Abstract
Objectives. The long-term prognostic value (> 5 years) of elevated cardiac biomarkers after elective coronary angioplasty is yet not clear. Most previous studies have included high risk, unstable patients and with conflicting results. The aim of this study was to determine the prognostic value of CK-MB mass vs. the cardiac troponins (values ≥ 3 times the reference) after elective angioplasty in low-risk patients with stable angina. Methods. A total of 202 consecutive patients were included in the final analysis. Patients with elevated values at baseline, and those suffering an acute coronary syndrome < 1 month before the time of inclusion, were excluded. Blood samples were drawn just before, 1–3 hours and 4–8 hours after the procedure and the next morning. Using a cutoff value of three times the reference, patients with high and low values (= controls) of CK-MB mass, cardiac troponin T (TnT) and troponin I (TnI) were compared. No patient developed new Q-waves on ECG. The median follow-up time was 82 months equalising 1600 patient years. Results. None of the patients died during the procedure or within the first 30 days after angioplasty, confirming a low risk cohort. There was an increasingly number of patients with levels ≥ 3 times the reference post procedure in TnT (10.4%) and TnI (16.8%) vs. CK-MB (6.9%). All cause mortality, readmission for acute coronary syndromes and target lesion revascularisation were more frequent in patients with high CK-MB, 42.9% vs. 22.3 %, p = 0.05 (log-rank test). Corresponding values for TnT were 33.3% vs. 22.7%, p = 0.22. In the TnI patients, there were more adverse events in controls vs. the high group, 25.0% vs. 17.6%, p = 0.34. Conclusions. CK-MB mass values ≥ 3 times, contrary to the cardiac troponins, predicts worse long-term event-free survival after elective angioplasty in low-risk patients.
Recently, we have shown that creatine kinase (CK)-MB values three times the reference predicts worse long-term event-free survival after elective percutaneous coronary intervention (PCI) in low-risk patients with stable angina (Citation1). The new guidelines for diagnosing periprocedural infarcts advocate the use of similar thresholds for CK-MB and the cardiac troponins (Citation2). However, few prior data are available comparing all these biomarkers after PCI and it is not clear whether elevations of the cardiac troponins can be treated the same as elevations of CK-MB. In the current study, we sought to compare the long-term (> 5 years) prognostic value of both cardiac troponin T (cTnT) and troponin I (cTnI) vs. CK-MB mass (using a cutoff value of three times the reference in all biomarkers) in patients with stable symptoms for at least one month prior to elective PCI.
Methods
Study patients
In this prospective study, 210 consecutive patients with stable angina for at least one month prior to the procedure were screened for inclusion during the period from 1998 to 1999. Eight patients were excluded. Exclusion criteria were elevated or missing biomarker values just before angioplasty, unavailability for follow-up, recent acute coronary syndrome (ACS) < 1 month, malignant disease, or creatinine > 200 μmol/l. Patients were compared according to biomarker values below three times the reference (controls) or above or equal to three times the reference (high biomarker group) at any time-point after angioplasty. A few patients with elevated baseline values were still included in the study if the two other cardiac biomarkers were within the reference limit.
The study was approved by the regional ethical committee, and informed written consent was obtained from all patients.
Study end points
During follow-up, we were able to investigate the medical records of all the patients as well as the Central Population Register and local patient administrative systems for predefined end points and other adverse clinical events. Predefined major adverse clinical events were the composite end point of all cause mortality (> 24 h after procedure), readmission for acute coronary syndromes (ACS), and target lesion revascularisation (TLR). ACS (unstable angina, ST-elevation and non ST-elevation myocardial infarction) were diagnosed according to AMI definition (Citation3).
PCI technique
The patients underwent angioplasty according to the hospitals standard techniques. All patients received aspirin and a thienopyridine agent at least 48 h before procedure and heparin was administered intravenously during procedure to achieve an ACT around 300. Stented patients were treated with a thienopyridine agent for one month post-PCI. All patients were recommended life-long aspirin treatment.
Biochemistry, ECG and angiography
Venous blood samples were prospectively collected just prior to angioplasty in all patients. Blood samples were also collected 1–3 h and 4–8 h after the procedure, and the next morning thereafter. CK-MB mass (reference limit < 5 μg/l) was assayed with an established immunoassay, the Technicon Immuno 1 System (Bayer Business Group Diagnostics, Tarrytown, NY, USA) according to the manufacturer. Cardiac TnI was analysed by a onestep, immunoenzymometric assay, ERIA, Diagnostics Pasteur, Marnes-la-Coquette, France (Citation4). Our reference limit based on the mean baseline values of the total cohort plus three times standard error of mean (SEM) was < 0.05 μg/l. Cardiac TnT was analysed at the time according to a revised procedure using microtitre plates which our laboratory was familiar with and with a reference value < 0.12 μg/l (mean preprocedural value plus three times SEM) (Citation5).
ECG was taken before and at least once after the procedure and changes were assessed according to the Minnesota Code for defining myocardial infarction based on new Q-waves (Citation6). All patients underwent angiography before PCI according to established routines in our institution (Citation7) and further treatment strategy was decided by a joint meeting of experienced invasive cardiologists and thoracic surgeons.
Statistical analysis
Data are presented as mean and standard deviation unless otherwise stated. Student t-test was used when comparing continuous variables and χ2 test (or Fisher exact test) for analysis of discrete variables (SPSS, version 17.0). Analysis of variance for repeated measurements was applied to determine p-value for trend. The Kaplan-Meier method and log-rank test were used to evaluate differences in event-free survival between patients with biomarker values ≥ 3 times the reference vs. controls. The independent ability of the biomarkers to predict worse outcome was assessed by a univariate and multivariate logistic regression analysis. All clinical relevant baseline and procedural variables presented in and were tested in the univariate analysis. Variables with a univariate p-value < 0.10 were adjusted for in the logistic regression multivariate analysis. Differences were considered significant with p < 0.05 if not otherwise stated.
Table I. Patient characteristics of all patients as well as the comparison of controls vs. high biomarker groups (presented as p-values in the biomarker columns).
Table II. Procedural data of all patients as well as the comparison of controls vs. high biomarker groups.
Results
Baseline and procedural characteristics
and show baseline characteristics and procedural data. The mean age of the 202 patients included was 65.8 years, range 41–85. The number of patients with elevated biomarkers (≥ 3 times the reference) vs. controls were: CK-MB 14 vs. 188, cTnT 21 vs. 181 and cTnI 34 vs. 168. There were more women in the high CK-MB and TnI group as compared with controls and fewer ever-smokers in the high TnI group. The mean value of creatinine was higher in controls vs. the high TnI group. The mean stent length was similar in the high vs. low group of all biomarkers. However, the number of stents implanted per procedure was significantly higher in the high biomarker groups as well as the cumulated stent length. Complications were significantly more frequent in the high group of CK-MB (42.9% vs. 19.3%) and TnT (38.1% vs. 19.0%). Corresponding values of TnI were 32.4% vs. 18.6% (p = 0.074). Creatinine was above 150 μg/l in one patient (value of 154 μg/l) and one patient had an EF less than 30% and nine patients had an EF < 40%.
Biomarkers
The mean peak CK-MB value was 4.8 μg/l at 20–24 h after PCI in the total study cohort (), p-value for trend < 0.001 and the corresponding p-values for trend of TnT and TnI were the same. There was an increasingly number of patients with levels ≥ 3 times the reference post procedure in TnT (10.4%) and TnI (16.8%) vs. CK-MB (6.9%). Mean peak values (μg/l) in controls vs. high groups were 2.9 μg/l vs. 38 μg/l (CK-MB), 0.13 μg/l vs. 1.03 μg/l (TnT), and 0.04 μg/l vs. 0.33 μg/l (TnI). The fraction of patients with peak values above the reference was 17.3%, 35.9% and 39.8% in CK-MB, TnT and TnI, respectively.
Table III. Temporal pattern of the cardiac biomarkers before and after angioplasty.
In a linear multivariate regression analysis including variables with univariate p-values < 0.10, the number of stents (p < 0.001), long lesions (p = 0.006) and gender (p = 0.030) were associated with peak CK-MB. Gender (p = 0.010) and the number of stents (p = 0.016) were associated with peak TnI values and the number of stents (p = 0.026) was associated with peak TnT values.
Clinical end-points
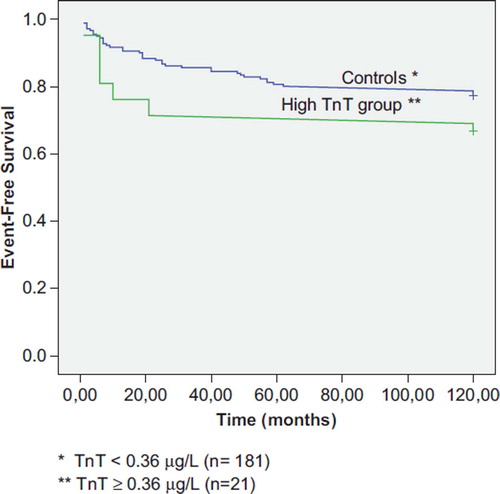
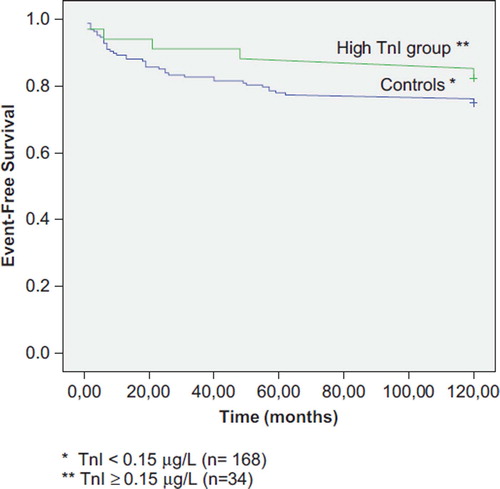
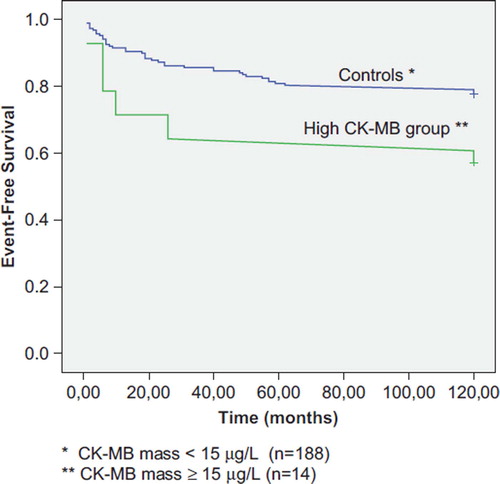
None of the patients died during the procedure or within the first 30 days after angioplasty, and only eight patients (3.9%) died during a median long-term follow-up time of 82 months (mean of 81.0 months), confirming a low-risk cohort. Seventy-seven point seven percent of controls compared to 57.1% in the high CK-MB group were free of predefined events (p = 0.05, ). The adverse events increased rapidly in the high CK-MB group up to about 20 months of follow-up with parallel event-free survival lines thereafter. Corresponding values for TnT () were 77.3% vs. 66.7% (p = 0.22) and for TnI () 75.0% vs. 82.4% (p = 0.34).
Figure 1. Kaplan-Meier plot of event-free survival (all patients, n = 202). P-value = 0.05 (log-rank test).
Independent predictors of event-free survival
All clinical relevant variables in and were tested for in a univariate logistic analysis. Ostial lesion (p = 0.015), former PCI (p = 0.002), hypercholesterolemia (p = 0.071), hypertension (p = 0.047) and CK-MB around the cut-point of 15 μg/l (p = 0.091) had a univariate p-value < 0.10. Neither accumulated stent length, the number of stents nor complications predicted worse event-free survival. In the multivariate analysis CK-MB had a p-value of 0.083. Systolic blood pressure tended to be higher in the high CK-MB group vs. controls (143 mmHg vs. 137 mmHg) and if hypertension was replaced by systolic blood pressure (univariate logistic p-value = 0.127) in the multivariate analysis, the p-value of CK-MB mass was 0.040. If both hypertension and systolic blood pressure were included in the multivariate analysis, the logistic p-value of CK-MB was 0.059.
The univariate and multivariate logistic p-value for TnT was 0.281 and 0.269. Corresponding values for TnI were p = 0.361 and p = 0.301. Using systolic blood pressure instead of hypertension did not lower the multivariate p-values of TnT and TnI.
Discussion
The main issue of this study was to compare the prognostic value of the cardiac biomarkers around the same cutoff value of three times the reference in a low-risk cohort of patients undergoing routine PCI. CK-MB mass, contrary to the cardiac troponins (≥ 3 times reference), predicted worse event-free survival after angioplasty during a median follow-up of 82 months. In the present study, adverse clinical events during follow-up were nearly twice as frequent in the high CK-MB group as compared to the controls.
Previous studies
Periprocedural myocardial infarction (PMI) is a harmful event that implies worsened short- and long-term prognosis (Citation8–16). The impact of very small release of the cardiac biomarkers, however, has been disputed (Citation8) in otherwise uncomplicated procedures. Two large metaanalysis (Citation11,Citation13) have assessed the prognostic value of CK-MB after PCI and reported increased risk in patients with elevated CK-MB values. Nienhus et al. (Citation16) suggested in a metaanalysis that TnI and TnT elevation post PCI provided important prognostic information. However, the results of the included troponin studies were conflicting and many studies were very small. All three metaanalysis included a large proportion of unstable patients. Nageh et al. reported increased risk of elevated TnI values postPCI in a cohort of 316 patients with stable coronary disease (Citation17). However, when they compared ≥ 3-fold increase vs. 1–3 fold increase of TnI there was no difference in adverse events at 30 days and 18 months. Unfortunately, a comparison of ≥ 3-fold increase vs. controls was not performed. The same group (Citation18) compared the long-term predictive value of the cardiac troponins and CK-MB in 109 patients and found that the biomarkers yielded similar prognostic information of increased risk. However, contrary to the present study, 42 patients with unstable angina were included and use of rotablator was more frequent than in our study (7% vs. 0.5%). Thus, to our knowledge, the present study is the first report comparing the long-term (> 5 years) prognostic value of CK-MB mass and the cardiac troponins in the same low-risk cohort of patients with stable angina undergoing routine PCI.
Possible mechanisms
The present study did not aim to assess causes of postprocedural biomarker release. Former studies have shown that multiple patient- and procedure-related factors may cause biomarker increase and subsequent adverse prognosis of patients (Citation11,Citation13,Citation16). The new guidelines for diagnosing MI (Citation2) suggest that any troponin release represents necrosis as reported in two magnetic resonance imaging (MRI) studies (Citation19,Citation20). Ricciardi et al. (Citation19) demonstrated that postPCI CK-MB elevation caused small areas of hyperenhancement using repeat MRI in nine patients and Selvanayagam et al. (Citation20), reported that TnI elevation after PCI directly represented the extent of irreversible myocardial injury as assessed by MRI in 50 patients. However, their detection limit of TnI was 0.2 μg/l and they used a cutoff of 1.0 μg/l as reference. Interestingly, none of the patients with values between 0.2 μg/l and 1.0 μg/l had MRI-defined necrosis and thus, the study does not rule out the possibility of reversible ischemia in patients with low troponin elevation.
It is well documented that troponin elevation in patients with acute coronary syndromes indicate higher risk The elevation of the cardiac troponins in these patients has been considered to indicate thrombosis and activated platelets as the causative mechanism. The present cohort consisted of low-risk patients with stable angina and thus the lack of predictive value of the troponins might be explained by the absence of thrombotic activity. Furthermore, the molecular size of the biomarkers might be of importance. CK-MB is nearly a three times as large a molecule compared to TnI and TnT is somewhat larger than TnI. CK-MB might be a more appropriate biomarker in stable patients and its release might to a larger degree represent cell death, particularly as compared to TnI which might leak more easily through a damaged cell membrane. Possibly, it is the degree of micronecrosis that predicts subsequent adverse events during follow-up in these stable patients and CK-MB elevation postPCI might to a larger degree than the troponins indicate necrosis at low values. A recent study by Sabatine et al. (Citation21), using an ultrasensitive troponin I assay to assess transient myocardial ischemia in stable patients in response to stress test give some support to the concept of reversible ischemia.
Strength/limitations
In this study we were able to assess the temporal pattern of the biomarkers with certainty up to 20–24 h. In all patients included in the study, normal baseline values were identified and blood samples were also collected immediately after the procedure to make sure that no other factors than the procedure itself influenced the biomarker levels. The results of this study were also strengthened by the very long follow-up time equalising 1600 patient-years. The study was limited by the fact that it was a single-centre study with a relatively small cohort of patients, although the number of patient years was quite high. In the multivariate logistic analysis including variables with univariate p-values < 0.10, the p-value of CK-MB was not significant. However, if systolic blood pressure was used instead of hypertension the p-value was significant. Systolic blood pressure is probably a more precisely defined variable than hypertension which was based on historical data. The measured blood pressure level might reflect the actual risk more accurate in patients being on antihypertensive treatment. Furthermore, in a recent study by us (Citation1) including a somewhat larger number of low-risk patients, the independent prognostic value of CK-MB values ≥ 3 times the reference was significant. Thus, the lower number of patients might also explain the higher P-value of CK-MB in the multivariate logistic analysis in the present study.
The recent guidelines for diagnosing postPCI myocardial infarction2 advocate the use of similar thresholds (3-fold) of CK-MB and the troponins. These recommendations are based on prognostic data as well as expert consensus. Our aim was to assess whether this expert consensus was valid in the present study population and we did not aim to define a diagnostic threshold of myocardial infarction. The exact diagnostic cutoff value might be difficult to define even by use of receiver-operating-characteristic analysis due to biomarker release caused by the procedure itself and also the lack of a precise diagnostic gold standard. In our study none of the patients developed new Q waves after PCI. Furthermore, the most recent troponin assays were not available at the time of inclusion. This will often be so in long-term follow-up studies and might influence the results. However, we have applied these assays in several experimental and clinical studies and the cardiac sensitivity and specificity have been high as compared to CK-MB mass.
In conclusion, this study suggests that in low-risk patients undergoing elective PCI, CK-MB values ≥ 3 times the reference predicts worse outcome during long-term follow-up whatever might have been the cause of the elevation. Importantly, this was not the case for the cardiac troponins. Contrary to the recommendations in the new guidelines for diagnosing MI, CK-MB mass seems more feasible than the cardiac troponins to assess the long-term prognosis in low-risk patients with stable angina undergoing routine angioplasty.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Vikenes K, Melberg T, Farstad M, Nordrehaug JE. Elevated CK-MB values after routine angioplasty predicts worse long-term prognosis in low-risk patients. Scand Cardiovasc J. 2010;44:69–75.
- Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. Eur Heart J. 2007;28;2525–38.
- The joint European Society of Cardiology/American College of Cardiology Committee. Myocardial infarction redefined-A consensus document of the joint European Society of Cardiology/American College of Cardiology committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959–69. doi: 10.1016/S0735-1097(00)00804-4.
- Larue C, Calzolari C, Bertinchant JP, Leclercq F, Grolleau R, Pau B. Cardiac-specific immunoenzymometric assay of troponin I in the early phase of acute myocardial infarction. Clin Chem. 1993;39:972–79.
- Hetland Ø, Gøransson L, Nilsen DWT. Cardiac troponin T immunoassay on biotin-streptavidin-coated microplates: Preliminary performance in acute myocardial infarction. Scand J Clin Lab Invest. 1995;55:701–13.
- Prineas RJ, Crowe RS, Blackburn H. The Minnesota Code manual of electrocardiographic findings. Bristol: John Wright; 1982.
- Nygård O, Nordrehaug JE, Refsum H, Ueland PM, Farstad M, Vollset SE. Plasma homocysteine levels and mortality in patients with coronary artery disease. New Eng J Med. 1997;337:230–36.
- Abdelmeguid AE, Topol EJ, Whitlow PL, Sapp SK, Ellis SG. Significance of mild transient release of creatine kinase-MB fraction after percutaneous coronary interventions. Circulation. 1996;94:1528–36.
- Califf RM, Abdelmeguid AE, Kuntz RE, Popma JJ, Davidson CJ, Cohen EA, . Myonecrosis after revascularization procedures. J Am Coll Cardiol. 1998;31:241–51.
- Ellis SG, Chew D, Chan A, Whitlow PL, Schneider JP, Topol EJ. Death following creatine kinase-MB elevation after coronary intervention: Identification of an early risk period: Importance of creatine kinase-MB level, completeness of revascularization, ventricular function, and probable benefit of statin therapy. Circulation. 2002;106:1205–10.
- Akkerhuis KM, Alexander JH, Tardiff BE, Boersma E, Harrington RA, Lincoff AM, . Minor myocardial damage and prognosis: Are spontaneous and percutaneous coronary intervention-related events different? Circulation. 2002;105: 554–6.
- Roe MT, Mahaffey KW, Kilaru R, Alexander JH, Akkerhuis KM, Simoons ML, . Creatine kinase-MB elevation after percutaneous coronary intervention predicts adverse outcomes in patients with acute coronary syndromes. Eur Heart J. 2004;25:313–21.
- Brener SJ, Lytle BW, Schneider JP, Ellis SG, Topol EJ. Association between CK-MB elevation after percutanous or surgical revascularisation and three-year mortality. J Am Coll Cardiol. 2002;40:1961–7.
- Ionnidis JPA, Karvouni E, Katritsis D. Mortality risk conferred by small elevations of creatine kinase-MB isoenzyme after percutaneous coronary intervention. J Am Coll Cardiol. 2003;42:1406–11.
- Herrmann J. Peri-procedural myocardial injury: 2005 update. Eur Heart J. 2005;26:2493–519.
- Nienhuis MB, Ottervanger JP, Bilo HJG, Dikkeschei BD, Zijlstra F. Prognostic value of troponin after elective percutaneous coronary intervention: A meta-analysis. Catheter Cardiovasc Interv. 2008;71:318–24.
- Nageh T, Sherwood RA, Harris BM, Thomas MR. Prognostic role of cardiac troponin I after percutaneous coronary intervention in stable coronary disease. Heart. 2005; 91:1181–5.
- Nageh T, Sherwood RA, Harris BM, Byrne JA, Thomas MR. Cardiac troponin T and I and creatine kinase-MB as markers of injury and predictors of outcome following percutaneous coronary intervention. Int J Cardiol. 2002;92: 285–93.
- Ricciardi MJ, Wu E, Davidson CJ, Choi KM, Klocke FJ, Bonow RO, . Visualization of discrete microinfarction after percutaneous coronary intervention associated with mild creatine kinase-MB elevation. Circulation. 2001;103:2780–3.
- Selvanayagam JB, Porto I, Channon K, Petersen SE, Francis JM, Neubauer S, . Troponin elevation after percutaneous coronary intervention directly represents the extent of irreversible myocardial injury: Insights from cardiovascular magnetic resonance imaging. Circulation. 2005; 111:1027–32.
- Sabatine MS, Morrow DA, De Lemos JA, Jarolim P, Braunwald E. Detection of acute changes in circulating troponin in the setting of transient stress test-induced myocardial ischaemia using an ultrasensitive assay: Results from TIMI 35. Eur Heart J. 2009;30:162–9.