Abstract
Objective. The aim of this study was to investigate the relation between native thiol/disulfide ratio (TDR) and severity of coronary atherosclerosis as assessed by the Syntax score (SXscore) in patients with non-ST elevation myocardial infarction (NSTEMI) who underwent coronary angiography. Material and Methods. A total of 290 patients with NSTEMI who underwent coronary angiography, were included in the study between January and August 2014. Baseline coronary angiography determined the SXscore. The patients were divided into two groups: one with low SXscores (< 23) and the other with high SXscores (≥ 23). Results. TDR was significantly lower in patients with high SXscores (p < 0.001). In-hospital mortality was higher in the group with low TDR and high SXscores. The cut-off value of TDR on admission that predicted a high SXscore in the groups combined was 14, with a sensitivity of 73% and a specificity of 68%. Conclusion. TDR can be determined by an easy, inexpensive, automated, or optionally manual spectrophotometric assay, and correlates inversely with SXscore in patients with NSTEMI.
Introduction
Thiols, or as they are better known, mercaptans contain a sulfhydryl group (-SH) (Citation1). The plasma thiol pool is largely formed by albumin and protein thiols, with smaller contributions from low-molecular-weight thiols such as cysteinylglycine, cysteine (Cys), homocysteine, glutathione, and γ-glutamylcysteine (Citation2). Thiols can undergo oxidation reaction via oxidants and form disulfide bonds (Citation3). Oxidation of Cys residues can lead to reversible formation of mixed disulfides between low-molecular-mass thiols and protein thiol groups when oxidative stress increases. Formed disulfide bonds can again be reduced to thiol groups, therefore thiol–disulfide homeostasis is maintained (Citation4).
Thiol/disulfide ratio (TDR) has been shown to play critical roles in detoxification, antioxidant protection, signal transduction, regulation of enzymatic activity, apoptosis, and cellular signaling mechanisms (Citation5,Citation6). TDR has been increasingly investigated in many disorders, and a growing body of evidence shows that an abnormal thiol–disulfide homeostasis state is involved in the pathogenesis of a variety of disorders including cardiovascular diseases (Citation7).
Previous studies have shown that oxidative stress markers increase after myocardial infarction (MI) (Citation8,Citation9) and acute coronary syndromes, and a strong correlation has been shown between oxidative stress and coronary artery disease (CAD) (Citation10–12).
Syntax score (SXscore) evaluates the angiographic severity of coronary lesions (Citation13), and can predict early and late mortality and morbidity irrespective of disease severity in different clinical conditions, including non-ST elevation myocardial infarction (NSTEMI) (Citation14–20).
To the best of our knowledge, this study is the first report on the correlation between native TDR and SXscores in NSTEMI patients, with analysis of the correlations of TDR with angiographic and clinical risk scores.
Material and methods
Patients admitted to our clinic with NSTEMI, who underwent coronary angiography between January and August 2014, were included in the study. The diagnosis of NSTEMI was based on increased troponin levels and the presence of at least one of the following; ischemic symptoms, ischemic ECG changes other than acute ST segment elevations, or new wall motion abnormalities/new loss of viable myocardium assessed by cardiac imaging modalities (Citation29). Patients with troponin elevation due to other than acute coronary events, such as acute heart failure, pulmonary embolism, active infection or sepsis, chronic kidney disease, stroke, arrhythmias, and aortic dissection, were excluded from the study. Patients with chronic inflammatory diseases, hematologic disorders, liver disease, previous stroke, rheumatologic diseases, malignancy, previous MI, and ST elevation myocardial infarction (STEMI) were excluded too.
Transthoracic echocardiography was performed within 72 h after admission of the patients to hospital. Left ventricular ejection fraction (LVEF) was calculated using Simpson's method.
Blood samples from the patients after a fasting period of 12 h were collected into plain tubes, and serum was separated after centrifugation at 1500 g for 10 min and stored at− 80°C until analysis. Blood samples from calcium–EDTA tubes were analyzed in an auto-analyzer. Complete blood count and differentials were determined from the peripheral venous blood samples obtained at admission.
TDR was determined as described previously (Citation30). Briefly, reducible disulfide bonds were first reduced to form free functional thiol groups. Unused reductant sodium borohydride was consumed and removed with formaldehyde, and all thiol groups including reduced and native ones were detected after reaction with DTNB [5, 5’-dithiobis- (2-nitrobenzoic) acid]. Half of the difference between total and native thiols provided the dynamic disulfide amount (-S-S). After the determination of native thiol (-SH) and disulfide (-S-S) amount, native TDR (-SH/-S-S-) was calculated.
Two independent and experienced interventional cardiologists unaware of the clinical data of the patients calculated SXscores. There were no discrepancies between the interventional cardiologists that assessed the SX score. Each lesion ≥ 1.5 mm in diameter and had ≥ 50% stenosis was scored using version 2.1 of the on-line (www.syntaxscore.com). An SXscore ≥ 23 was regarded as severe CAD, by definition. After this, the patients were divided into two groups: the ones with low SXscores (< 23) and the ones with high SXscores (≥ 23).
SPSS 22.0 statistical software (SPSS Inc. Chicago, IL) was used to analyze data. Kolmogorov–Smirnov test was used to analyze the distribution pattern. Continuous data were presented as median and interquartile range (IQR), or mean ± standard deviation (SD). The Spearman correlation coefficient was calculated to analyze the association between two continuous variables. The effects of different variables on SXscore were determined with univariate analysis. Variables with unadjusted p values < 0.2 in logistic regression analysis were identified as potential risk factors and included in the full model. We eliminated potential risk factors using likelihood ratio tests with reduced model, using stepwise multivariate logistic regression analysis. A p value < 0.05 was considered statistically significant. The receiver operating characteristics (ROC) curve was used to show the sensitivity and specificity of TDR, and optimal cut-off value for predicting SXscore.
At the time of diagnosis, and before coronary angiography, all patients were given 300 mg acetyl salicylic acid po, the ones < 75 years of age were administered 300 mg clopidogrel po, and the ones ≥ 75 years of age were given 75 mg clopidogrel po, and 5,000 U heparin iv.
The standard Judkins technique and 6F catheters (Massachusetts, Expo; Boston Scientific Corporation) were used to perform baseline angiography through the femoral artery, and Siemens Axiom Sensis XP device was used.
Ankara Numune Education and Research Hospital's local ethics committee approved the study protocol, and all patients provided their written informed consents.
Results
Baseline clinical characteristics of the study patients and univariate analysis results (p-values) are presented in . There were 290 patients in the study group, and 96 of them (33%) had high SXscores. Gender, age, smoking status, rate of diabetes mellitus, levels of total cholesterol, low-density lipoprotein, high-density lipoprotein, creatinine, total bilirubin, hemoglobin, mean platelet volume, as well as counts of white blood cells, neutrophils, and platelets were similar in low- and high-SXscore groups.
Table I. Baseline clinical and biochemical characteristics of the study population, and univariate analyses.
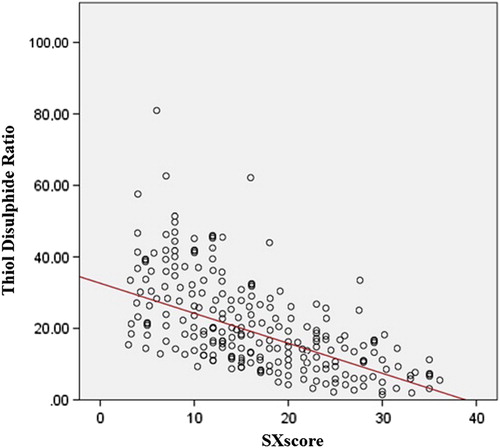
Univariate analysis showed that TDR, peak Troponin I level, LVEF, free thiol-, and disulfide levels were significantly correlated with SXscore in NSTEMI patients. Twenty-six patients died during hospitalization. In-hospital mortality rate was higher in patients with higher SXscores. When those four variables were incorporated in a multivariate analysis, the independent predictors of high SXscore were native TDR (95% confidence interval 6.949 to 13.741, p < 0.001), and LVEF (95% confidence interval 4.14–12.7, p = 0.001). Those variables were significantly lower in the high-SXscore group (). In-hospital mortality was higher in high-SXscore group. Patients with high SXscores had lower TDR compared with the ones with low-SXscores (). As shown in , there was a negative correlation between TDR and SXscore in patients with NSTEMI (n = 290, r = -0.445, p < 0.001)
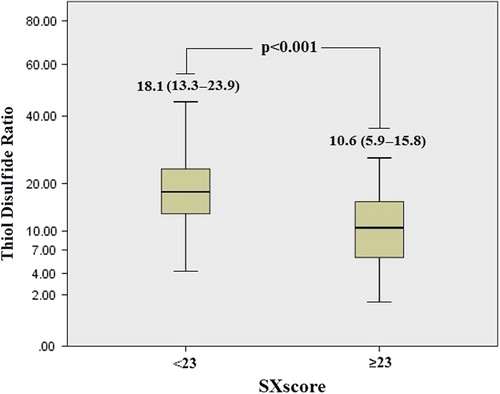
Table II. Multivariate logistic regression analysis showing independent predictors of high SXscores.
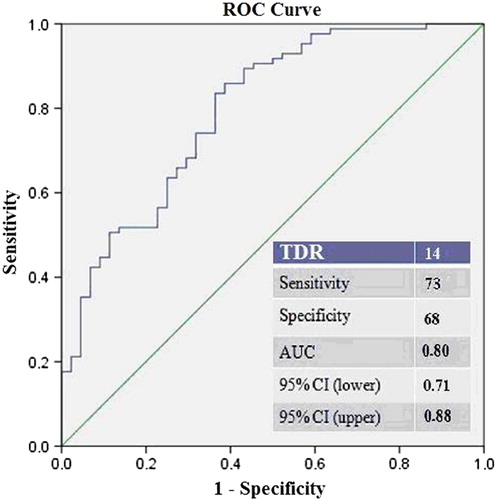
Lastly, ROC analysis was performed to determine the cut-off value of TDR to predict a high SXscore. The cut-off value of TDR on admission to predict a high SXscore in all population was 14, with a sensitivity of 73% and a specificity of 68% (area under the curve 0.80, p < 0.001; ).
The patients were divided into two groups based on TDR cut-off value of 14. Patients with a TDR ≥ 14 were younger than the patients with TDR < 14 (p = 0.043). In addition, peak Troponin I and SXscores were smaller, but LVEF was higher in the high TDR group. Finally, in-hospital mortality was higher in patients with a TDR < 14 compared with the ones with a TDR ≥ 14 (17% vs 4%, p < 0.001; ).
Table III. Clinical characteristics of the study population according to TDRs.
Discussion
To the best of our knowledge, the present study is the first investigation on the correlation between thiol–disulfide homeostasis and Syntax risk scores in NSTEMI patients. Our results indicated that TDR was significantly correlated with clinical risk factors and angiographic risk scores.
The SXscore, an anatomic scoring system based on coronary angiography that quantifies lesion severity, also predicts poor cardiovascular outcomes including mortality in NSTEMI patients (Citation21,Citation22). Palmerini et al. (Citation21) reported that SXscore was an independent predictor of 1-year death rate, MI, cardiac death, and target vessel revascularization in patients with NSTEMI. Scherff et al. (Citation22) found that the SXscore anticipated short-term adverse clinical events in elderly who had MI and underwent primary percutaneous coronary intervention (PCI). In another study, high SXscore was found to be an independent factor for stent thrombosis in patients with STEMI, and a predictor of late mortality (Citation23). Magro et al. (Citation23) demonstrated a relation between SXscore and the development of no reflow in patients that were treated with primary PCI for STEMI.
In a recent study, Yadav et al. (Citation24) showed a strong link between the severity and complexity of CAD as assessed by the SXscore, and the occurrence of stent thrombosis at 30-day- and 1-year follow-up in patients with NSTEMI who underwent PCI. The present study confirms that SXscore predicts in-hospital mortality rate in patients with NSTEMI. A SXscore ≥ 23 was associated with higher in-hospital mortality rate. Our findings demonstrates that TDR is correlated with age, peak Troponin levels and LVEF. All these findings suggest that admission to hospital TDR can be beneficial for clinical and angiographic risk assessment in NSTEMI patients.
It has been shown that oxidative stress indices increase after MI (Citation8,Citation9). NSTEMI alters biomarker levels including oxidative stress indices. The relationship between oxidative stress and CAD has attracted clinical interest for a long time, and it has been shown that both excessive oxidative stress and inadequate defense can induce early onset of severe CAD (Citation25). Increased oxidative stress markers act synergistically with the standard risk factors of CAD (Citation26,Citation27). Oxidative stress starts as a result of an impaired balance between antioxidant defense and reactive oxygen species. The onset of atherosclerotic disease increases oxidative stress (Citation10–12).
TDR has critical roles in detoxification, antioxidant protection, signal transduction, transcription factors and regulation of enzymatic activity, apoptosis, and cellular signaling mechanisms (Citation5,Citation6). It has been reported that an abnormal thiol–disulfide homeostasis state is involved in the pathogenesis of a variety of diseases including cardiovascular diseases (Citation7) and diabetes (Citation28). Recently, Erel and Neselioglu showed that plasma disulfide levels were higher in patients with degenerative diseases such as, diabetes, obesity, pneumonia, and in the cases of smoking, and were lower in patients with proliferative diseases such as multiple myeloma, urinary-bladder cancer, colon cancer, and renal cancer (Citation30).
We hypothesized that TDR might correlate to SXscores since previous studies support a close relation between TDR and anti-oxidative processes, and found a significant correlation. The role of anti-oxidation in the pathophysiology of coronary atherosclerosis also supports our hypothesis.
Our study has several limitations. First, coronary angiography was assessed visually, and only major lesions of coronary arteries can be detected in this way. The second limitation is the inclusion of a relatively small number of patients, all admitted to a single center. Finally, TDR was not compared with other oxidative stress indices, including lipid hydroperoxide, total antioxidant status, total oxidant status, oxidative stress index, paraoxonase, and arylesterase.
Conclusion
TDR was significantly lower in NSTEMI patients with high SXscores. Therefore, we believe that measuring TDR NSTEMI patients on their admission to hospital could be beneficial for clinical and angiographic risk assessment. Plasma TDR can be determined by the method used in our study since it is an easy, inexpensive, automated, and optionally manual spectrophotometric assay.
Acknowledgments
None.
Declaration of interest: The authors report no declarations of interest. The authors alone are responsible for the content and writing of the paper.
Funding
This research received no grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Sen CK, Packer L. Thiol homeostasis and supplements in physical exercise. Am J Clin Nutr. 2000;72:653–69.
- Turell L, Radi R, Alvarez B. The thiol pool in human plasma: the central contribution of albumin to redox processes. Free Radic Biol Med. 2013;65:244–53
- Cremers CM, Jakob U. Oxidant sensing by reversible disulfide bond formation. J Biol Chem. 2013;288:26489–96.
- Jones DP, Liang Y. Measuring the poise of thiol/disulfide couples in vivo. Free Radic Biol Med. 2009;47:1329–38.
- Biswas S, Chida AS, Rahman I. Redox modifications of protein–thiols: emerging roles in cell signaling. Biochem Pharmacol. 2006;71:551–64
- Circu ML, Aw TY. Reactive oxygen species, cellular redox systems, and apoptosis. Free Radic Biol Med. 2010;48: 749–62
- Go YM, Jones DP. Cysteine/cystine redox signaling in cardiovascular disease. Free Radic Biol Med. 2011;50:495–509
- Levy Y, Bartha P, Ben-Amotz A, Gerald Brook J, Dankner G, Lin S, et al. Plasma antioxidants and lipid peroxidation in acute myocardial infarction and thrombolysis. J Am Coll Nutr. 1998;17:337–41.
- Kasap S, Gönenç A, Sener DE, Hisar I. Serum cardiac markers in patients with acute myocardial infarction: Oxidative stress, C-reactive protein and N-terminal probrain natriuretic peptide. J Clin Biochem Nutr. 2007;41:50–7.
- Demirbag R, Rabus B, Sezen Y, Taækin A, Kalayci S, Balkanay M. The plasma and tissue oxidative status in patients with coronary artery disease. Turkish J Thorac Cardiovasc Surg J. 2010;18:79–82.
- Sezen Y, Bas M, Polat M, Yildiz A, Buyukhatipoglu, H, Kucukdurmaz Z, et al. The relationship between oxidative stress and coronary artery ectasia. Cardiol J. 2010;17:488–94.
- Gur M, Aslan M, Yildiz A, Demirbag R, Yilmaz R, Selek S, et al. Paraoxonase and arylesterase activities in coronary artery disease. Eur J Clin Invest. 2006;36:779–87.
- Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, et al. The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. Eurontervention. 2005;1:219–27.
- Valgimigli M, Serruys PW, Tsuchida K, Vaina S, Morel MA, van den Brand MJ, et al. Cyphering the complexity of coronary artery disease using the syntax score to predict clinical outcome in patients with three-vessel lumen obstruction undergoing percutaneous coronary intervention. Am J Cardiol. 2007;99:1072–81.
- Capodanno D, Di Salvo ME, Cincotta G, Miano M, Tamburino C, Tamburino C. Usefulness of the SYNTAX score for predicting clinical outcome after percutaneous coronary intervention of unprotected left main coronary artery disease. Circ Cardiovasc Interv. 2009;2:302–8
- Garg S, Sarno G, Serruys PW, Rodriguez AE, Bolognese L, Anselmi M, et al. Prediction of 1-year clinical outcomes using the syntax score in patients with acute st-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: A substudy of the strategy (single high-dose bolus tirofiban and sirolimus-eluting stent versus abciximab and bare-metal stent in acute myocardial infarction) and multistrategy (multicenter evaluation of single high-dose bolus tirofiban versus abciximab with sirolimus-eluting stent or bare-metal stent in acute myocardial infarction study) trials. JACC Cardiovasc Interv. 2011;4:66–75
- Caixeta A, Généreux P, Palmerini T, Lansky AJ, Mehran R, Dangas GD, et al. Prognostic utility of the syntax score in patients with single versus multivessel disease undergoing percutaneous coronary intervention (from the acute catheterization and urgent intervention triage strategy [acuity] trial). Am J Cardiol. 2014;113:203–10
- van Gaal WJ, Ponnuthurai FA, Selvanayagam J, Testa L, Porto I, Neubauer S, et al. The SYNTAX score predicts peri-procedural myocardial necrosis during percutaneous coronary intervention. Int J Cardiol. 2009;135:60–5.
- Yang CH, Hsieh MJ, Chen CC, Chang SH, Wang CY, Lee CH, et al. SYNTAX score: an independent predictor of long-term cardiac mortality in patients with acute ST elevation myocardial infarction. Coron Artery Dis. 2012;23:445–9.
- Magro M, Nauta S, Simsek C, Onuma Y, Garg S, van der Heide E, et al. Value of the SYNTAX score in patients treated by primary percutaneous coronary intervention for acute ST-elevation myocardial infarction: the MI SYNTAX Score study. Am Heart J. 2011;161:771–81.
- Palmerini T, Genereux P, Caixeta A, Cristea E, Lansky A, Mehran R, et al. Prognostic value of the SYNTAX score in patients with acute coronary syndromes undergoing percutaneous coronary intervention: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial. J Am Coll Cardiol. 2011;57:2389–97.
- Scherff F, Vassalli G, Sürder D, Mantovani A, Corbacelli C, Pasotti E, et al. The SYNTAX score predicts early mortality risk in the elderly with acute coronary syndrome having primary PCI. J Invasive Cardiol. 2011;23:505–10
- Magro M, Nauta ST, Simsek C, Boersma E, van der Heide E, Regar E, et al. Usefulness of the SYNTAX score to predict “no reflow” in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Am J Cardiol. 2012;109:601–6.
- Yadav M, Généreux P, Palmerini T, Caixeta A, Madhavan MV, Xu K, et al. Syntax score and the risk of stent thrombosis after percutaneous coronary intervention in patients with non-st-segment elevation acute coronary syndromes: An acuity trial substudy. Catheter Cardiovasc Interv. 2015;85:1–10.
- Chisolm GM, Steinberg D. The oxidative modification hypothesis of atherogenesis: An overview. Free Radic Biol Med. 2000;28:1815–26.
- Mallika V, Goswami B, Rajappa M. New risk factor-atherosclerosis pathophysiology and the role of novel risk factors: A clinicobiochemical perspective. Angiology. 2007;58:513–22.
- Morrow JD. Quantification of isoprostanes as indices of oxidant stress and the risk of atherosclerosis in humans. Arterioscler Thromb Vasc Biol. 2005;25:279–86.
- Matteucci E, Giampietro O. Thiol signaling network with an eye to diabetes. Molecules. 2010;15:8890–3
- Thygesen K, Alpert JS, Jaffe AS, White HD, Simoons ML, Chaitman BR, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60:1581–98
- Erel O, Neselioglu S. A novel and automated assay for thiol/disulphide homeostasis. Clin Biochem. 2014;47:326–32.