Abstract
Objectives. Complement activation as evidenced by C4d deposition indicates immunological tissue reactivity. We sought to study the vascular reactivity of the aortic wall by characterizing C4d deposits. Design. Aortic wall histology and immunohistochemistry for C4d, leukocytes, T- and B-lymphocytes, plasma cells, macrophages, endothelial cells, smooth muscle cells, cell proliferation, elastase, and Van–Gieson-staining were performed to 91 consecutive patients that underwent surgery for ascending aorta, and the samples were grouped according to presence of C4d deposits. Results. Fifty-three out of 91 patients had C4d deposits mainly within the adventitia (C4d +), whereas 38 patients lacked C4d deposits (C4d−) including decreased staining of intra-aortic vessels (p < 0.005). Intimal thickness and cellularity, together with inflammation consisting of plasma cells were increased in C4d‐ as compared with C4d + (p < 0.05). Receiver operating characteristic curve (ROC) analysis showed that C4d was associated with stabile nondissecting ascending aorta (AUC 0.792; SE 0.053; p = 0.000; 95% CI 0.688–0.895), but not with presence of aortitis per se (AUC 0.523; SE 0.069; p = 0.752; 95 % CI 0.388–0.658). Conclusions. Lack of C4d may indicate active remodeling of the aortic wall leading to aortic dissection (AD). Immunologic complement factors may be amenable to diagnosis of instability after aortic surgery.
Key words::
Introduction
Prompt surgery is required for ascending aortic dilatation (AA) prone to rupture to prevent life-threatening aortic dissection (AD) (Citation1). While an arbitrary border-line of 5-cm enlargement of the diameter of the ascending aorta has been shown to increase the risk for AD, there is increasing awareness that aortic remodeling and subsequent AD may occur at an earlier stage of AA occasionally with aorta diameters less than 4.5 cm (Citation1). Risk for AD may be associated with different molecular mechanisms of the aortic wall as compared with AA alone (Citation2,Citation3). AD is considered to initiate from a sudden tear in the aortic wall endothelium due to decreased resiliency (Citation4). The origin may occur in the vasa vasorum of the aortic wall, which leads to intramural hematoma that induces subsequent AD (Citation5).
Increasing evidence suggest that complement factors are involved during inflammatory remodeling of the arterial wall (Citation6). Significant amounts of complement components are found in atherosclerotic lesions compared to healthy arteries (Citation6,Citation7). Increased amounts of complement end products are associated with development of intracranial saccular aneurysms (Citation8). Pathogenesis of aortic valve stenosis (Citation7) and experimental aortic dilatation (Citation9) have been associated with complement activity. These findings may implement that complements play a crucial role in the extension of chronic lesion formation devoid of arterial wall rupture.
We hypothesized that the complement cascade is present during AA and AD indicating aortic wall remodeling. In this study, we define aortic wall remodeling as histologically confirmed aortic wall changes during AA and AD.
Materials and methods
Study protocol and surgery
After IRB approval, ascending aortic wall resection of 102 consecutive patients undergoing surgery for ascending aorta was obtained and processed for histology. AA was preoperatively confirmed and evaluated with computer tomography (CT). According to our institutional policy, AA included aortic diameter more than 5.5 cm wide or aortic growth more than 1 cm in a year. This definition was adjusted to presence of Marfan syndrome, gender, patient size, and symptoms including AD according to The Yale Center criteria (Citation10). Surgery was performed between December 2006 and August 2009 in the Heart Center of Tampere University Hospital, and all cases of AA including AD processed for histology were enrolled. The samples of 11 patients were excluded due to technical failure during preparation of the samples.
Decision on the extension of resection and surgical technique was at the discretion of the operating surgeon. When AA including the sinotubular junction (STJ) was estimated as the reason for aortic regurgitation, STJ was tailored for a suitable graft in a supracoronary fashion. Whenever dilatation included the aorta root, a radical resection of the dilated ascending aorta together with the root and the aortic valve was performed in all but four patients, in whom a David-type valve-sparing operation was achieved. The graft size was estimated by the principal surgeon. Resection of the aortic arch was carried out depending on extension of distal aortic dilatation. Since the surgical procedure was performed upon surgical decision, the sample was procured from the middle of the resected diseased area of the ascending aorta at the vicinity of STJ.
Histology and immunochemistry
Two to five blocks of resected ascending aorta were embedded in paraffin and cut to 4-μm-thick segments and stained with hematoxylin and eosin (H&E), Verhoeff-van Gieson (VVG), elastase-van Gieson (EVG) and periodic acid-Schiff (PAS). A representative 1-cm-long piece of ascending aortic wall corresponding to all different staining was evaluated systematically for all resected samples procured during surgery. The heights of different layers (adventitia, media, and intima) were calculated for each sample. Inflammatory cells, intensity of inflammation, medial degeneration, intima cellularity, and thickness were estimated as previously described and expressed as point score units (PSU) (Citation2).
Immunohistochemistry was performed using Ventana Lifesciences Benchmark XT© Staining module. Vasa vasorum were evaluated using Polyclonal Rabbit antibody for Von Willebrand factor (dilution 1:2500) (DakoCymation). Lymphatic vessels were evaluated using Podoplanin (dilution 1:50) (Angiobio Co.) and monoclonal mouse antibody D2 - 40 (dilution 1:50) (DakoCymation) (Citation11, Citation12). C4d (dilution 1:50) (Biomedica Gruppe) was stained for slides, accordingly. Ventana Lifesciences Antibody Dilution Buffer© was utilized for dilution media.
Statistical analysis
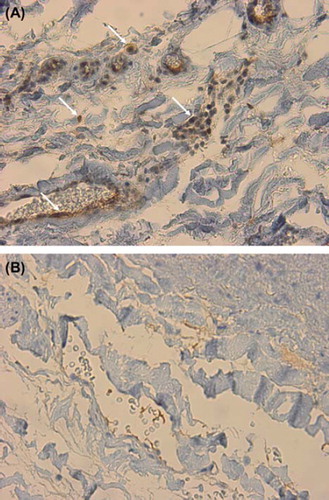
C4d + staining was predominantly found in the adventitia, at the border of the media including endothelial cell lining of small vessels (). In order to seek for clinical relevance associated with histology, the patients were divided into two groups according to presence of C4d staining of small vessels of the aortic wall. Patients with C4d + staining of the ascending aortic wall were referred as C4d +, and those without C4d staining as C4d‐Φ Quantitative variables are listed as mean and standard error of the mean. Categorical variables are stated as count and percentage. Statistical analysis was performed with SPSS version 19.0. Mann–Whitney-test was used for continuous variables and chi-square-test for categorical analysis. The predictive value of C4d to identify AD among patients with AA only was assessed by receiver operating characteristic curve (ROC) analysis. P-values less than 0.05 were considered statistically relevant.
Results
Patient characteristics ()
There were twice as many male than female in the study. The study population consisted of 61 male and 30 female. Mean age for the patients was 62 ± 13 years. Hypertension was diagnosed in only 28 patients, and no difference in its prevalence between the groups was found. There were seven patients (8%) with Marfan syndrome, of whom the majority had C4d positivity. The one patient with a nonspecific vasculitis in our study group was also C4d +. The frequency of preoperative inflammatory state, such as myositis and arthritis, showed no difference between the groups. The mean diameter of the ascending aorta at the sinotubular junction was 57 ± 9 mm for all patients. Interestingly, moderate to severe aortic valve stenosis (AVS) was found to be more frequent in C4d + group with 21 patients (40%) in contrast to 7 patients (19%) with C4d negativity, whereas aortic valve insufficiency (AVI) was equally present among the groups. The majority of the patients had tricuspid aortic valve. Ten patients with C4d positivity and 4 patients with C4d negativity underwent a previous cardiothoracic operation.
Table I. Patient demographics.
Operative technique ()
Graft replacement for the ascending aorta was performed either with root replacement (in 52 patients), or without encompassing the root (in 39 patients). The extension of root dilatation together with dilatation of the ascending aorta from STJ was remarkably equally distributed among the patients in both groups being 57% and 58% in C4d + and C4d −, respectively. A valve-sparing operation David operation was offered for four patients. Concomitant coronary artery bypass grafting was required to 12 patients.
Table II. Operative details according to surgical evaluation of extension of diseased aorta.
Perioperative findings, histology and immunohistochemistry ( and )
Confirmed by histology, the aorta had acute or chronic dissection in 17 out of 38 patients (45%) with C4d − staining of the aorta. In contrast, only one patient had acute and three patients had chronic dissection in the group with C4d positivity (11%). Though dissection was undeniably diagnosed histologically, in six patients (five with C4d positivity and one with C4d negativity), the adventitia was difficult to evaluate for every inflammatory cells in every sample block due to blood stains and artifact. Altogether, 13 patients with C4d positivity and 6 patients with C4d negativity had histological findings of aortitis. Four patients died immediately, including 3 patients with AD and C4d negativity. In contrast, only one C4d + patient with a history of previous coronary artery bypass operation died due to perioperative heart failure.
Table III. Histology and quantitative immunohistochemistry.
Table IV. Immediate postoperative outcome.
In C4d − aortas, vasa vasorum small vessels of the adventitia, as detected by vWF density, were decreased in number as compared with C4d + aortas (p <0.0001). Also, small lymphatic vessels were less numerous in C4d − group as observed with D2-40 and podoplanin stainings and compared with C4d + aortas (p <0.003 and p <0.004, respectively). The intima did not show any positivity of C4d, and C4d + vessels were observed in the media only whenever they were present in the adventitia. Intimal thickness and cellularity were increased in C4d − aortas (2.1±0.9 PSU and 1.9±0.7 PSU, respectively) as compared with C4d + aortas (1.7±0.9 PSU and 1.5±0.7 PSU, respectively), mostly owing to presence of inflammatory plasma cells in the intima (p <0.05).
ROC curve analysis ()
The predictive value of C4d + staining to identify AD from operated AA only was assessed by ROC analysis. C4d staining was significantly associated with nondissecting AA (AUC 0.792; SE 0.053; p =0.000; 95% CI 0.688–0.895), but not with histologically identified ascending aortitis per se (AUC 0.523; SE 0.069; p =0.752; 95% CI 0.388–0.658).
Figure 2. Receiver operating characteristic curve (ROC) analysis of C4d associated with stabile nondissecting ascending aortic dilatation (A) and histologically defined aortitis (B). C4d is significantly associated with the prevalence of nondissecting ascending aortic dilatation (AUC 0.792; SE 0.053; p = 0.000; 95% CI 0.688–0.895, A), but not with aortitis (AUC 0.523; SE 0.069; p = 0.752; 95 % CI 0.388–0.658, B).
Discussion
In this study, C4d positivity was frequently present in patients who underwent surgery for ascending aorta. Patients with AA without AD showed clear C4d deposition indicating aortic wall remodeling associated with complement activation. Instead, C4d deposition was predominantly lacking in patients with AD.
The majority of the patients in our study were male, in whom hypertension was well-controlled. The extension of aortic dilatation, for example, to the root was not predictable by aortic wall C4d positivity. Histopathology revealed significant aortitis in 19 patients, of whom 7 had Marfan syndrome. Neither aortitis nor previous thoracic operation was statistically associated with either C4d positivity or negativity. C4d complement deposition was present during remodeling phase of the aortic wall without major aortic inflammation or intimal reactivity. According to ROC curve, C4d deposition predicted AA, but not aortitis. Activation of complement reaction has been proposed as an initiator of lesion formation, as modified lipoproteins initiate complement cascade in in vitro models (Citation13). While the ascending aorta is relatively rarely affected with atherosclerosis as compared with the descending aorta, presumably due to embryological differences of the sites of the aorta (Citation14), clinical observations approve for a protective nonactive aortic wall against AD during the degenerative AA (Citation6,Citation9).
Frequently, C4d depositions were devoid in patients with AD, while an important decreased number of adventitial lymphatic and vasa vasorum vessels together with inflammatory plasma cell infiltration in the intima were observed. The main difference in pathogenesis between AA and AD may be associated with vasa vasorum. Disturbances in media and adventitia vasa vasorum induce remodeling of the whole arterial wall (Citation5). Rupture of aortic wall vasa vasorum vessels cause intramural hematoma, which eventually affects the integrity of aortic wall and leads to AD (Citation5). It is tempting to suggest that lack of C4d deposition is associated with changes of complement activation of the aorta during AD.
This study also revealed aortic disease undetected clinically before surgery. As stated above, diagnosis for AD was always confirmed by histology. Meticulous and systematic histopathological analysis was performed for all samples (), and included widely acknowledged immunohistochemical methods to evaluate inflammatory cells. We acknowledge the challenge for the resection to include impeccably all three layers of aortic wall during AD; indeed, though AD was undeniably diagnosed histologically, the adventitia was difficult to evaluate for every inflammatory cells in every sample block due to blood stains and arterfact in six patients. We did not, however, exclude these patients, since statistical analysis was not confounded with or without these patients. Interestingly, immediate death occurred in four patients, including three with C4d negativity. All these three had AD, while only one C4d + patient with a history of previous coronary artery bypass operation died but only due to perioperative heart failure. Obviously, it is too early to associate early mortality with histology of the aortic wall, least to mention with C4d negativity, and subsequent follow-up of our patients is warranted.
To our best of knowledge, the association of complement factors has not been studied earlier during AA and AD. Complement factors are ubiquitous molecules, which are produced mainly in the liver, though some local production is observed during target tissue inflammation (Citation15). Complement cascade has been proved to play an important role in cardiovascular diseases (Citation13,Citation16). Intracranial saccular aneurysms show increased complement activation (Citation8). The protective ability of complement activation may involve solubilization and degradation of cell debris and apoptotic cells that are proinflammatory by nature (Citation17). A study using rats devoid of complements showed that experimental arterial lesions consisted of increased number of apoptotic cells as compared with control rats owing intact classical complement pathways (Citation18). C4d positivity may therefore indicate vascular wall stiffness through a mechanism initiated within the adventitia (Citation6). Vascular wall stiffness is tentatively defined as increased aortic wall degeneration related to atherosclerosis (Citation6). Instead of a traditional “inside-out” theory of intima endothelial cell activation and subsequent aortitis, a potential “outside-in” mechanism of vascular stiffness during periadventitial activation of inflammatory adipose tissue may produce C4d deposition that bind to collagen and elastin fibers through covalent thiolester bonds leading to increased aorta wall stiffness (Citation6). End products of complements, such as C5b-9, are prominent during atherosclerosis and aortic valve stenosis (Citation19). Interestingly, 21 out of 53 patients (40%) with C4d aortic wall deposition and thus AA had also moderate to severe aortic valve stenosis, in contrast to 7 out of 38 patients (19%) without C4d aortic wall deposition. It remains to be investigated whether presence of important aortic valve stenosis and C4d aortic wall deposition are both associated with AA but not with AD.
A protective role of complements has previously been associated with the classical complement pathway (Citation14). As C4d is the end product for classical and lectin pathways, the activation mechanics for C4d cannot be further differentiated (Citation16,Citation20). The complement activation of the alternative pathway may also be involved (Citation20). To date, there has not been found any physiological role or receptor for C4d, but it is considered a remnant of C4b. On the other hand, complement activation may be associated with different complements than C4d. It is unfortunately beyond the scope of this study to further differentiate different complement pathways associated with AA and AD. Again, our study group is relatively small and postoperative follow-up includes only c.a. 1 year. However, as presence of complement C4d deposition seems beneficial for the integrity of aortic wall during AA, further investigation on complement activation associated with aortic remodeling is much appreciated based on this systematic pilot analysis.
Taken together, immunologic complement factors may be amenable to follow-up after surgery for AA. Since C4d is the end product of complement reaction and has a relatively long half-life due to its ability to form covalent bindings among other molecules, we speculate whether evaluation of presence of C4d deposition via immunohistochemistry enables one to identify aortic wall prone to AD. It remains to be investigated whether intervening with complement cascade may add an armament against AD.
Acknowledgements
This study was supported by research funding from The Competitive Research Foundation of Tampere University Hospital (Grant 9L058), Tuberculosis Foundation, The Finnish Heart Association and The Finnish Cultural Foundation. Dr A Mennander is the recipient of the Ingegeerd and Viking O Bjork award for Scandinavian Cardiovascular Research.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Narayan P, Rogers CA, Davies I, Angelini GD, Bryan AJ. Type A aortic dissection: has surgical outcome improved with time? J Thorac Cardiovasc Surg. 2008;136:1172–7.
- Levula M, Paavonen T, Valo T, Pelto-Huikko M, Laaksonen R, Kahonen M, . A disintegrin and metalloprotease-8 and -15 and susceptibility for ascending aortic dissection. Scand J Clin Lab Invest. 2011;71:515–22.
- He R, Guo DC, Estrera AL, Safi HJ, Huynh TT, Yin Z, . Characterization of the inflammatory and apoptotic cells in the aortas of patients with ascending thoracic aortic aneurysms and dissections. J Thorac Cardiovasc Surg. 2006;131:671–8.
- Wilson WR, Anderton M, Schwalbe EC, Jones JL, Furness PN, Bell PR, . Matrix metalloproteinase-8 and -9 are increased at the site of abdominal aortic aneurysm rupture. Circulation. 2006;113:438–45.
- Marcus ML, Heistad DD, Armstrong ML, Abboud FM. Effects of chronic hypertension on vasa vasorum in the thoracic aorta. Cardiovasc Res. 1985;19:777–81.
- Shields KJ, Stolz D, Watkins SC, Ahearn J. Complement proteins C3 and C4 bind to collagen and elastin in the vascular wall: a potential role in vascular stiffness and atherosclerosis. Clin Trans Sci. 2011;4:146–52.
- Wysokinski A, Zapolski T. Relationship between aortic valve calcification and aortic atherosclerosis: a transoesophageal echocardiography study. Kardiol Pol. 2006;64:694–701.
- Tulamo R, Frosen J, Junnikkala S, Paetau A, Kangasniemi M, Pelaez J, . Complement system becomes activated by the classical pathway in intracranial aneurysm walss. Lab Invest. 2010;90:168–79.
- Baldo G, Wu S, Howe RA, Ramamoothy M, Knutsen RH, Fang J, . Pathogenesis of aortic dilatation in mucopolysaccharidosis VII mice may involve complement activation. Mol Genet Metab. 2011;104:608–19.
- Elefteriades JA. Thoracic aortic aneurysm: reading the enemy's playbook. World J Surg. 2008;32:366–74.
- Fujii T, Zen Y, Sato Y, Sasaki M, Enomae M, Minato H, . Podoplanin is a useful diagnostic marker for epithelioid hemangioendothelioma of the liver. Modern Patholo. 2008; 21:125–30.
- Fernandez-Flores A. Lack of expression of podoplanin by microvenular hemangioma. Pathol Res Practice. 2008;204:817–21.
- Fraser DA, Tenner AJ. Innate immune proteins C1q and mannan-binding lectin enhance clearance of atherogenic lipoproteins by human monocytes and macrophages. J Immunol. 2010;1:3932–9.
- Barbetseas J, Alexopoulos N, Brili S, Aggeli C, Chrysohoou C, Frogoudaki A, . Atherosclerosis of the aorta in patients with acute thoracic aortic dissection. Cic J. 2008;72:1773–6.
- Rensen SS, Slaats Y, Driessen A, Peutz-Koostra CJ, Nijhuis J, Steffensen R, . Activation of complement system in human nonalcoholic fatty liver disease. Hepatology. 2009; 50:1809–17.
- Jenkins CP, Cardona DM, Bowers JN, Oliai BR, Allan RW, Normann SJ. The utility of C4d, C9, and troponin T immunohistochemistry in acute myocardial infarction. Arch Pathol Lab Med. 2010;134:256–63.
- Zhang B, Hirahashi J, Cullere X, Mayadas TN. Elucidation of molecular events leading to neutrophil apoptosis following phagocytosis: cross-talk between caspase 8, reactive oxygen species, and MAPK/ERK activation. J Biol Chem. 2003;1:28443–54.
- Bhatia VK, Yun S, Leung V, Grimsditch DC, Benson GM, Botto MB, . Complement C1q reduces early atherosclerosis in low-density lipoprotein receptor-deficient mice. Am J Pathol. 2007;170:416–26.
- Helske S, Oksjoki R, Lindstedt KA, Lommi J, Turto H, Werkkala K, . Complement system is activated in stenotic aortic valves. Atherosclerosis. 2008;196:190–200.
- Ganter MT, Brohi K, Cohen M, Shaffer LA, Walsh MC, Stahl GL, . Role of the alternative pathway in the early complement activation following major trauma. Shock. 2007; 28:29–34.