Abstract
Objectives. To study the effect of aerobic interval training (AIT) on myocardial function in sedentary seniors compared to master athletes (MA) and young controls. Design. Sixteen seniors (72± 1 years, 10 men) performed AIT (4 × 4 minutes) at ∼90% of maximal heart rate three times per week for 12 weeks. Results were compared with 11 male MA (74± 2 years) and 10 young males (23±2 years). Results. Seniors had an impaired diastolic function compared to the young at rest. AIT improved resting diastolic parameters, increased E/A ratio (44%, p <0.01), early diastolic tissue Doppler velocity (e′) (11%, p <0.05) and e′ during exercise (11%, p <0.01), shortened isovolumic relaxation rate (IVRT) (13%, p <0.01). Left ventricle (LV) systolic function (S′) was unaffected at rest, whereas S′ during stress echo increased by 29% (p <0.01). Right ventricle (RV) S′ and RV fractional area change (RFAC) increased (9%, p <0.01, 12%, p =0.01, respectively), but not RV e′. MA had the highest end-diastolic volume, stroke volume, diastolic reserve and RV S′. Conclusion. AIT partly reversed the impaired age related diastolic function in healthy seniors at rest, improved LV diastolic and systolic function during exercise as well as RV S′ at rest.
Introduction
The aging process of the heart, characterized by both systolic and diastolic impairment are related to increased cardiomyocyte loss, increased interstitial fibrosis, loss of arterial elasticity, reduced myocardial metabolic capacity, and decreased maximal heart rate (Citation1). Normal aging affects both left ventricular (LV) relaxation with a prolonged isovolumic relaxation time (IVRT) and deceleration time resulting in reduced early mitral diastolic inflow (E) and increased atrial contribution to late diastolic filling (A) (Citation2,Citation3). Additionally, tissue Doppler imaging that can detect preclinical myocardial dysfunction before conventional measurements show that both systolic tissue Doppler velocity (S′) and early diastolic velocities (e′) are reduced with advancing age (Citation4). The impaired cardiac function is more apparent during physical activity and reveals a reduced myocardial reserve with advancing age (Citation3).
Previous studies indicate that exercise training can influence upon both systolic and diastolic function of the heart, but the evidence whether physical activity can influence age related changes are conflicting (Citation5–8). The reason for this may be due to use of different training protocols as well as echocardiographic techniques in the different studies. Aerobic interval training (AIT) has been shown to have a profound effect to improve cardiac reserve in both healthy subjects (Citation9) and cardiac patients (Citation10). This has not been studied in a healthy aged population.
The hypothesis of the present study was that AIT could reduce the age-related decline in diastolic and systolic cardiac function in both left and right ventricle (RV).
Materials and methods
Study design
The study consists of three parts. First, a cross sectional study where old master athletes (MA) were compared to a group of healthy, sedentary seniors, and to a group of young, sedentary students. Among the MA, we were only able to recruit men, and therefore, the comparison between the three groups was done with males only to avoid gender effects. Secondly, a prospective training intervention was performed in the sedentary seniors, including both men and women, to assess the training effects of short term training in sedentary seniors. Thirdly, a comparison was done between the sedentary males before and after the training intervention to the old MA to assess the training effects of short term versus lifelong training among healthy seniors.
Subjects
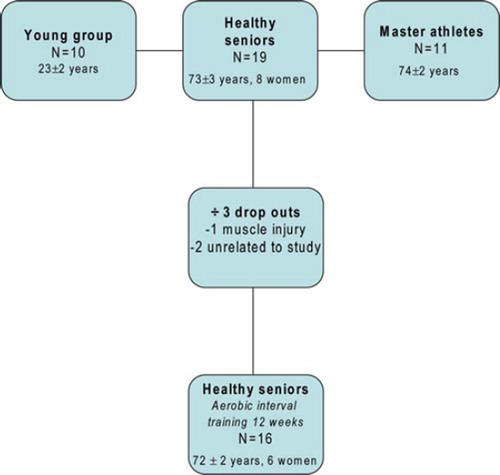
We enrolled 19 persons (73±3 years, 8 women) after an advertisement in a local newspaper (). Inclusion criteria were age >70 years, healthy and not exercising more than twice per week the last year. Persons with chronic illness or chronic use of any medication, regular smoking, or any metabolic or cardiovascular diseases were excluded. All subjects performed a 12-lead ECG at rest and during an individualized graded treadmill test to test maximal oxygen uptake (VO2max). From the university, we recruited 10 (23±2 years) healthy, nonsmoking male students. None of the students had taken part in regular endurance training the previous 2 years. Based on the top 10 results from a national cross-country long distance (54 km) cross-country ski contest (www.birkebeiner.no), 11 male MA (74±2 years) were recruited (from two different subsections, 70–75 years old and from 75 years and older). All of them had exercised regularly (greater than five times per week) the last 25 years and the majority of the participants were still competing at the top national or international level for their age group. They were all still active with an exercise frequency of at least five times per week. The study protocol was approved by the regional committee for medical ethical research, followed the ethic directives according to the Declaration of Helsinki and all subjects gave written informed consent.
Exercise training
The sedentary seniors exercised three times a week at our laboratory, supervised by a personal trainer, for 12 weeks. All training was performed on treadmill as AIT and consisted of 10 minutes warm up at ∼60% of maximal heart rate (HRmax), 4 × 4 minutes intervals at 90–95% of HRmax (corresponding to 85–90% of VO2max) walking/running uphill on a treadmill, with 3 minutes active pause between the exercise bouts at 60–70% HRmax. The session was terminated with 3 minutes cool down. Total exercise time was 38 minutes. Criterion for completing the study was a 90% compliance with the training program. Training intensity was controlled by heart rate monitors (Polar Electro, Kempele, Finland). All patients were encouraged to maintain their usual diet.
Exercise testing, VO2max
VO2max was tested using a standardized graded ramp protocol on a treadmill (Woodway, Sport 5000 PS) (Citation11). After a 10-minutes warm-up, a facemask was placed on the subjects face for metabolic measurements using a Metamax 2 (Cortex, Leipzig, Germany). Incline was constant at 10% and band speed increased every minute until VO2 leveled off (<2 ml/kg/min increase) despite increased work load was reached and a respiratory exchange ratio >1.10.
The sedentary seniors were tested twice, at baseline and follow up. The MA and the young male controls were only tested once.
Echocardiography
The subjects were examined by an experienced cardiologist using Vivid 7 scanner (GE Vingmed Ultrasound, Horten, Norway) with a phased array M3S matrix probe. Measurements obtained in this study are in accordance to standard procedures recommended by the American Society of Echocardiography (Citation12). Data was analyzed blinded both to subject and time point. B-mode images were recorded with a frame rate of 53 frames per second. LV volumes and ejection fraction (EF) were calculated from apical four- and two-chamber recordings by modified biplane Simpson's method. LV inflow velocity was measured by pulsed Doppler with the sample volume at the tips level of mitral valves. Measurements included early diastolic filling (E), late diastolic filling (A), and isovolumic relaxation time (IVRT). Stroke volume (SV) was calculated from Doppler flow velocity integral in the LV outflow tract (LVOT) and LVOT diameter. Pulsed tissue Doppler recordings from the mitral annulus were obtained from the septal and lateral points in four-chamber and in the anterior and inferior points in two-chamber views, as well as from the lateral corner of the tricuspid annulus. Peak annulus velocity in systole (S′), early diastole (e′), and late diastole (a′) were measured as average of the four points for the LV. Right ventricular fractional area change (RFAC) was measured in four-chamber view, and calculated as the difference between the RV area in diastole and systole as percentage of end-diastolic RV area. Left atrial (LA) volume was calculated by the squared area of LA, four-chamber, in end systole, multiplied with 0.85.
Blood pressures were measured before and after the intervention. Measurements were done at rest in office according to standard procedures (Citation13).
Stress echocardiography
Echocardiography was performed sitting forward on a stationary bike at rest and after 2 minutes of a workload of 70% of HRmax. The sedentary seniors were tested before and after intervention at 70% of HRmax. Pulsed Doppler flow velocity recordings from four-chamber view and color tissue Doppler recordings were obtained from four-chamber and two-chamber view. The other two groups were tested only at baseline. Measurements at rest included E, A, stroke volume, and cardiac output and during stress e′ (e′submax) and S′ (S′submax). Mean values from all four points were used in the analysis. All patients had a fusion of early and late diastole tissue velocities at submaximal heart rate. Blood pressure was measured at rest, lying on bench and sitting upfront on bike at rest, and at submaximal exercise on bike.
Statistical analysis
Data are presented as ± SD. One-way analysis of variance, Bonferroni corrected, was used to detect differences between the male groups. The second main analysis included both genders using students paired t-test, to discover within group differences of the intervention effect. Correlations between changes in parameters after training were calculated by Pearson's correlation coefficient.
Results
Subjects
A total of 16 subjects among the seniors (72±2 years, 6 women) completed the training (). One subject dropped out due to muscle injury and two for reasons unrelated to the study. A reduction in weight and body mass index was observed among the seniors by 1.2±1.8 kg, (p =0.02) and 0.41±0.65 kg/m2 (p =0.03), respectively ().
Table II Effect of intervention, both genders.
VO2max, resting heart rate and blood pressures
At baseline, VO2max among the senior males was 60% (p <0.01) and 44% (p =0.02) lower compared to the young males and MA, respectively (). AIT increased VO2max by 15% (p <0.01) among the seniors ().
Table I Baseline measurements, cross sectional analysis, males only.
Resting heart rate was 18% higher among seniors vs. young at baseline (p =0.05). MA had significantly lower resting heart rate (66 versus 53 beats/minute, p <0.01) compared to baseline values among senior males (). There was no difference in resting heart rate between young males and MA (p =0.99). AIT reduced resting heart rate by 10 beats per minute (p <0.01) among the seniors ().
At baseline the seniors had a higher systolic and diastolic blood pressure compared to the two other groups (p <0.01 and p =0.04) (). Among the seniors, AIT reduced systolic and diastolic blood pressure with 12% and 9%, respectively (p <0.01) ().
Cardiac volumes
Compared to the senior males at baseline, young males and MA had higher end diastolic volume (EDV) (33% and 39% respectively; group differences NS) and SV (8% and 29% respectively; group difference, NS) (). Senior males had 32% (p <0.01) smaller left atrial size compared to MA (). Cardiac output was similar between groups at all time points.
AIT increased EDV by 17% among the seniors (p <0.01 () (both genders), and 22% among the senior males (). Stroke volume increased by 10% (p <0.05) after the training period among the seniors (both genders and senior males) ( and ). Left atrial volume and cardiac output was unchanged after the intervention period.
Table III. Echocardiographic measurements, effect of intervention (both genders).
Table IV. Effect of intervention, comparison seniors- versus master athletes (only males).
Diastolic and systolic function
At baseline, MA and senior males had a similar E, which was markedly lower than observed among the young males (0.82 m/s vs. 0.58 m/s, p <0.01) (). E/A ratio was similar in MA and senior males, and MA had 61% lower compared to the young males (2.4 vs. 1.33, p <0.01) (). IVRT was similar at baseline among MA and senior males (110.0 ms versus 98.0 ms, p =0.21) and was significantly longer compared to the young males (73.0 ms, seniors p <0.01, MA p =0.02) (). Among the senior males, e′ was 66% lower compared to the young males (p <0.01) and a trend 23% lower compared to the MA (p =0.08)(). S′, among the senior males was 12% lower than the MA (p =0.40) and by 26% compared to the young males (p =0.01) (). EDV was correlated to IVRT and e′ (0.69, p <0.01 and‐0.67, p <0.01, respectively).
AIT improved all resting diastolic parameters among the seniors with an increased E (12.5%, p <0.05) and decreased A (25.6%, p <0.01), and hence, an increased E/A ratio (44%, p <0.01), a shortened IVRT (13%, p <0.01), an increased e′ (11%, p <0.05), and decreased a′ (12%, p <0.01) (). There was no effect of the intervention on LV S′ at rest among the seniors.
RV S′ and e′ was higher among the MA compared to the senior males (), but no difference in a′ was observed (17.3±3.5 cm/s vs. 15.7±5.8 cm/s respectively, p =0.48). RV S′, but note, ′ increased after intervention (). There was no difference in RV S′ among the seniors and the young at baseline (11.8±2.1 cm/s vs. 12.7±1.7 cm/s respectively, p =0.88) RV S′ increased after the intervention by 9.9% (p <0.05) (). RVFAC increased after intervention among the seniors by 12% (p <0.01) (). RV e′ were significantly higher and a′ significantly lower among the young at baseline. There was no training effect on RV e′ among the seniors.
Submaximal stress echocardiography test
The MA had the largest stroke volume during submaximal exercise at baseline compared to the senior males (p <0.01), and this was still present at follow-up (p =0.02) (). Stroke volume during submaximal exercise increased significantly among the seniors (p <0.01)().
S′submax was 41% higher among the MA at baseline compared to the senior males (p <0.01), whereas AIT increased S′submax by 29% to similar level as MA (p =0.18) ().
There was no difference in e′submax between the senior males and the young males (p =0.20) (). MA had a trend towards 16% higher e′submax than the senior males at baseline, (p =0.07) (), whereas no difference were seen between the MA and the young males. AIT increased e′submax by 11% (p <0.01) among the seniors ().
Discussion
The main findings in the present study were that (Citation1); healthy seniors had a lower longitudinal systolic function compared to young, (Citation2) only 12 weeks of AIT improved diastolic function at rest and both systolic and diastolic exercise reserve among healthy seniors (Citation3) lifelong training increases LV volumes and diastolic reserve capacity comparable to young sedentary people.
VO2max, resting heart rate
This study demonstrated that healthy seniors adapted to exercise and improved their aerobic capacity to the same extend as seen in younger subjects, confirming previous findings (Citation8). The reduction in resting heart rate may be considered equivalent to an increase in heart rate reserve, which may be important as maximal heart rate declines with age.
Cardiac volumes
Sedentary seniors had smaller LV volumes than young persons, and this might be considered a result of atrophy. Nevertheless, AIT increased both EDV and SV and may reflect eccentric remodeling, which may indicate that smaller volumes among sedentary seniors are largely a result of inactivity. It may be reversed by AIT, although short term intervention did not seem to be sufficient compared to the MA. The atria were larger in MA, but the relation between left atrial and ventricular size were the same in both groups, and were also proportionally similar between seniors and MA. This suggests atrial enlargement to be rather a symmetric training adaption than a specific atrial “overload” effect. However, in this study we observed no effect on atrial size after training in the seniors.
Diastolic function
Lifelong physical exercise could not compensate the E/A ratio as the young subjects had a higher value compared to the MA. However, there was probably a positive effect of training, indicated by the difference between the MA and the sedentary seniors. This was further supported by the comparison of deceleration time and IVRT as well.
Although debated, e′ has been found to be a less load dependent measurement of early diastolic function compared to traditional echocardiographic measurements (Citation14). In our study, e′ increased among the senior males after the training intervention to the same level as observed in MA. The young group had a superior relaxation with a higher e′ at rest at any time of measurement compared to the two other groups. This indicates that LV relaxation declines with age despite lifelong training, although some of the reduction seen in older cohorts is due to inactivity and can be reversed by short-term high intensity exercise. The effect may in part be explained by changes in preload, afterload and heart rate (Citation14–16). Although, we did not measure plasma volume, other studies have demonstrated increased plasma volume in healthy subjects after a training period (Citation15), which may have increased preload and affected the echocardiographic measurements in our study. Systolic BP decreased during the training period and thus reduced the afterload among the seniors. A reduced afterload elicits a lesser resistance for the LV to contract, causing faster recoil and a greater diastolic suction. EDV was correlated to both e′ and IVRT demonstrating concomitant training adaptions involving mechanisms related to preload, afterload and contractility. However, the changes may be parallel, and not causally related. Heart rate has a significant influence on the traditional diastolic flow markers and may be partly responsible for the increased E/A ratio of the mitral flow (Citation16). Although e′ has shown to be less dependent by HR (Citation17), a recent study suggest that e′ is also affected by HR (Citation18).
The myocardial static compliance is determined by the relation of the relatively compliant cardiac muscle and the less compliant extracellular matrix and connective tissue. Levine and colleagues found increased e′ and increased compliance among fit elderly subjects compared to their sedentary counterparts (Citation19). In addition, they demonstrated a modest increase in LV relaxation after one year of training, although no increase in e′ and LV compliance (Citation20). Our findings correspond to their findings, but we also demonstrate that short term intensive exercise improves diastolic function almost to the same level as lifelong endurance training. Our study differed somewhat to their study. Our subjects had a much higher VO2max at baseline, and after the training period they achieved values of VO2max corresponding to the same level as their old MA. In addition, our subjects exercised at higher intensities for longer periods. Further studies are required to elucidate the mechanisms of the improved diastolic function.
Systolic function
Stroke volume at rest was higher among the young subjects and the MA, in relation to the higher end diastolic volume and lower heart rate. The RV has been less studied among athletes, and considered having a relatively passive role. RV function has been a larger challenge for echocardiographic evaluation compared to LV function, due to the anatomic location. However, tissue Doppler has become a reliable and easy tool to evaluate RV function (Citation21), which is an important predictor of exercise capacity and mortality in patients with heart failure (Citation22). We found that the MA had a better RV systolic and diastolic function compared to the senior males. Enhanced RV function has not, to our knowledge, been shown before in elderly MA. On the contrary, Teske et al. found no difference in RV diastolic function in aged athletes’ and nonathletic's hearts (Citation23). However, their study was limited by not measuring VO2max to verify the actual fitness level. Biventricular adaptations to training in our senior population differed with a mainly systolic improvement of RV and both systolic and diastolic improvements of LV. The exercise effect on the RV in our seniors has to be analyzed with caution due to its load dependency.
Submaximal exercise
The adaptations to exercise in terms of systolic and diastolic reserve are shown in submaximal exercise measurements. Stroke volume is the most trainable cardiac parameter to increase VO2max (Citation24) as maximal heart rate is less affected by fitness level (Citation25). The stroke volume is a compound of both LV volumes, systolic and diastolic functional reserve. Results should also be interpreted with caution, as HR during exercise was lower in the MA group, than in the two other groups.
At baseline, e′submax was highest in the MA. The seniors increased e′submax, indicating that the diastolic exercise reserve is trainable in older years. The diastolic function during stress was improved. However, it is not possible to elucidate the exact mechanism as e′ and A′ had a fusion. The improvement in the diastolic reserve may thus not be only a result of increased early relaxation, but can partly be influenced by increased plasma volume, reduced afterload and a higher LV compliance due to a less stiff ventricle (Citation7,Citation15,Citation19).
Systolic exercise capacity indicated by S′ increased among the senior males and no difference was observed after intervention compared to MA. These findings indicate that systolic reserve decreases with age, but that it's highly susceptible to respond to endurance exercise. This correspond to other studies confirming that older people profit by exercise training by improving the systolic cardiac reserve (Citation26), which might be the most important cardiac improvement of endurance training for elderly.
Limitations and strengths
The main limitation in this study is the small numbers of participants and therefore some of the p values border significant. The cross sectional study is limited as no conclusions on causality can be drawn. However, this is supplemented by the exercise effects in the interventional part. The MA and students consisted of males only, and thus the comparison with follow-up results was limited. We did no invasive measurements to study different loading conditions, which may have been changed during the training period. Strength of the study is the well-controlled and highly defined exercise intensity intervention regime. The MA had a higher VO2max compared to many other studies.
Conclusions
This study demonstrates that short term AIT significantly improve LV diastolic function at rest in sedentary seniors. In addition, short term intensive training improved LV diastolic and systolic function during exercise and systolic function of the RV at rest.
Acknowledgements
CBI is recipient of research grant from the Norwegian Research Council, through the center for research based innovation, MI-Lab, Trondheim, Norway. The study was supported by grants from the Norwegian University of Science and Technology (CBI), Norwegian Council on Cardiovascular Disease and Norwegian Research Council Funding for Outstanding Young Investigators (UW) and Foundation for Cardiovascular Research at St. Olav's Hospital (AS, UW), K.G. Jebsen Foundation (UW) and by EXTRA funds from the Norwegian Foundation for Health and Rehabilitation and The Norwegian Heart and Lung Patient Organization.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Klausner SC, Schwartz AB. The aging heart. Clin Geriatr Med. 1985;1:119–41. Epub 1985/02/01.
- Bryg RJ, Williams GA, Labovitz AJ. Effect of aging on left ventricular diastolic filling in normal subjects. Am J Cardiol. 1987;59:971–4. Epub 1987/04/15.
- Schulman SP, Lakatta EG, Fleg JL, Lakatta L, Becker LC, Gerstenblith G, . Age-related decline in left ventricular filling at rest and exercise. Am J Physiol. 1992;263:H1932– 8. Epub 1992/12/01.
- Innelli P, Sanchez R, Marra F, Esposito R, Galderisi M. The impact of aging on left ventricular longitudinal function in healthy subjects: a pulsed tissue Doppler study. Eur J Echocardiogr. 2008;9:241–9.
- Levy WC, Cerqueira MD, Abrass IB, Schwartz RS, Stratton JR. Endurance exercise training augments diastolic filling at rest and during exercise in healthy young and older men. Circulation. 1993;88:116–26 Epub 1993/07/01.
- Fleg JL, Shapiro EP, O’Connor F, Taube J, Goldberg AP, Lakatta EG, . Left ventricular diastolic filling performance in older male athletes. JAMA. 1995;273:1371–5. Epub 1995/05/03.
- Arbab-Zadeh A, Dijk E, Prasad A, Fu Q, Torres P, Zhang R, . Effect of aging and physical activity on left ventricular compliance. Circulation. 2004;110:1799–805. Epub 2004/09/15.
- Stratton JR, Levy WC, Cerqueira MD, Schwartz RS, Abrass IB. Cardiovascular responses to exercise. Effects of aging and exercise training in healthy men. Circulation. 1994;89:1648–55. Epub 1994/04/01.
- Helgerud J, Hoydal K, Wang E, Karlsen T, Berg P, Bjerkaas M, . Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc. 2007;39:665–71. Epub 2007/04/07.
- Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, . Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115:3086–94. Epub 2007/06/06.
- Wolthuis RA, Froelicher VF, Jr., Fischer J, Triebwasser JH. The response of healthy men to treadmill exercise. Circulation. 1977;55:153–7. Epub 1977/01/01.
- Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, . Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63. Epub 2005/12/27.
- Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, . European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2007;14 Suppl 2:S1–113. Epub 2007/11/06.
- Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, . Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: A comparative simultaneous Doppler-catheterization study. Circulation. 2000;102: 1788–94. Epub 2000/10/12.
- Hagberg JM, Goldberg AP, Lakatta L, O’Connor FC, Becker LC, Lakatta EG, . Expanded blood volumes contribute to the increased cardiovascular performance of endurance-trained older men. J Appl Physiol. 1998;85:484–9. Epub 1998/08/04.
- Galderisi M, Benjamin EJ, Evans JC, D’Agostino RB, Fuller DL, Lehman B, . Impact of heart rate and PR interval on Doppler indexes of left ventricular diastolic filling in an elderly cohort (the Framingham Heart Study). Am J Cardiol. 1993;72:1183–7. Epub 1993/11/15.
- Yu CM, Lin H, Ho PC, Yang H. Assessment of left and right ventricular systolic and diastolic synchronicity in normal subjects by tissue Doppler echocardiography and the effects of age and heart rate. Echocardiography. 2003;20:19–27. Epub 2003/07/10.
- Burns AT, Connelly KA, La Gerche A, Mooney DJ, Chan J, MacIsaac AI, . Effect of heart rate on tissue Doppler measures of diastolic function. Echocardiography. 2007;24: 697–701. Epub 2007/07/27.
- Prasad A, Popovic ZB, Arbab-Zadeh A, Fu Q, Palmer D, Dijk E, . The Effects of Aging and Physical Activity on Doppler Measures of Diastolic Function. Am J Cardiol. 2007;99:1629–36.
- Fujimoto N, Prasad A, Hastings JL, Arbab-Zadeh A, Bhella PS, Shibata S, . Cardiovascular effects of 1 year of progressive and vigorous exercise training in previously sedentary individuals older than 65 years of age. Circulation. 2010;122:1797–805. Epub 2010/10/20.
- Innelli P, Esposito R, Olibet M, Nistri S, Galderisi M. The impact of ageing on right ventricular longitudinal function in healthy subjects: a pulsed tissue Doppler study. Eur J Echocardiogr. 2009;10:491–8. Epub 2008/12/17.
- de Groote P, Millaire A, Foucher-Hossein C, Nugue O, Marchandise X, Ducloux G, . Right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure. J Am Coll Cardiol. 1998;32: 948–54.
- Teske AJ, Prakken NH, De Boeck BWL, Velthuis BK, Doevendans PA, Cramer MJM, . Effect of Long Term and Intensive Endurance Training in Athletes on the Age Related Decline in Left and Right Ventricular Diastolic Function as Assessed by Doppler Echocardiography. Am J Cardiol. 2009;104:1145–51.
- Levine BD. VO2max: what do we know, and what do we still need to know? J Physiol. 2008;586:25–34. Epub 2007/11/17.
- Ogawa T, Spina RJ, Martin WH, 3rd, Kohrt WM, Schechtman KB, Holloszy JO, . Effects of aging, sex, and physical training on cardiovascular responses to exercise. Circulation. 1992;86:494–503. Epub 1992/08/01.
- Ehsani AA, Ogawa T, Miller TR, Spina RJ, Jilka SM. Exercise training improves left ventricular systolic function in older men. Circulation. 1991;83:96–103. Epub 1991/01/01.