Abstract
Objectives. The aim of this study was to assess whether NLR levels are associated with echocardiographic parameters, New York Heart Association (NYHA) functional class, or B- type natriuretic peptide (BNP) levels in patients with idiopathic dilated cardiomyopathy (DCM). Design. Eighty-seven patients with idiopathic DCM were included prospectively from 2009 to 2014. Patients with acute decompensated heart failure and conditions that alter the total or differential white blood cell counts were excluded. Blood samples were collected before echocardiographic investigation on admission. Results. There was a statistically significant correlation between neutrophil/lymphocyte ratio (NLR) and NYHA functional class (r = 0.68, p < 0.001), BNP levels (r = 0.61, p < 0.001) and various echocardiographic parameters. NLR was significantly higher in patients in NYHA functional class III or IV (n = 39) than among those categorized as NYHA class I or II (n = 48), (3.3 ± 1.0 vs 2.1 ± 0.6; p < 0.001). The NLR cutoff value predicting severe chronic HF was 2.25 with 82% sensitivity and 65% specificity (p < 0.001). On multivariate linear regression analysis NLR (p = 0.025), left ventricular end-diastolic volume (p = 0.041) and left atrial volume index (LAVI) (p = 0.001) were found to be independent positive predictors of BNP levels. Conclusion. Neutrophil/Lymphocyte ratio is associated with the severity of chronic heart failure in patients with idiopathic DCM.
Introduction
Inflammation plays an important role in pathophysiology of chronic heart failure (HF) and its presence indicates worsening functional capacity and a poorer prognosis (Citation1,Citation2). High white blood cell (WBC) count, neutrophilia and relative lymphocytopenia are associated with increased mortality in patients with HF (Citation3–5). Recently, the neutrophil/lymphocyte ratio (NLR), a composite marker of systemic inflammation, has emerged as a new prognostic marker for a variety of cardiovascular diseases (Citation6). NLR has been superior to WBC, neutrophil counts and relative lymphocyte counts (RLC) at predicting the long-term mortality in patients admitted with acute decompensated HF (Citation7). However, although inflammation is important for chronic HF progression (Citation8), its relationship to cardiac structural deterioration is uncertain.
Idiopathic dilated cardiomyopathy (DCM) is a primary myocardial disease of unknown etiology which is likely to be multifactorial, potentially including occult viral myocarditis, immune system abnormalities, and genetic factors (Citation9,Citation10). About half of patients with cardiomyopathy are diagnosed with idiopathic DCM (Citation11), but data are sparse on the role of leukocytes for the severity of idiopathic DCM.
The aim of this study was to assess whether NLR levels are associated with echocardiographic parameters, New York Heart Association (NYHA) functional class, or (BNP) levels in patients with idiopathic DCM.
Material and methods
Study population
We included 87 patients with idiopathic DCM and admitted to our outpatient Cardiology clinic from 2009 to 2014. Patients with coronary artery disease documented by coronary angiography or nuclear scintigraphy, acute de-compensated heart failure, hypertensive or valvular cardiomyopathy, organic mitral valve disease, atrial fibrillation or flutter, chronic renal failure (creatinine ≥ 132 μmol/L or on hemodialysis) and hepatic or airway disease were excluded from the study. In addition, patients with conditions that could alter the total or differential WBC counts (hematopoietic disorders, malignancy, chronic inflammatory diseases, autoimmune diseases, infection, or recent history of chemotherapy, radiotherapy, or corticosteroid usage) were not included. Also, because cardiac resynchronization therapy decreases the NLR (Citation12), patients receiving resynchronization therapy were excluded. Patient functional status was assessed by using the NYHA functional classification scheme. Laboratory tests, including complete blood count with automated differential counts, were collected on admission as part of the routine clinical examination on the day before transthoracic echocardiography (TTE) was performed. Prior to data collection, the study had been approved by the local ethics committee and written informed consent was obtained from each patient.
Biochemical analyses and echocardiography
All samples were collected by vein puncture into EDTA tubes and analyzed immediately in our laboratory. BNP level was determined with a commercial kit which is for the quantitative measurement of BNP levels in human plasma by using the Access Immunoassay Systems. Complete blood count with automated differential counts was performed with a commercially automated system. NLR was calculated by dividing the absolute neutrophil count (ANC) by the absolute lymphocyte count. RLC was defined as (Total lymphocyte count/Total leukocyte count) x100.
TTE was performed in all patients in the left lateral decubitus position with a 2.5–3.5 MHz phased-array transducer probe (Vingmed System 3; GE Vingmed, Horten, Norway). All echocardiographic parameters were measured off-line, and an average of three cardiac cycles was used. Left ventricular ejection fraction (LVEF), left ventricular end systolic volume (LVESV) and end diastolic volume (LVEDV) were measured from apical four and two chamber views by using the modified Simpson method (Citation13). The left atrial volume was measured from the apical four-chamber view by using the area-length method in end systole before mitral valve opening. The left atrial volume index (LAVI) was obtained for all patients by dividing the left atrial volume by the body surface area (Citation13). Peak early (E) and late (A) transmitral filling velocities and deceleration time (Dec T) were measured to determine diastolic functions (Citation14). The severity of mitral regurgitation was measured by using the proximal isovelocity surface area method (Citation15). The estimated systolic pulmonary artery pressure (sPAP) was calculated as the sum of right ventricular pressure from the transtricuspid gradient and the estimated right atrial pressure (Citation14). Pulsed Doppler tissue imaging of tricuspid annular systolic motion (RV Sm) was used for the assessment of right ventricular systolic functions (Citation16).
Statistical analysis
Continuous variables were expressed as mean ± SD. Categorical variables were expressed as frequencies and percentages. Correlation analysis was performed by Spearman correlation test for variables with abnormal distribution. Mann-Whitney U tests for unequally distributed variables and Student's t tests were used in comparison of groups. Chi-square tests were used to compare categorical variables. Receiver-operating characteristic (ROC) curve for the prediction of severe chronic HF (NYHA class III-IV) was constructed and the area under the curve (AUC) was calculated for NLR. The CI value for the cut off NLR was calculated using the sensitivity and specificity estimates A multivariate linear regression analysis was performed to identify which parameters were independently associated with plasma BNP levels. Covariates included in linear regression analysis were LVEF, LVEDV, LVESV, LAVI, EROA, Dec T, sPAP, NLR, age, and creatinine. A p-value less than 0.05 were considered as statistically significant. All statistical analyses were performed by statistical software (SPSS Inc. 16.0, Chicago, IL, USA).
Results
A total of 87 patients (54 male, 33 female) with idiopathic DCM were assessed. The mean age of patients was 48.7 ± 13.8, and their mean LVEF was 29.7 ± 6.9. The average values for NLR, WBC, ANC and RLC were 2.6 ± 1.0, 7.7 ± 1.7, 4.9 ± 1.6 and 26.4 ± 7.7, respectively. Eighty-two (91%) of patients were on ACEİ/ARB, 69 (79%) on beta-blockers, and 74 (85%) on diuretics. The numbers of patients classified as NYHA functional classes I, II, III, and IV were 6, 42, 24, and 15, respectively. Baseline characteristics of the study population are summarized in . There were statistically significant correlations between NLR and NYHA functional class (r = 0.68, p < 0,001), BNP (r = 0.61, p < 0,001), () and various echocardiographic parameters (). Furthermore, NLR's correlation with these parameters was better than that of WBC, ANC, or RLC ().
Figure 1. Correlation between NLR and BNP (A), Dec T (B), LVEF (C). BNP: B-type natriuretic peptide, LVEF: Left ventricle ejection fraction, NLR: Neutrophil/lymphocyte ratio.
Table I. Baseline characteristics of the study population (n = 87).
Table II. Correlationship of NLR, WBC, ANC, and RLC with NYHA functional class, BNP, and echocardiographic parameters in patients with idiopathic dilated cardiomyopathy.
NLR was significantly higher in patients allocated to NYHA functional class III or IV (n = 39) than among those categorized as NYHA class I or II (n = 48); 3.3 ± 1.0 vs 2.1 ± 0.6; p < 0.001), (). These two groups are compared in terms of demographic, echocardiographic and hematological characteristics in . The NLR cut off value predicting severe chronic HF was 2.25 with 82% sensitivity and 65% specificity (AUC, 0.841; 95% CI, 0.74-0.93; p < 0.001), (). All parameters of cardiac remodeling, except RV Sm, were found to be further impaired in patients with NLR ≥ 2.25 (). On multivariate linear regression analysis, NLR (p = 0.025), LVEDV (p = 0.041), and LAVI (p = 0.001) were found to be independent positive predictors of BNP, with higher levels of each variable predicting higher levels of BNP ().
Figure 2. Patients in NYHA functional classes III- IV show significantly higher levels of NLR than NYHA classes I-II. NLR: Neutrophil/lymphocyte ratio, NYHA: New York Heart Association.
Figure 3. Receiver operating characteristic curve of neutrophil/lymphocyte ratio for predicting severe heart failure (NYHA class III-IV) in patients with idiopathic dilated cardiomyopathy. NLR: neutrophil/lymphocyte ratio, NYHA: New York Heart Association.
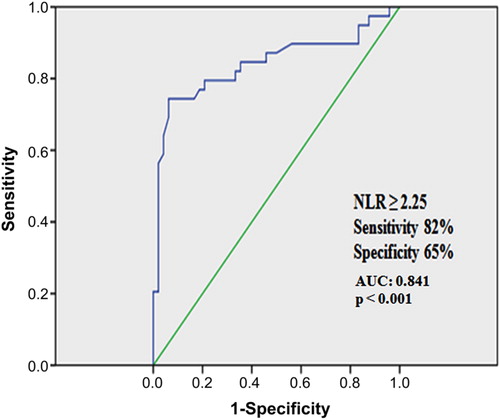
Table III. Comparison of variables according to NYHA functional class in patients with idiopathic dilated cardiomyopathy.
Table IV. Comparison of echocardiographic parameters according to the NLR level in patients with idiopathic dilated cardiomyopathy.
Table V. Independent predictors of increased B-type natriuretic peptid levels in multivariate linear regression analysis.
Discussion
Inflammation has been implicated in both the progression and clinical worsening of HF. The present study revealed a significant relationship between NLR and impaired echocardiographic indexes and functional capacity. In addition, NLR was found to be a significant and independent predictor of increased BNP levels. This correlation shows that NLR can reflect neurohumoral activation, as well as cardiac remodeling. Thus, NLR may be a useful marker of chronic HF severity in patients with idiopathic DCM. Activation of the sympathetic nervous and renin-angiotensin system and release of natriuretic peptides, endothelin, cytokines, and cortisol are the proven mechanisms behind HF progression (Citation17). Despite pharmacologic therapies targeting the above pathways and advanced interventional device treatments, HF still has high rate of mortality and morbidity (Citation10,Citation11). Recently, studies have focused on anti-inflammatory therapies hoping to reduce mortality rates. However, clinical trials testing the effects of anti-inflammatory therapies in HF have failed to demonstrate any significant clinical benefit (Citation1) and the pathophysiological role of inflammation in HF has become a controversial topic. Knowing the association between NLR and severity of chronic HF may better describe the pathophysiology and potentially serve to establish new therapies directed against inflammatory process.
Previous studies have shown that increased levels of leukocytes and certain leukocyte subtypes are associated with increased mortality in HF patients (Citation3–5). Leukocytes play an important role in the pathogenesis of HF, as well as being indicators of prognosis via their contribution to inflammation, extracellular matrix remodeling, and reparatory processes (Citation18). Although the precise mechanism of this inflammatory pathway remains unknown, leukocytes release pro-inflammatory cytokines like tumor necrosis factor alpha, interleukin-6 and C-reactive protein. These molecules may have direct deleterious effects on the myocardium, resulting in decreased ventricular function (Citation7). Activated neutrophils release a variety of proteolytic enzymes, such as myeloperoxidase, acid phosphatase and elastase, which facilitate increased tissue destruction (Citation7). Another hematological marker associated with mortality in HF is RLC (Citation5,Citation17). Chronic activation of sympathetic and renin-angiotensin systems stimulates hypothalamus-hypophysis-adrenal axis to secrete cortisol. Over- secretion of cortisol results in a low RLC that has been found to be an independent predictor of poor prognosis in patients with HF (Citation5,Citation17).
Recently, NLR that combines two WBC cell types into a single composite marker has been reported as a new prognostic marker for a variety of cardiovascular diseases (Citation6), also superior to individual WBC cell types at predicting poor outcomes in patients with acute decompensated HF (Citation7). LVEF is the most commonly used clinical measure of left ventricular systolic function, and a good indicator of cardiac remodeling (Citation19). In our study, we found a statistically significant correlation between NLR and LVEF. This finding suggests that NLR is linked to LV dysfunction in patients with idiopathic DCM. This was supported by other significant correlations between NLR and anatomic parameters like LVEDV, LVESV, LVEDD, LVESD and LAD. Furthermore, a correlation was identified between NLR and severity of mitral regurgitation, pulmonary artery pressure, and RV systolic function, all of which are worse predictors of HF prognosis. Thus, NLR may be implicated in the progression of myocardial damage, though further studies are required to demonstrate causality.
Higher NYHA functional class predicts hospitalizations, disease progression and mortality in patients with chronic HF (Citation20). Studies have consistently revealed a direct relationship between inflammatory cytokine levels and deteriorating functional classes of HF (Citation21). In our study, NLR was moderately to strongly correlated with NYHA functional class. Moreover, it was statistically higher in patients classified as NYHA functional class III or IV than among those in class I or II. An NLR ≥ 2.25 was 82% sensitive at predicting severe chronic HF. In addition to these findings, our study also revealed NLR to be positively correlated with the E/A ratio and LAVI and negatively with Dec T. It is well known that diastolic dysfunction (Citation22) and increases in LAVI (Citation23) are associated with impaired functional capacity, and are predictors of increased mortality in patients with chronic HF. In terms of the development and progression of diastolic dysfunction, the role of RAAS and inflammatory process is very complex. Briefly, the RAAS contributes myocardial and vascular inflammation through the activation of different cell types and secretion of cytokines and chemokines (Citation24). Inflammation leads to myocardial fibrosis and stiffness, which in turn result in diastolic dysfunction (Citation24). For these reasons and per our findings, NLR can also reflect both diastolic and systolic dysfunction.
NLR predicts long term mortality better than WBC, neutrophil counts and RLC in patients with HF (Citation7). According to our findings, this might be explained by the stronger correlations between NLR and a variety of adverse prognostic markers in HF. It can also be suggested that NLR is an indirect marker of increased sympathetic and renin angiotensin system activation, both of which contribute to myocardial damage. One possible explanation for this is that neurohumoral activation and cortisol secretion result in decreased lymphocyte counts that increase NLR relatively. The correlation between NLR and BNP further supports this theory, because BNP is secreted from ventricular myocytes in response to volume expansion, pressure overload and increased wall tension (Citation25). BNP levels increase in proportion to the severity of HF and are an independent predictor of hospitalizations, total mortality and cardiovascular death (Citation25).We found NLR, LVEDV and LAVI to be independent predictors of increased levels of BNP, a finding that clearly exhibits the influence of NLR on prognosis and adverse events in patients with idiopathic DCM.
Limitations
First, study limitation of note is the relatively small sample size for each subgroup of HF. Second, patients seen in clinical practice can have a variety of confounding causes for an abnormal NLR. In addition, inflammatory markers like C-reactive protein, myeloperoxidase, TNF alpha, and interleukin 6 were not measured and compared to NLR. Finally, the correlations between NLR and various anatomic indexes of echocardiography may not be valid for acute decompensated HF, as in the case of BNP.
Conclusion
It is well known that inflammation contributes to the progression of cardiac dysfunction and plays a role in the worsening of the clinical status. NLR is a noninvasive, inexpensive and readily available marker that may be used to assess severity of chronic HF in patients with idiopathic DCM.
Declaration of interest: The authors report no declarations of interest. The authors alone are responsible for the content and writing of the paper.
References
- Fu M. Inflammation in chronic heart failure: what is familiar, what is unfamiliar?Eur J Heart Fail. 2009;11:111–2.
- Anker SD, von Haehling S. Inflammatory mediators in chronic heart failure: an overview. Heart. 2004;90:464–70.
- Cooper HA, Exner DV, Waclawiw MA, Domanski MJ. White blood cell count and mortality in patients with ischemic and nonischemic left ventricular systolic dysfunction (an analysis of the Studies Of Left Ventricular Dysfunction [SOLVD]). Am J Cardiol. 1999;84:252–7.
- Arruda-Olson AM, Reeder GS, Bell MR, Weston SA, Roger WL. Neutrophilia predicts death and heart failure after myocardial infarction: a community-based study. Circ Cardiovasc Qual Outcomes. 2009;2:656–62.
- Ommen SR, Hodge DO, Rodeheffer RJ, McGregor CG, Thomson SP, Gibbons RJ. Predictive power of the relative lymphocyte concentration in patients with advanced heart failure. Circulation. 1998;97:19–22.
- Han YC, Yang TH, Kim DI, Jin HY, Chung SR, Seo JS, et al. Neutrophil to lymphocyte ratio predicts long-term clinical outcomes in patients with st-segment elevation myocardial ınfarction undergoing primary percutaneous coronary ıntervention. Korean Circ J. 2013;43:93–9.
- Uthamalingam S, Patvardhan EA, Subramanian S, Ahmed W, Martin W, Daley M, Capodilupo R. Utility of the neutrophil to lymphocyte ratio in predicting long-term outcomes in acute decompensated heart failure. Am J Cardiol. 2011;107:433–8.
- Heymans S, Hirsch E, Anker SD, Aukrust P, Balligand JL, Cohen-Tervaert JW, et al. Inflammation as a therapeutic target in heart failure? A scientific statement from the Translational Research Committee of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2009;11:119–29.
- Dec GW, Fuster V. Idiopathic dilated cardiomyopathy. N Engl J Med. 1994;331:1564–75.
- Wu AH. Management of patients with non-ischaemic cardiomyopathy. Heart. 2007;93:403–8.
- Felker GM, Thompson RE, Hare JM, Hruban RH, Clemetson DE, Howard DL, et al. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med. 2000;342:1077–84.
- Agacdiken A, Celikyurt U, Sahin T, Karauzum K, Vural A, Ural D. Neutrophil-to-lymphocyte ratio predicts response to cardiac resynchronization therapy. Med Sci Monit. 2013;19:373–7.
- Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63.
- Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009;10:165–93.
- Vahanian A, Baumgartner H, Bax J, Butchart E, Dion R, Filippatos G, et al. Guidelines on the management of valvular heart disease: the Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. Eur Heart J. 2007;28:230–68.
- Horton KD, Meece RW, Hill JC. Assessment of the right ventricle by echocardiography: a primer for cardiac sonographers. J Am Soc Echocardiogr. 2009;22:776–92.
- Acanfora D, Gheorghiade M, Trojano L, Furgi G, Pasini E, Picone C, et al. Relative lymphocyte count: a prognostic indicator of mortality in elderly patients with congestive heart failure. Am Heart J. 2001;142:167–73.
- Shantsila E, Bialiuk N, Navitski D, Pyrochkin A, Gill PS, Pyrochkin V, et al. Blood leukocytes in heart failure with preserved ejection fraction: impact on prognosis. Int J Cardiol. 2012;155:337–8.
- Solomon SD, Anavekar N, Skali H, McMurry JJ, Swedberg K, Yusuf S, et al. Influence of ejection fraction on cardiovascular outcomes in a broad spectrum of heart failure patients. Circulation. 2005;112:3738–44.
- Ahmed A. A propensity matched study of New York Heart Association class and natural history end points in heart failure. Am J Cardiol. 2007;99:549–53.
- Murray DR, Freeman GL. Proinflammatory cytokines: predictors of a failing heart?Circulation. 2003;107:1460–2.
- Fruhwald FM, Fahrleitner A, Watzinger N, Fruhwald S, Dobnig H, Schumacher M, et al. Natriuretic peptides in patients with diastolic dysfunction due to idiopathic dilated cardiomyopathy. Eur Heart J. 1999;20:1415–23.
- Popescu BA, Popescu AC, Antonini-Canterin F, Rubin D, Cappelletti P, Piazza R, et al. Prognostic role of left atrial volume in elderly patients with symptomatic stable chronic heart failure: comparison with left ventricular diastolic dysfunction and B-type natriuretic peptide. Echocardiography. 2007;24:1035–43.
- Sciarretta S, Paneni F, Palano F, Chin D, Tocci G, Rubattu S, et al. Role of the renin-angiotensin-aldosterone system and inflammatory processes in the development and progression of diastolic dysfunction. Clin Sci (Lond). 2009;116: 467–77.
- Isaac DL. Biomarkers in heart failure management. Curr Opin Cardiol. 2008;23:127–33.
