Abstract
Objectives. This project aims to identify socio-demographic, medical and psychosocial factors (study factors) associated with coronary risk control and prognosis, and to test their impact in a representative sample of coronary heart disease (CHD) patients. Design. The first phase includes a cross-sectional study designed to explore the association between the study factors and coronary risk factor control in CHD patients. Data from hospital records, a questionnaire, clinical examination and blood samples were collected. The independent effects of study factors on subsequent coronary events will be explored prospectively by controlling for baseline coronary risk factors. In the second phase, we will test the effect of tailored interventions to modify the study factors associated with unfavourable risk profile in phase I. Results. In all 1366 patients (21% women), aged 18-80 years with a coronary event on average 17 (2-38) months prior to study participation were identified (83% participation rate). Of the 239 patients who refused participation, 229 patients consented to analysis of hospital record data (non- participants). Conclusions. If the study variables contribute to CHD risk factors and prognosis, the present project may be important for the development of prevention programs by tailoring these to the patients perceived needs and behaviour profiles.
Trial registration: ClinicalTrials.gov identifier: NCT02309255.
Introduction
Mortality rates for atherosclerotic cardiovascular disease have been declining during the past decades due to improvements in diagnosis and treatment, leaving a larger number of patients in need of optimal secondary prevention.[Citation1] Even though unidentified risk factors obviously exist, traditional modifiable risk factors presently account for more than 90% of the risk of acute coronary events worldwide.[Citation2] Despite evidence-based secondary preventive guidelines for more than 20 years,[Citation3] non-adherence is still a major challenge. A recently published European multicenter study revealed a significant treatment gap as 30-70% of coronary heart disease (CHD) patients fail to achieve target levels for modifiable coronary risk factors.[Citation4] Furthermore, the participation rate in cardiac rehabilitation programs remains low (30-60%), particularly in high-risk patients, such as the elderly, and those with somatic and psychiatric comorbidity.[Citation5] Patient education, information and psychological support, which are essential components of rehabilitation programs, have not proven sufficient effective in reducing subsequent events,[Citation6,Citation7] and the link between patient information, psychosocial factors and coronary risk factor control and prognosis in CHD patients have yet to be established. The long-term consequences of the current practice with high readmission rates during the first five years after acute coronary syndromes have been demonstrated.[Citation8]
The reasons for unhealthy lifestyle and low-risk factor control are complex and poorly understood and the identification of modifiable patient and healthcare factors of importance for coronary risk profile remains a public health priority.[Citation3] Socio-demographic, medical and psychosocial factors may act as barriers to lifestyle changes, treatment adherence and may moderate the effects of cardiac rehabilitation.[Citation9] To our knowledge, the relative importance of these potentially modifiable factors in association with each established coronary risk factor not at target has not been studied. Furthermore, an increasing number of studies also suggest that concurrent psychosocial factors may worsen the prognosis of CHD.[Citation10,Citation11] For example, in one study anxiety was only associated with increased mortality in CHD patients in the presence of comorbid depression.[Citation10] Further studies that explore the combined effect of various psychosocial factors on cardiovascular prognosis and the mechanisms (e.g. behavioural pathways) by which they may lead to adverse cardiac outcomes in CHD patients have recently been requested.[Citation9] Furthermore, to our knowledge, previous studies have not explored the co-existence of the psychosocial factors other than anxiety and depression, while simultaneously controlling for traditional coronary risk factors.[Citation10] Further knowledge of the relationship between different psychosocial factors and bio-behavioural mechanisms linking psychosocial factors to cardiovascular prognosis in CHD patients may be useful in the development of more effective tailored secondary prevention programmes.
The purpose of the present NORwegian CORonary (NOR-COR) prevention study is to identify socio-demographic, medical and psychosocial factors (study factors) associated with unfavourable coronary risk factor control and subsequent cardiovascular events in CHD patients. Moreover, using tailored interventions the project will test the impact of the associated factors in a representative sample of coronary patients. The present paper presents the rationale for this study project, design, methods and baseline sample characteristics.
Materials and methods
Design of the NOR-COR model
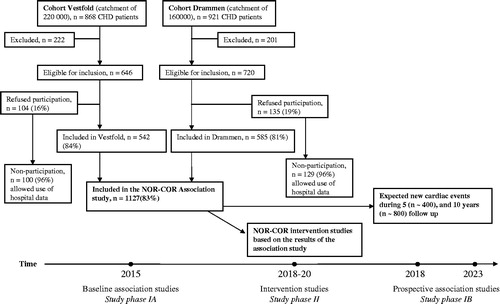
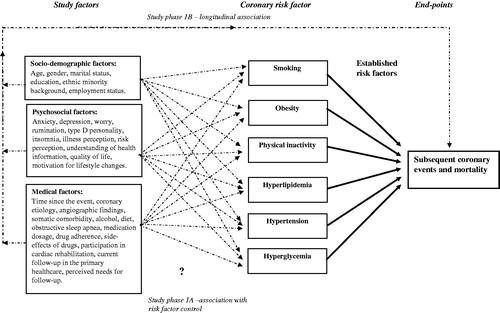
The NOR-COR model is illustrated in . The NOR-COR project is divided into an observational study phase I and an interventional study phase II, as illustrated in the study flow-chart (). Study phase IA is a cross-sectional study, with a retrospective component, designed to explore the associations between the study factors and control of each major coronary lifestyle and biological risk factor with established impact on CHD.[Citation3] The study factors and the coronary risk factors are defined in detail below. The NOR-COR dataset has included an extensive number of potentially modifiable study factors relevant for the patients’ ability to adhere to guidelines. Some of these factors have previously, to some extent, been demonstrated to be associated with coronary risk factors, adherence to medication and prognosis in cardiac patients.[Citation12–18] However, their relative contribution to coronary risk factor control and their interaction are not established and will therefore be explored to identify potential targets for interventions. In study phase IB, the independent effects of the study factors on subsequent coronary events and survival after 5 and 10 years, respectively, will be explored prospectively by controlling for baseline coronary risk factors.
In study phase II, we will test the effect of tailored interventions to modify the study factors that show significant association with unfavourable risk profile in phase I. For example, if we find illness perception to be associated with persistent smoking, we aim to conduct a randomised intervention study to test whether persistent smokers’ randomised to a tailored intervention that improves the patients’ illness perception also contribute to smoking cessation. Some of the study factors included in the NOR-COR dataset (e.g. depression) have previously been reported as being modifiable in cardiac patients.[Citation17] However, whether modification will be associated with improved drug adherence and risk factor control has previously not yet been tested. If significant study factors are identified for which no specific interventions exist, attempts will be made to develop novel tailored interventions.
Study population
All patients aged 18-80 years with first or recurrent diagnosis or treatments for CHD (acute myocardial infarction (ICD-10; I21), coronary artery by-pass graft operation, or elective or emergency PCI, defined as the index event/treatment) at two representative Norwegian hospitals (Drammen Hospital and Hospital of Vestfold) were selected from hospital patient discharge lists by searching chronologically after last admission for the index event during the past three years (2011-2014) prior to study inclusion. Exclusion criteria were: (i) a diagnosis of type 2 myocardial infarction, (ii) not able to understand the Norwegian language, (iii) cognitive impairment including living in nursing homes, (iv) psychosis, (v) drug abuse and (vi) short life expectancy due to terminal heart (NYHA class 4), lung, liver or kidney disease (stage 5), or malignant disease.
The study hospitals have a total catchment area of 380 000 inhabitants, with a representative blend of both city and rural areas in Norway regarding geography, economy, age distribution, cardiovascular morbidity and mortality.[Citation19] The cardiac rehabilitation programme at Drammen Hospital includes a multi-disciplinary one day “heart school” at the outpatient clinic, and exercise training twice per week in 6 weeks with start-up 4-6 weeks following the index event. The Hospital of Vestfold provides comprehensive lifestyle intervention with educational and training programme with duration amounting to 6 months after the event, described elsewhere.[Citation20] All participants gave informed consent before study participation. The study sample population and the study bio-bank were approved by the Regional Committee of Ethics in Medical Research. The NOR-COR Study is registered at www.ClinicalTrials.gov (ID NCT02309255).
Study assessments
All patients selected from the hospital database who fulfilled the inclusion criteria were mailed a letter with study information, an extensive self-report questionnaire (27 pages, 24 questionnaires), appointment for the clinical examination and collection of the venous blood samples. All blood samples were analysed at Drammen Hospital to avoid inter-laboratory bias. In and , all study variables are presented. Complete hospital records have been collected from study participants and 96% of the non-participants after a dedicated evaluation and consent by the ethics committee. Data from the self-report questionnaire, clinical examination and blood samples were obtained from study participants.
Table I. Main data collections in the NOR-COR study.
Table II. De novo NOR-COR variables (participants only).
As there was no validated questionnaire suitable for the study, the NOR-COR questionnaire was created de novo following an extensive process as recommended by Perk et al.[Citation21] The first set of questions was prepared and revised by the interdisciplinary research group (preventive cardiologists, psychosomatic and behavioural medicine specialists, specialist in questionnaire development). After two revisions, two cardiac nurses and two CHD patients contributed further valuable comments, the latter in order to incorporate the patients’ perspective in all questions (“patient research partners”). A third version was tested in 20 randomly selected eligible CHD patients in order to estimate relevance, acceptance and feasibility. All patients understood and accepted the questionnaire and responded to all items. After final minor changes, the questionnaire was approved by the research group for the present study.
Psychosocial factors were assessed by questionnaires that are widely used in this field for comparative reasons.[Citation10,Citation13] Assessment methods for main variables: Anxiety and depression were assessed by the Hospital Anxiety and Depression Scale (HADS), which is a 14-item self-report questionnaire comprising items covering symptoms of anxiety (HADS-A) and depression (HADS-D). It was designed to be applied in hospital settings and focuses on psychological and cognitive symptoms rather than somatic symptoms.[Citation22] Rumination was assessed by the Ruminative Response Scale (RRS). The RRS is a 22-item self-report inventory designed to assess the tendency to ruminate in response to a depressed mood. The items focussed on the meaning of rumination and thinking about feelings related to depressed mood, symptoms, consequences and its causes.[Citation18] Worry was assessed by the Penn State Worry Questionnaire (PSWQ), a 16-item measure of pathological worry.[Citation23] Type D personality was assessed by DS-14, which consists of 14 items with seven items each on subscales of negative affectivity and social inhibition. The sum of the scores on each subscale was calculated, and subjects were regarded as positive for negative affectivity or social inhibition if above 10. To be categorized with type D personality, both subscales must be positive.[Citation24]
Subsequent cardiovascular events were obtained from the Norwegian Cardiovascular Disease Registry (www.fhi.no/artikler/?id=112056) and the Cause of Death Registry in Norway (http://www.fhi.no/helseregistre/dodsaarsaksregisteret). In addition, the hospital records at the participating hospitals will be screened.
Primary outcome measures
The primary outcome measures in study phase IA are the major coronary risk factors that are not at targeted in the interview.[Citation3]
Behavior risk factors: (i) smoking, (ii) physical activity [Citation25] less than 30 min of moderate intensity three times a week, and (iii) BMI > 25.0 and 30.0 kg/m2, waist circumference >94 and 102 cm [men] and >80 and 88 cm [women].
Biological risk factors: (i) total-cholesterol >4.5 mmol/l, LDL cholesterol >1.8 mmol/l, (ii) BP (26) > 140/90 mmHg [>140/80 mmHg in Diabetes], and (iii) HbA1c >6.1% [>7.0% in patients with diabetes mellitus]).
BMI, BP, total and LDL-cholesterol and HbA1c will also be studied as continuous variables applying linear regression analyses.
In study phase IB, the composite outcome includes (1) re-hospitalization with subsequent coronary events, i.e. acute myocardial infarction (ICD-10; I21), coronary artery by-pass graft operation, or elective or emergency PCI and (2) cardiovascular and all-cause mortality obtained after 5 and 10 years, respectively.
Covariates
The following descriptive and potentially modifiable study factors will be obtained from the comprehensive dataset:
Socio-demographic factors: Age, gender, ethnicity, marital status, level of education and employment status.
Medical factors:
Type of coronary event, angiographic findings, coronary intervention, number of coronary events and time since the index coronary event.
Participation in the cardiac rehabilitation programme.
Number of follow-up visits past year in primary healthcare.
Somatic [Citation27] and psychiatric co-morbidity at hospital discharge.
Medication at discharge, cardiovascular medication at interview, and drug adherence.[Citation28]
Obstructive sleep apnea.[Citation29]
Diet [Citation30] and alcohol consumption.[Citation31]
Self-reported perceived needs
Self-reported perceived needs for further secondary preventative follow-up.
Psychosocial factors
Psychological factors: Anxiety and depression,[Citation22] rumination,[Citation13] worry.[Citation23]
Type D personality.[Citation24]
Sleep disturbances.[Citation32]
Quality of life (Short Form-12).[Citation33]
Illness perception,[Citation34] risk perception,[Citation16] beliefs regarding what caused their CHD, and perception and understanding of the information provided by health care workers.[Citation21]
Current motivation for further lifestyle changes.
Statistics
In the REACH study,[Citation35] the incidence of the composite cardiovascular endpoint was 35% after 4 years follow-up in patients with established CHD. We can therefore expect at least 400 cases with subsequent events after 5 years follow-up. The present study will have a 80% power (alpha = 0.05) of detecting a 10% difference between participants and non-participants in binary outcomes (e.g. coronary events) when the overall proportion of given outcome is approximately one-third and a 95% power at an overall level of 20%. Differences within the participant group with respect to psychosocial risk factors, such as HADS (assuming a 20% rate of positives) will be detected with 90% power when the binary outcome has a between-group difference of 10% and the overall level is 15% (even with continuity correction).
Associations between covariates (study factors) and the other coronary risk factors will be analysed univariately using an independent samples t-test for continuous variables, correlation coefficients for pairs of continuous variables and χ2 test for categorical variables. The relative contribution of study factors with continuous study outcomes will be assessed by multiple linear regressions and ANCOVAs and with logistic regressions for binary outcomes, with interaction terms included where appropriate. Cox regression analysis will be used to explore the relative contribution of study factors on subsequent cardiovascular events by when controlling for established coronary risk factors at baseline. Cox regression analysis will be used to assess relative risk of subsequent cardiovascular events between study participants and non-participants.
Protocols
In study phase IA, the first two papers will describe the prevalence of coronary risk factors not at target in a representative population from Northern Europe. Prevalence of coronary risk factor not at target will be compared with European data,[Citation4] within the different high risk patient groups (elderly, co-morbidity, patients not attending cardiac rehabilitation) and in the patient groups 2-12 months and 12-36 months after the index coronary event, respectively. Furthermore, hospital record data will be compared between participants and non-participants regarding risk factors, somatic and psychiatric co-morbidity. Through six association studies, we will explore how all study factors are associated with each major coronary risk factor not at target. A review paper will summarise all study factors associated with poor coronary risk factor control and suggest intervention models tailored to the specific risk factor, and thus give empirical evidence to tailored effective components that can be implemented in cardiac rehabilitation programmes. In study phase IB, we will conduct several prospective cohort studies to explore the independent effects of the study factors on subsequent coronary events and survival by controlling for baseline coronary risk factors.
In phase II of the project, we will conduct tailored intervention studies to attempt to modify the study factors with significant associations with the coronary risk profile in phase I. We might identify important patient and/or healthcare factors that cannot be modified through interventions in a hospital setting, such as factors related to the organisation of the primary healthcare. These factors can be tested in other study settings and may be useful for policymakers in developing population strategies.
Main characteristics of the study population
The catchment area of the two Norwegian hospitals with 380 000 inhabitants is a representative selection of the population of Norway, amounting to 7.5%. In total, 1789 patients aged 18-80 years were identified with an index coronary event. Of these, 423 were excluded and 1366 patients invited to participate. The reasons for exclusion were: cognitive impairment (n = 28), psychosis (n = 18), drug abuse (n = 10), short life expectancy (n = 136), dead (n = 160), not able to understand the Norwegian language (n = 44) and other (n = 26). A total of 1127 patients (82.5%) consented to participate. Of the 239 patients who refused the participation, 229 patients consented to analysis of hospital record data (non-participants). Ten patients (0.7%) refused to participate in the non-participants’ study. The frequency of missing values for the questionnaire based data is low, within the range of 0-10%. Baseline characteristics are presented in and . The study included a number of underserved patient groups including women, old patients and with low socio-economic status. The prevalence of coronary risk factors above current recommendations at the index event ranged between 17% and 64%.
Table III. Baseline socio-demographic and medical characteristics of the NOR-COR study participants.
Table IV. Baseline data on coronary diagnosis, angiographic findings, interventions, risk factors and participation in the cardiac rehabilitation programme of the study participants.
Strength of the study
The NOR-COR study includes a representative, clinical cohort with a high participation rate (83%). The comprehensive data set analysed as a connected whole will enable us to study a large number of potentially important patient and healthcare factors influencing coronary risk factor control, subsequent events and survival. Knowledge about the relative importance of these factors regarding control of the major lifestyle factors as well as their relative and combined predictive power with respect to subsequent cardiovascular events will provide new knowledge of putative bio-behavioural mechanisms linking psychosocial factors and cardiovascular prognosis in CHD patients. In addition, the study will give new knowledge of the characteristics of non-participants and their risk of subsequent cardiovascular events. The study has evolving methods by introducing a systematic stepwise approach for the development of empirical-based intervention components tailored to the patients’ underlying problem that will be tested in study phase II. The study design and the questionnaire have been developed by an interdisciplinary study group including CHD patients.
Study limitations
The coronary risk factors were measured at one time point and thus could be influenced by measurement or recall bias. Additional important factors associated with poor coronary risk factor control included those related to patient-provider communication, which cannot be explored in this study. Selection-bias is always a challenge in a study setting. This study allows us to explore characteristics of a majority of the non-participating patients to account for this. The results should thus be fairly representative of a general CHD population.
Conclusions
The NOR-COR project is now established with a sufficient number of patients to address factors that may explain why patients with CHD do not adhere to guidelines that would make for a longer and healthier life. The comprehensive interdisciplinary approach identifies potentially important patient and healthcare factors and tests their impact by tailored interventions. If the identified factors contribute to CHD risk factors and the prognosis of CHD, the present project may be important for the development of prevention programmes by tailoring these to the patients perceived needs and behaviour profiles.
Acknowledgements
The authors thank study patients and all study personnel in the NOR-COR Research group for their invaluable help in completing the study.
The NOR-COR project is based at Department of Medicine Drammen Hospital and the study is funded and carried out at the sections for cardiology at Drammen and Vestfold Hospitals. The concept is developed by the project in close collaboration with communities at the University of Oslo, with methodological expertise in behavioral sciences. The study was funded by research grants from the participating hospitals.
Declaration of interest
The authors report no conflicts of interest.
References
- Nichols M, Townsend N, Scarborough P, et al. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J. 2014;35:2929–2933.
- Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952.
- Perk J, De Backer G, Gohlke H, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J. 2012;33:1635–1701.
- Kotseva K, Wood D, De Bacquer D, et al. EUROASPIRE IV: a European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J of Prev Cardiol. Epub ahead of print 6 January 2015. DOI: 10.1177/2047487315569401.
- Beswick AD, Rees K, Griebsch I, et al. Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups. Health Technol Assess. 2004;8:1–152.
- Brown JP, Clark AM, Dalal H, et al. Effect of patient education in the management of coronary heart disease: a systematic review and meta-analysis of randomized controlled trials. Eur J of Prev Cardiol. 2013;20:701–14.
- Whalley B, Rees K, Davies P, et al. Psychological interventions for coronary heart disease. Cochrane Database Syst Rev. 2011;(8):CD002902. DOI: 10.1002/14651858.CD002902.pub3.
- Fox KA, Carruthers KF, Dunbar DR, et al. Underestimated and under-recognized: the late consequences of acute coronary syndrome (GRACE UK-Belgian Study). Eur Heart J. 2010;31:2755–2764.
- Pogosova N, Saner H, Pedersen SS, et al. Psychosocial aspects in cardiac rehabilitation: from theory to practice. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation of the European Society of Cardiology. Eur J Prev Cardiol. 2015;22:1290–1306.
- Watkins LL, Koch GG, Sherwood A, et al. Association of anxiety and depression with all-cause mortality in individuals with coronary heart disease. J Am Heart Assoc. 2013;2:e000068.
- Rutledge T, Linke SE, Krantz DS, et al. Comorbid depression and anxiety symptoms as predictors of cardiovascular events: results from the NHLBI-sponsored Women's Ischemia Syndrome Evaluation (WISE) study. Psychosomatic Med. 2009;71:958–964.
- Gehi A, Haas D, Pipkin S, et al. Depression and medication adherence in outpatients with coronary heart disease: findings from the Heart and Soul Study. Arch Internal Med. 2005;165:2508–2513.
- Tully PJ, Cosh SM, Baune BT. A review of the affects of worry and generalized anxiety disorder upon cardiovascular health and coronary heart disease. Psychol Health Med. 2013;18:627–644.
- Svansdottir E, Denollet J, Thorsson B, et al. Association of type D personality with unhealthy lifestyle, and estimated risk of coronary events in the general Icelandic population. Eur J Prev Cardiol. 2013;20:322–330.
- Grandner MA. Addressing sleep disturbances: an opportunity to prevent cardiometabolic disease? Int Rev Psychiatry. 2014;26:155–176.
- Broadbent E, Petrie KJ, Ellis CJ, et al. Patients with acute myocardial infarction have an inaccurate understanding of their risk of a future cardiac event. Internal Med J. 2006;36:643–647.
- Lichtman JH, Froelicher ES, Blumenthal JA, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation. 2014;129:1350–1369.
- Denton EG, Rieckmann N, Davidson KW, Chaplin WF. Psychosocial vulnerabilities to depression after acute coronary syndrome: the pivotal role of rumination in predicting and maintaining depression. Front Psychol. 2012;3:288. DOI: 10.3389/fpsyg.2012.00288.
- Assessed 1st of March at Statistics Norway. Available from: http://statbank.ssb.no/statistikkbanken.
- Otterstad J. Influence on lifestyle measures and five-year coronary risk by a comprehensive lifestyle intervention programme in patients with coronary heart disease. Eur J Cardiovasc Prev Rehabil. 2003;10:429–437.
- Perk J, Hambraeus K, Burell G, et al. Study of Patient Information after percutaneous Coronary Intervention (SPICI): should prevention programmes become more effective? EuroIntervention. 2015;10: e1–e7.
- Zigmond A, Snaith R. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370.
- Pallesen S, Nordhus IH, Carlstedt B, et al. A Norwegian adaptation of the Penn State Worry Questionnaire: factor structure, reliability, validity and norms. Scand J Psychol. 2006;47:281–291.
- Denollet J. DS14: standard assessment of negative affectivity, social inhibition, and Type D personality. Psychosom Med. 2005;67:89–97.
- Kurtze N, Rangul V, Hustvedt BE, et al. Reliability and validity of self-reported physical activity in the Nord-Trondelag Health Study: HUNT 1. Scand J Public Health. 2008;36:52–61.
- Alpert BS. Validation of the Welch Allyn ProBP 3400: a device for modern medical practice. Blood Press Monit. 2011;16:156–158.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
- Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74.
- Netzer N, Stoohs R, Netzer C, et al. Using the Berlin questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–491.
- Mosdol A. Dietary assessment – the weakest link?: A dissertation exploring the limitations to questionnaire based methods of dietary assessment [PhD thesis]. Norway: Department of Nutrition, Institute of Basic Medical Sciences, Faculty of Medicine, University of Oslo; 2004.
- Støver M, Bratberg G, Nordfjærn T, et al. Bruk av alkohol og medikamenter blant eldre (60+) i Norge. Levanger: HUNT forskningssenter, NTNU; 2012.
- Pallesen S, Bjorvatn B, Nordhus IH, et al. A new scale for measuring insomnia: the Bergen Insomnia Scale. Percept Mot Skills. 2008;107:691–706.
- Mols F, Pelle AJ, Kupper N. Normative data of the SF-12 health survey with validation using postmyocardial infarction patients in the Dutch population. Qual Life Res. 2009;18:403–414.
- Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–637.
- Bhatt DL, Eagle KA, Ohman EM, et al. Comparative determinants of 4-year cardiovascular event rates in stable outpatients at risk of or with atherothrombosis. JAMA. 2010;304:1350–1357.