP) were considered experimentally. In addition, the histophatological examination was also carried out to confirm the findings.
Materials and methods
Chemicals
2,4,6-Tris(2-pyridyl)-S-triazine (TPTZ) (cat. 93285) and formaldehyde (cat. #F8923) were the product of Sigma-Aldrich Chemical Co. (St. Louis, MO). Dimethylsulfoxide (DMSO) (cat. #JBS-CPP-A01L) was supplied from Axxora Life Sciences Inc. (San Diego, CA). Butylated hydroxytoluene (BHT) (cat. #LKT-B7977) was purchased from LKT Laboratories, Inc. (St. Paul, MN). Acetaminophen or 4-hydroxyacetanilide (cat. #822325), diethyl ether (cat. #100926), FeSO4 (II) standard (cat. #103965), FeCl3 (cat. #103943), sodium acetate (cat. #106265), acetic acid glacial (cat. #100047), and HCl (cat. #100317) were obtained from Merck Co., Darmstadt, Germany. The PBS tablet (cat. #18912014) was supplied from Gibco Co., Carlsbad, CA,. The SOD and CAT enzyme activities kit (cat. #BV-K335-100; cat. BV-K773-100, respectively) and GSH assay kit (cat. #BV-K264-100) were purchased from BioVision, Inc., Milpitas, CA. The LP assay kit (cat. #BML-AK170-0001) was from Enzo Life Sciences, Inc., Exeter, UK.
Plant preparation
Fresh A. wilhelmsii aerial parts grown in Iran were collected in spring 2011 from Qazvin province. Prof. Mozaffarian V. (Botanist) authenticated the plant materials (Voucher no. I.217) from herbarium of Iranian Medicinal Plant Society (IMPS). Oil distillation was carried out using a Clevenger-type apparatus.
Animal treatments
Male Wistar rats were used throughout this study. Animals were obtained from Pasteur Institute of Iran and maintained in our animal house facilities. Adult animals were 3–4 months of age, weighing 180 ± 20 g. They were allowed to acclimatize to their surrounding for 1 week at temperature of 22 ± 2 °C and humidity of 48%. They were maintained on a commercial pellet food and tap water ad libitum. Animal studies were approved by the Medical Ethics Committee of Tarbiat Modares University.
The animals were divided into five groups (n = 5). In the negative control group (NC), acetaminophen vehicle, i.e., 400 μl DMSO, was only injected. In the control group (C), acetaminophen (500 mg/kg) dissolved in 400 μl DMSO was intraperitoneal (i.p.) injected (Dadkhah et al., Citation2006; Silva et al., Citation2006). In treatment groups, the essential oils prepared from the plants at two different doses, i.e., 100 and 200 mg/kg (Fatemi et al., Citation2010), were diluted in 400 μl DMSO and injected i.p. immediately after acetaminophen administration. In the positive control group, BHT (10 mg/kg) dissolved in 400 μl DMSO was injected i.p. immediately after acetaminophen administration.
Preparation of tissue homogenate and plasma
Heparinated blood samples were collected at different time intervals (2, 4, 8, 16, and 24 h after APAP administration) by heart puncture from all the animals and centrifuged at 3000 × g for 10 min to obtain plasma. Liver samples were immediately transferred to ice-cold containers and homogenized (20% w/v) in the appropriate buffer (PBS) using a homogenizer (E.L.M. 2500). The homogenate was used to measure biochemical parameters.
Biochemical assays
LP
A weighed portion of liver was homogenized in phosphate buffer (100 mM, pH 7.0) and used to measure the concentration of malondialdehyde (MDA)/thiobarbituric acid reacting substances (TBARS) as an indicator of LP. The concentration of TBARS was measured spectrophotometrically according to the instructions of the kit. The assay is based on the reaction of a chromogenic reagent, N-methyl-2-phenylindole, with MDA to yield a stable chromophore with maximal absorbance at 586 nm. The rate of absorbance is linearly related to the level of MDA.
GSH estimation
GSH was estimated in liver homogenate based on the protocol of the purchased kit. Briefly, o-phthalaldehyde (OPA) reacts with GSH generating fluorescence. So, GSH can be specifically quantified by plotting a standard curve of fluorescence against different concentrations of GSH.
Determination of SOD and CAT enzyme activities
The activities of SOD and CAT were estimated in liver homogenate using commercial kits. The SOD assay kit utilizes WST-1 reduced to formazan dye by superoxide anion which absorbs light at 450 nm. The rate of the reduction with a superoxide anion is inhibited by SOD. Therefore, the inhibition activity of SOD can be determined by a colorimetric method.
In the CAT assay, CAT first reacts with H2O2 to produce water and oxygen. The unconverted H2O2 reacts with OxiRed™ probe to produce a product, which can be measured at 570 nm (the colorimetric method). CAT activity is reversely proportional to the signal.
FRAP assay
This assay was performed using a TPTZ reagent as described by Benzie and Strain (1996). The FRAP level was calculated by plotting a standard curve of absorbance against μmol/l concentration of Fe (II) standard solution.
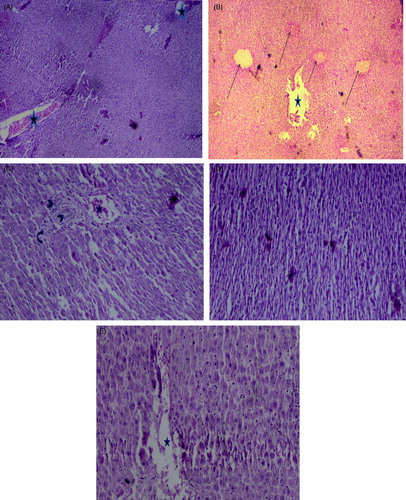
Histophatological studies
The histological changes were quantitatively analyzed by a veterinary pathologist. All animals were sacrificed 24 h after acetaminophen administration. Small portions of liver were excised from the central lobe and were fixed in 10% buffered formaldehyde solution, embedded in paraffin and sectioned at 6 μm. Then, the samples stained with hematoxylin and eosin (H&E) and studied with light microscope for histological analysis (Arthur et al., Citation2012; Hassan et al., Citation2009).
Statistical analysis
Data are presented as means ± standard error of mean (SEM). The results were subjected to a one-way ANOVA followed by Tukey's HSD using SPSS (version 19.0, SPSS Inc., Chicago, IL) software. Significant levels were defined as p < 0.05.
Results
Effect of A. wilhelmsii essential oil on plasma and hepatic oxidative/antioxidant injury parameters in rats treated by APAP
As shown in , the oxidative/antioxidant injury parameters, i.e., LP, GSH, SOD, and CAT, were analyzed in a time-dependent manner at 2, 4, 8, 16, and 24 h after APAP administrations. The data indicated that LP level was increased significantly only 4 h after administration as compared with the negative control group (p < 0.05). The APAP administration could only affect the GSH level at 4 and 8 h after treatment (p < 0.05). SOD activity was significantly increased at 8 h after administration and remained at high level until 24 h (p < 0.05), whereas CAT activity did not change significantly in all time intervals (p > 0.05). As shown in , the FRAP value was significantly higher in APAP-treated rats at 4 h as compared with the negative control group (p < 0.05).
Figure 1. Time-course changes in LP levels in rats treated with APAP compared to negative controls. In the control group (C), APAP (500 mg/kg bw) dissolved in 400 μl DMSO was i.p. injected. Data are mean ± S.E.M. of five samples obtained from five animals in each group. *Significantly different from the respective negative control group (p < 0.05).
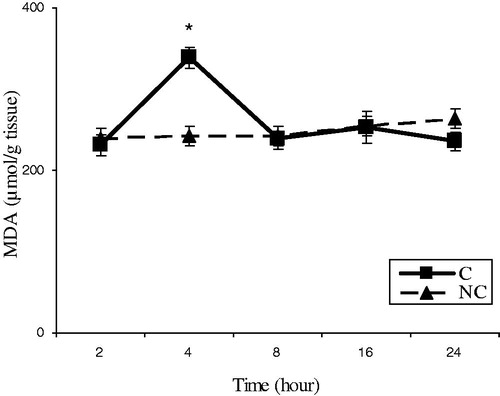
Figure 2. Time-course changes in GSH levels in rats treated with APAP compared to negative controls. In the control group (C), APAP (500 mg/kg bw) dissolved in 400 μl DMSO was i.p. injected. Data are mean ± S.E.M. of five samples obtained from five animals in each group. *Significantly different from the respective negative control group (p < 0.05).
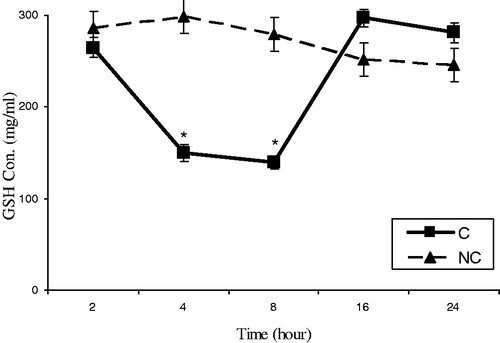
Figure 3. Time-course changes in SOD activities in rats treated with APAP compared to negative controls. In the control group (C), APAP (500 mg/kg bw) dissolved in 400 μl DMSO was i.p. injected. Data are mean ± S.E.M. of five samples obtained from five animals in each group. *Significantly different from the respective negative control group (p < 0.05).
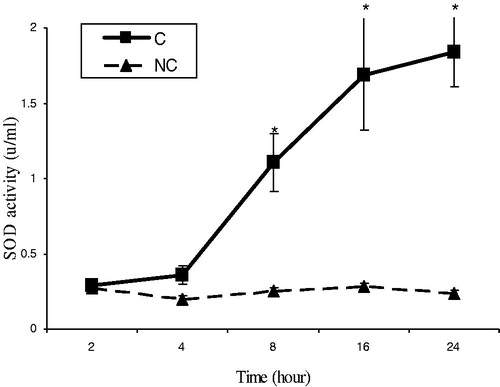
Figure 4. Time-course changes in CAT activities in rats treated with APAP compared to negative controls. In the control group (C), APAP (500 mg/kg bw) dissolved in 400 μl DMSO was i.p. injected. Data are mean ± S.E.M. of five samples obtained from five animals in each group.
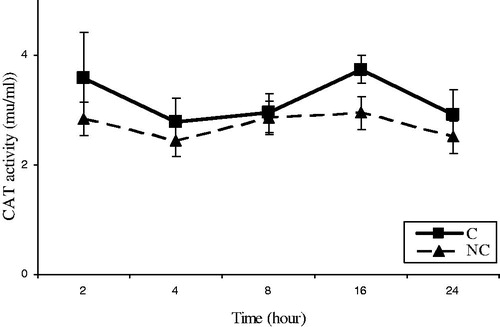
Figure 5. Time-course changes in FRAP levels in rats treated with APAP compared to negative controls. In the control group (C), APAP (500 mg/kg bw) dissolved in 400 μl DMSO was i.p. injected. Data are mean ± S.E.M. of five samples obtained from five animals in each group. *Significantly different from the respective negative control group (p < 0.05).
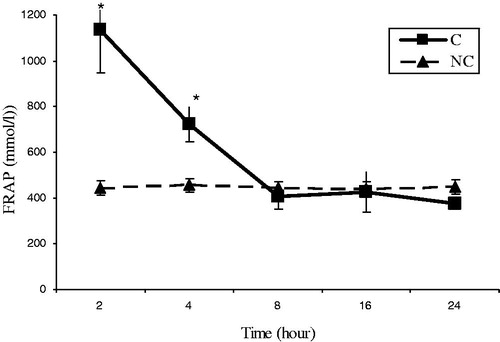
From the data in , it is deduced that APAP administration in time intervals (2, 4, 8, 16, and 24 h) could only modulate the LP level at 4 h, GSH level at 4 and 8 h, SOD activity at 8-24 h, and FRAP level at 4 h. So, we assigned the i.p. administration of A. wilhelmsii oils on the levels of oxidative plasma and liver injury parameters in experimental rats treated with APAP only at 4 h after APAP administration presented in , , , and . As the changes of some parameters in 8 h, the SOD activity and the GSH level were considered at 8 h too ( and ). In fact, we investigated the above parameters in all groups in the entire time intervals, but as mentioned above because of the expansion of unnecessary data, we did not to present all of the data.
Figure 6. Effect of A. wilhelmsii essential oil on LP levels 4 h after APAP administration. In the positive control group (BHT), BHT (10 mg/kg bw) dissolved in 400 μl DMSO was injected i.p. immediately after APAP administration. Data are mean ± S.E.M. of five samples obtained from five animals in each group. *Significantly different from the respective negative control group (p < 0.05). ≠Significantly different from the respective control group (p < 0.05).
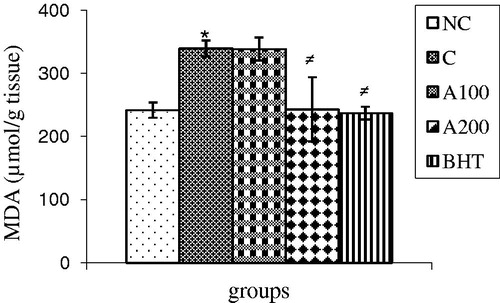
Figure 7. Effect of A. wilhelmsii essential oil on GSH levels 4 h after APAP administration. In the positive control group (BHT), BHT (10 mg/kg bw) dissolved in 400 μl DMSO was injected i.p. immediately after APAP administration. Data are mean ± S.E.M. of five samples obtained from five animals in each group. *Significantly different from the respective negative control group (p < 0.05). ≠Significantly different from the respective control group (p < 0.05).
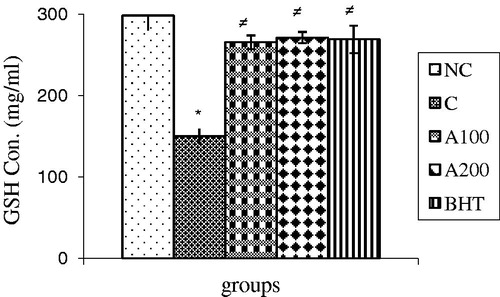
Figure 8. Effect of A. wilhelmsii essential oil on CAT activities 4 h after APAP administration. In the positive control group (BHT), BHT (10 mg/kg bw) dissolved in 400 μl DMSO was injected i.p. immediately after APAP administration. Data are mean ± S.E.M. of five samples obtained from five animals in each group.
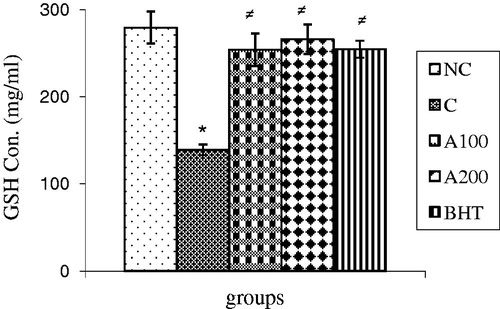
Figure 9. Effect of A. wilhelmsii essential oil on FRAP levels 4 h after APAP administration. In the positive control group (BHT), BHT (10 mg/kg bw) dissolved in 400 μl DMSO was injected i.p. immediately after APAP administration. Data are mean ± S.E.M. of five samples obtained from five animals in each group. *Significantly different from the respective negative control group (p < 0.05).
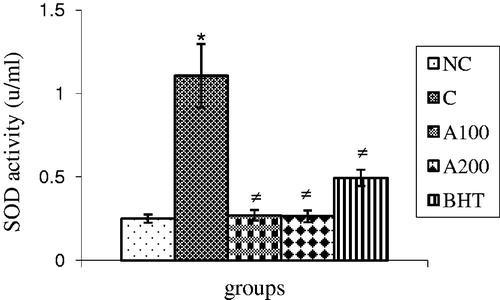
Figure 10. Effect of A. wilhelmsii essential oil on GSH levels 8 h after APAP administration. In the positive control group (BHT), BHT (10 mg/kg bw) dissolved in 400 μl DMSO was injected i.p. immediately after APAP administration. Data are mean ± S.E.M. of five samples obtained from five animals in each group. *Significantly different from the respective negative control group (p < 0.05). ≠Significantly different from the respective control group (p < 0.05).
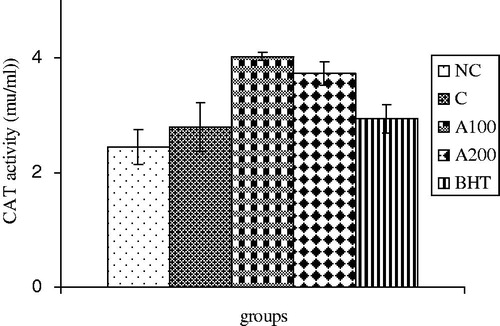
Figure 11. Effect of A. wilhelmsii essential oil on SOD activities 8 h after APAP administration. In the positive control group (BHT), BHT (10 mg/kg bw) dissolved in 400 μl DMSO was injected i.p. immediately after APAP administration. Data are mean ± S.E.M. of five samples obtained from five animals in each group. *Significantly different from the respective negative control group (p < 0.05). ≠Significantly different from the respective control group (p < 0.05).
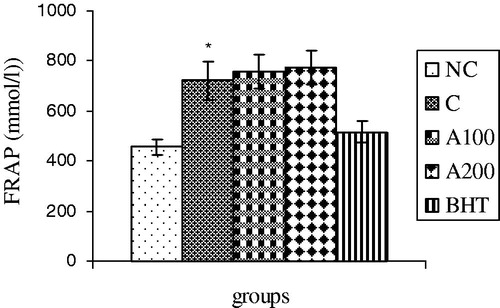
The data indicated that as a reference antioxidant (BHT), the plant essential oils especially at the dose of 200 mg/kg could decrease the LP to control level (p < 0.05) (). The GSH level could successfully reach to normal level both at 4 and 8 h after essential oil and BHT treatments as compare with control groups (p < 0.05) ( and ). SOD activity also returned to the normal level after administration of the plant essential oils at both doses as also seen in the positive control group at 8 h after treatment (p < 0.05) (), whereas no difference was noticed in CAT activity in all groups (p > 0.05) (). Administration of the essential oil to APAP-treated rats had no effect on the FRAP level at 4 h (p > 0.05) ().
Effect of A. wilhelmsii essential oil on hepatic histophatological changes in rats treated by APAP
Histophatological studies performed on liver biopsies showed normal structure of liver tissue with normal central vein (stars) in the negative control group (). In liver tissue of rats treated with APAP, minimally 3–8 points of necrotic hyalinized aggregation (arrow) were detected. In some of the cells, wholly white, hyalinized, karyokisis, and chromatolysis cytoplasm was also observed. Occasionally, these hyalinized aggregations seen in one parallel row near together affected zonation and distribution of blood in liver (). Any effect of necrotic aggregation was not detected in groups treated with APAP concomitant with 100 mg/kg of A. wilhelmsii essential oils and also in BHT-treated rats. The histological structures of sinusoids (arrows), hepatocytes, veins (star), arteries (bend arrow), bile ducts, and portal spaces were normal (). No necrotic aggregation has been detected in rats treated with APAP plus 200 mg/kg of A. wilhelmsii essential oils, but some of histological structures were distributed and sinusoids were less arranged. The cytoplasm of hepatocytes was smaller and more basophilic than the normal group ().
Figure 12. Effect of A. wilhelmsii essential oil on histopathological changes 24 h after APAP administration. Light microscopy showed histologic sections of liver of rats from different groups of animals. (A) Negative control group (NC) (original magnification × 40). (B) Control group (C) (original magnification×40). (C) Essential oil treatment group (100 mg/kg) (original magnification × 100). (D) Essential oil treatment group (200 mg/kg) (original magnification × 100). (E) Positive control group (10 mg/kg BHT) (original magnification × 100).
Discussion
This study indicated the disturbed hepatic oxidative stress/antioxidant statues were adapted by A. wilhelmsii oils (100 and 200 mg/kg) implying the efficient hepatoprotective effects of the essential oils in modulating the oxidative stress induced by APAP.
As indicated in , APAP treatments increased SOD, LP, and FRAP levels concomitant with the diminished GSH level. These results confirmed the role of APAP metabolism in increasing the oxidative stress leading to oxidative stress/antioxidants statue imbalance (Dai et al., Citation2006; Jodynis-Liebert et al., Citation2005; Kumari & Kakkar, Citation2012). The toxicity of APAP is related to its bioactivation by cytochrome P450 to the electrophilic metabolite N-acetyl parabenzoquinone imine (NAPQI). At therapeutic doses, NAPQI is efficiently detoxified by GSH and sulfate and eliminated through the urine or bile; however, at supratherapeutic doses, both the glucuronidation and sulfation pathways become saturated, and the extensive bioactivation of APAP depletes the hepatic GSH pool and causes oxidative stress (Dai et al., Citation2006). This oxidative stress may trigger signaling pathways acting through mitochondrial toxicity, ultimately causing cell death (Kumari & Kakkar, Citation2012). In contrast, GSH is essential for the protection of thiol and other nucleophilic groups in proteins from the toxic metabolite of APAP. Therefore, the concentration of intracellular GSH is the key determinant of the extent of APAP-induced hepatic injury (Ross, Citation1988). Besides, the activity of SOD is a sensitive index in hepatorenal damage as it scavenges the superoxide anion to form hydrogen peroxide leading to diminish the toxic effects. Changes in the activity of this antioxidant enzyme () may occur as the result of imbalance between the pro-oxidant and antioxidant systems in liver.
Increased TBARS level in APAP-treated rats () indicating the main role of LP in the initiation of oxidative stress. Excessive ROS generation triggers the process of LP in cell membranes and causes the destruction of cell components and cell death. LP and protein carbonyl content are two important parameters to assess the oxidative damage to lipids and proteins, respectively. Reports from other labs and our own studies have shown that hepatic LP increases during APAP toxicity (Dadkhah et al., Citation2006; James et al., Citation2003; Sharma et al., Citation2011). In addition, induction of FRAP in plasma and SOD activity in liver of APAP-treated rats ( and ) may be due to the compensatory increased of enzymatic and non-enzymatic antioxidants which leads to increased resistance and/or decreased susceptibility of the liver to free radical attack (Dadkhah et al., Citation2006; Manju & Nalini, Citation2005). In contrast, these changes were accompanied by no change in CAT activity () implying the imbalance among the antioxidants resulting to the accumulation of toxic-free radicals that cause cell damage (Sun, Citation1990). Other studies also indicated the disturbed oxidative stress/antioxidant statues by APAP involved in hepatotoxicity (Kumari & Kakkar, Citation2012; Shanmugasundaram & Venkataraman, Citation2006).
The results in indicated that, as a reference antioxidant (BHT), the A. wilhelmsii essential oils (100 and 200 mg/kg) could adjust the parameters involving in the oxidative stress/antioxidant statues. In this connection, the essential oils increased the GSH level, as important antioxidant, indicated a raise in the antioxidative capacity as well. The oils could scavenge reactive free radicals that eventually lessen the oxidative damage to the tissues and subsequently improved the level of this antioxidant (Bhadauria & Nirala, Citation2009). In addition, the SOD activity and LP and FRAP levels, as important factors in oxidative stress/antioxidant balancing (Dadkhah et al., Citation2006), were compensated by the essential oils as an antioxidant leading to the protection of liver against APAP-induced peroxidative damages. Several active constituents and organic compounds present in A. wilhelmsii essential oils could act synergistically and inhibited LP as an effective chain breaking antioxidant to diminish APAP-induced peroxidative damage in the test organs (Bhadauria & Nirala, Citation2009). Other studies also indicated that essential oils could modulate the oxidative stress/antioxidant statues. Protective effect of Aquilegia vulgaris L. (Ranunculaceae) on APAP-induced oxidative stress in rats is mediated by amelioration of microsomal LP and restoring antioxidant enzymes activity (Jodynis-Liebert et al., Citation2005). Lupeol, a triterpene, when co-administered with APAP, effectively reduces oxidative stress and prevents APAP-induced hepatotoxicity by inhibiting critical control points of apoptosis (Kumari & Kakkar, Citation2012). One study also indicated the protective effect of α- and β-amyrin, a triterpene mixture from the trunk wood resin, against APAP-induced liver injury in mice through modulating the oxidative stress/antioxidant parameters (Oliveira et al., Citation2005). The protective effects of quercetin and curcumin on APAP-induced liver injury in rat through mitigation the rise in TBARS and restored the activities of antioxidant enzymes were also reported (Yousef et al., Citation2010). These data were confirmed by histophatological examinations () indicating administration of essential oils as potency as BHT decreases the oxidative hepatic injuries such as necrotic aggregations in acetaminophen-treated rats.
Conclusions
We indicated that one of the mechanisms of hepatoprotective activity of A. wilhelmsii essential oils may be through the regulating of oxidative stress/antioxidant statues such as LP, GSH, and SOD in liver tissue. These results rationalize the folkloric use of this plant in hepatic toxicity.
Declaration of interest
The authors declared no conflict of interest.
References
- Afsharypuor S, Asgary S, Lockwood GB. (1996). Constituents of the essential oil of Achillea wilhelmsii from Iran. Planta Med 62:77–8
- Ali N, Shah SW, Shah I, et al. (2011). Cytotoxic and anthelmintic potential of crude saponins isolated from Achillea wilhelmsii C. Koch and Teucrium stocksianum Boiss. BMC Complement Altern Med 11:1–7
- Arthur FK, Woode E, Terlabi EO, Larbie C. (2012). Evaluation of hepatoprotective effect of aqueous extract of Annona muricata (Linn.) leaf against carbon tetrachloride and acetaminophen-induced liver damage. J Nat Pharm 3:25–30
- Asgary S, Naderi GH, Sarrafzadegan N, et al. (2000). Antihypertensive and antihyperlipidemic effects of Achillea wilhelmsii. Drug Exp Clin Res 26:89–93
- Bashi DS, Fazly Bazzaz BS, Sahebkar A, et al. (2012). Investigation of optimal extraction, antioxidant, and antimicrobial activities of Achillea biebersteinii and A. wilhelmsii. Pharm Biol 50:1168–76
- Benzie IFF, Strain JJ. (1996). The ferric reducing ability of plasma (FRAP) as a measure of antioxidant power: The FRAP assay. Anal Biochem 239:70–6
- Bhadauria M, Nirala SK. (2009). Reversal of acetaminophen induced subchronic hepatorenal injury by propolis extract in rats. Environ Toxicol Pharmacol 27:17–25
- Boyer TD, Rouff LJ. (1971). Acetaminophen-induced hepatic necrosis and renal failure. J Am Med Assoc 218:440–1
- Cesquini M, Torsoni MA, Stoppa GR, Ogo SH. (2003). t-BOOH-induced oxidative damage in sickle red blood cells and the role of flavonoids. Biomed Pharmacother 57:124–9
- Dadkhah A, Allameh AA, Fatemi F, et al. (2007). Considering the pathologic lesions of liver and changes of plasma alanine transaminase and aspartate transaminase in acetaminophen-induced toxicity in rat. Pharm Sci 2:47–54
- Dadkhah A, Fatemi F, Kazemnejad S, et al. (2006). Differential effects of acetaminophen on enzymatic and non-enzymatic antioxidant factors and plasma total antioxidant capacity in developing and adult rats. Mol Cell Biochem 281:145–52
- Dai G, He L, Chou N, Wan YJ. (2006). Acetaminophen metabolism does not contribute to gender difference in its hepatotoxicity in mouse. Toxicol Sci 92:33–41
- Fatemi F, Allameh A, Khalafi H, Ashrafihelan J. (2010). Hepatoprotective effects of gamma-irradiated caraway essential oils in experimental sepsis. Appl Radiat Isot 68:280–5
- Fathi H, Lashtoo Aghaee B, Ebrahimzadeh MA. (2011). Antioxidant activity and phenolic contents of Achillea wilhemsii. Pharmacologyonline 2:942–9
- Gazzani G, Papetti A, Massolini G, Daglia M. (1998). Anti and prooxidant activity of water soluble components of some common diet vegetables and the effect of thermal treatment. J Agric Food Chem 46:4118–22
- Halliwell B. (2000). The antioxidant paradox. Lancet 355:1179–80
- Hassan IE, Mohamed F, Shalaby FM, et al. (2009). Histopathological effects of cisplatin, doxorubicin and 5-flurouracil (5-FU) on the liver of male albino rats. Int J Biol Sci 5:466–73
- Hawkins LC, Edwards JN, Dargan PI. (2007). Impact of restricting paracetamol pack sizes on paracetamol poisoning in the United Kingdom: A review of the literature. Drug Saf 30:465–79
- James LP, Mayeux PR, Hinson JA. (2003). Acetaminophen induced hepatotoxicity. Drug Metab Dispos 31:1499–506
- Jodynis-Liebert J, Matławska I, Bylka W, Murias M. (2005). Protective effect of Aquilegia vulgaris (L.) on APAP-induced oxidative stress in rats. J Ethnopharmacol 97:351–8
- Khani A, Asghari J. (2012). Insecticide activity of essential oils of Mentha longifolia, Pulicaria gnaphalodes and Achillea wilhelmsii against two stored product pests, the flour beetle, Tribolium castaneum, and the cowpea weevil, Callosobruchus maculatus. J Insect Sci 12:1–10
- Khashab M, Tector AJ, Kwo PY. (2007). Epidemiology of acute liver failure. Curr Gastroenterol Rep 9:66–73
- Kumari A, Kakkar P. (2012). Lupeol prevents acetaminophen-induced in vivo hepatotoxicity by altering the Bax/Bcl-2 and oxidative stress-mediated mitochondrial signaling cascade. Life Sci 90:561–70
- Larson AM, Polson J, Fontana RJ, et al. (2005). Acute Liver Failure Study Group. Acetaminophen-induced acute liver failure: Results of a United States multicenter, prospective study. Hepatology 42:1364–72
- Majnooni MB, Mohammadi-Farani A, Gholivand MB, et al. (2013). Chemical composition and anxiolytic evaluation of Achillea wilhelmsii C. Koch essential oil in rat. Res Pharm Sci 8:269–75
- Manju V, Nalini N. (2005). Chemopreventive efficacy of ginger, a naturally occurring anticarcinogen during the initiation, post-initiation stages of 1,2 dimethylhydrazine-induced colon cancer. Clin Chim Acta 358:60–7
- Maxwell SRJ. (1995). Prospects for the use of antioxidant therapies. Drugs 49:345–61
- Michael SL, Pumfod NR, Mayeux PR, et al. (1999). Pretreatment of mice with macrophage inactivators decreases acetaminophen hepatotoxicity and the formation of reactive oxygen and nitrogen species. Hepatology 30:186–95
- Oliveira FA, Chaves MH, Almeida FR, et al. (2005). Protective effect of α- and β-amyrin, a triterpene mixture from Protium heptaphyllum (Aubl.) March. trunk wood resin, against acetaminophen-induced liver injury in mice. J Ethnopharmacol 98:103–8
- Roshanaei K, Dadkhah A, Fatemi F, et al. (2012). [Study of the chemical composition and antioxidant properties of Iranian Achillea wilhelmsii C. Koch essential oils and hydroalcoholic extracts from Qazvin area]. Appl Biol 1:73–85
- Ross D. (1988). Glutathione, free radicals and chemotherapeutic agents. Pharmacol Ther 37:231–49
- Sener G, Sehirli AO, Ayanoğlu-Dülger G. (2003). Protective effects of melatonin, vitamin E and N-acetylcysteine against acetaminophen toxicity in mice: A comparative study. J Pineal Res 35:61–8
- Shanmugasundaram P, Venkataraman S. (2006). Hepatoprotective and antioxidant effects of Hygrophila auriculata (K. Schum) Heine Acanthaceae root extract. J Ethnopharmacol 104:124–8
- Sharma S, Singh RL, Kakkar P. (2011). Modulation of Bax/Bcl-2 and caspases by probiotics during acetaminophen induced apoptosis in primary hepatocytes. Food Chem Toxicol 49:770–9
- Sharififar F, Pournourmohammadi S, Arabnejad M. (2009). Immunomodulatory activity of aqueous extract of Achillea wilhelmsii C. Koch in mice. Indian J Exp Biol 47:668–71
- Silva VM, Hennig GE, Manautou JE. (2006). Cholestasis induced by model organic anions protects from acetaminophen hepatotoxicity in male CD-1 mice. Toxicol Lett 160:204–11
- Souri E, Amin G, Dehmobed-Sharifabadi A, et al. (2004). Antioxidative activity of sixty plants from Iran. Iran J Pharm Res 3:55–9
- Sun Y. (1990). Free radicals, antioxidant enzymes, and carcinogenesis. Free Radical Biol Med 8:583–99
- Vermeulen NP, Bessems JG, Van De Straat R. (1992). Molecular aspect of paracetamol – induced hepatotoxicity and its mechanism based prevention. Drug Metabol Rev 24:367–407
- Yousef MI, Omar SAM, El-Guendi MI. (2010). Potential protective effects of quercetin and curcumin on paracetamol-induced histological changes, oxidative stress, impaired liver and kidney functions and hematotoxicity in rat. Food Chem Toxicol 48:3246–61
