Abstract
Fractional photothermolysis has become popular in the recent years and is currently widely used for the treatment of scars and for photo-rejuvenation purposes. The fractional photothermolysis is to thermally alter a ‘fraction’ of the skin, leaving intervening areas of normal skin untouched, which rapidly repopulate the altered columns of tissue. Fractional photothermolysis is subdivided into non-ablative and ablative fractional resurfacing. Ablative fractional resurfacing uses fractional CO2 or Er:YAG lasers to create deeper columns of thermal damage.Few studies have compared fractional CO2 and Er:YAG lasers on scars and cutaneous photodamages by a split trial. In this pilot study, we have compared the effects, down time, postprocedure erythema, pain of CO2 and Er:YAG fractional lasers using analysis of clinical photographs, dermoscopic findings and patient's rate of satisfaction.
Introduction
Fractional photothermolysis has become popular in recent years and is currently widely used for the treatment of scars and for photo-rejuvenation purposes. The purpose of the fractional photothermolysis is to thermally alter a ‘fraction’ of the skin, leaving intervening areas of normal skin untouched, which rapidly repopulate the altered columns of tissue (Citation1). Fractional photothermolysis is subdivided into non-ablative and ablative fractional resurfacing. Ablative fractional resurfacing uses fractional CO2 or Er:YAG lasers to create deeper columns of thermal damage (Citation2).
Few studies have compared fractional CO2 and Er:YAG lasers on scars and cutaneous photodamages by a split trial. In this pilot study, we have compared the effects, downtime, post-procedure erythema, pain of fractional CO2 and Er:YAG lasers using analysis of clinical photographs, dermoscopic findings and patient's rate of satisfaction.
Methods
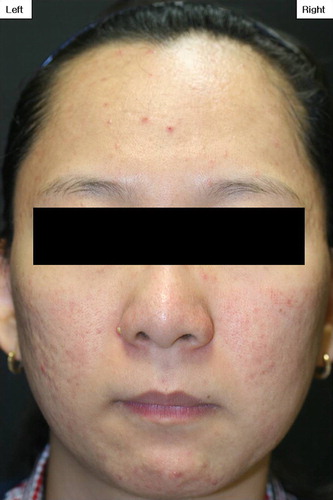
Our case series included 13 female patients (aged 23–57 years; Fitzpatrick skin types III and IV), all with either scars or cutaneous photodamage (). We performed a split trial using fractional CO2 (iPixel CO2 ™; Alma laser, Israel) and Er:YAG lasers (Profile ProFractional ™; Sciton Inc., Palo Alto, CA, USA), respectively. The study was approved by the Institutional Review Board of the Catholic Medical Center, and the patients gave written informed consent before enrollment.
Table I. Patients’ characteristics, laser parameters, short-term discomfort following laser treatment and patient satisfaction.
Topical anesthetic cream (EMLA®; AstraZeneca, London, UK) was applied for 30 min prior to treatment. The procedure was performed by a single dermatologist under the following energy settings (fractional CO2 laser; 25–50 mJ/ pixel, 9 × 9 pixel, high (70W) and fractional Er:YAG laser; 100–200 μm with 5.5% coverage, coagulation none and scanning area of 8 × 8 mm), depending on the patient's condition (scar depth, degree of photodamage, skin type). Postoperative care included application of Cicaplast® (La Roche Posay, France) on both sides of the face, twice daily after a light facial wash. Sun avoidance and sun protection with a broad spectrum sunscreen were advised.
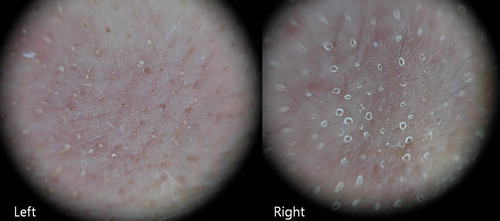
Photographic documentations under identical camera settings (Sony DSC-H9, 8.1 megapixels, high resolution settings, 3253 × 2448; Sony Corp., Tokyo, Japan) and dermoscopic documentations (DermoGenius®) were obtained at baseline and 1 week after the treatment. Two blinded dermatologists compared the degree of erythema and microcrusts on the CO2 and Er:YAG-treated sides of the patients’ face from reviewing the photos taken 1 week post-treatment. Patients were asked about their overall rate of satisfaction and pain comparing both sides.
Results
At 1 week follow-up, significant improvement was seen in skin texture and scars compared with the baseline skin condition. Seven of 13 patients (53.8%) said that fractional CO2 laser was much more painful than fractional Er:YAG laser. The rest of the patients (46.2%) said that they could not tell any difference regarding pain. Six patients had remaining microcrusts only on the fractional CO2 laser side (46.1%) (), whereas 53.9% of patients had no microcrusts left on either side of the face at 1 week follow-up visit. In terms of postprocedure erythema, there was no significant difference between fractional CO2 and Er:YAG lasers within our treatment parameters. Regarding the patient's satisfaction, three patients replied that overall they were more satisfied with the fractional CO2 laser than Er:YAG laser (23.0%) (). No significant side effects were noticed following the laser procedure except for post-procedural erythema, reactive acne (3 patients on both sides), and pin-point bruising (1 patient, both fractional CO2 and Er:YAG-treated areas and 2 patients, only on the fractional Er:YAG treated side) ().
Discussion
CO2 laser (10,600 nm) heats cells instantly to more than 100℃C, resulting in vaporization and removal of a surface layer of cells; coagulation necrosis of cells and denaturation of extracelluar proteins in a subjacent residual layer; nonfatal damage to cells in a deeper zone; and heat-induced shrinkage of collagen (Citation3). An Er:YAG laser of 2,940 nm (shorter wavelength than CO2 laser), which also targets intracellular water, can deliver energy more precisely without extensive thermal damage to the surrounding tissue, permitting quicker wound healing and recovery of dermis, although it exerts less hemostatic effect and dermal tightening than the CO2 laser (Citation4). In terms of discomfort such as pain, postprocedure erythema and microcrust, few reports have compared the fractional CO2 and Er:YAG lasers (Citation5,Citation6).
This pilot study shows that both fractional CO2 and Er:YAG lasers have certain instantaneous effects in the treatment of photodamage and scars. Although fractional CO2 laser was more painful and required a longer recovery period than fractional Er:YAG laser, all our patients replied that they were overall either equally or more satisfied fractional CO2 laser than Er:YAG laser. From the findings, we could see that the greater discomfort following fractional CO2 laser could easily be overcome by the better efficacy of the fractional CO2 laser, especially with those with deeper skin lesions such as scars. Interestingly, among the side effects following fractional laser therapy, pin-point bleeding was more commonly associated with fractional Er:YAG laser which may be related to the poor coagulation properties of Erbium.
Few studies have compared the efficacy and side effects of fractional CO2 and Er:YAG lasers in the past. Khatri et al. have shown that Er:YAG laser has significantly less residual thermal dermal damage, with a faster healing time and less post-procedure erythema compared to fractional CO2 laser (Citation5). Alexiades-Armenakas et al. report that fractional CO2 laser has superior results but the Er:YAG laser is better tolerated with less downtime in acne scar patients (Citation1). In terms of post-procedure discomfort, Karsai et al. report that the discomfort was slightly more pronounced after Er:YAG treatment in the first few days, but later on there were more complaints following CO2 laser treatment (Citation6).
Based on the results of our own study and previous reports, we suggest that the fractional Er:YAG laser might be more suitable for treating superficial and mild lesions such as photodamages and for people who want minimal downtime. Fractional CO2 lasers may be the choice for those with scars and who opt for greater treatment outcome.
This pilot study has limitations in that we cover only a small sample size, a single treatment course and a short follow-up period. We mainly aimed to compare the early post-procedure discomforts including pain, erythema and crusts (micro-crusts or blood crusts) following the two popular ablative fractional lasers. Further controlled long-term follow-up studies are needed to define the long-term effects and satisfaction between the two fractional lasers.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Alexiades-Armenakas MR, Dover JS, Arndt KA. The spectrum of laser skin resurfacing: Nonablative fractional, and ablative laser resurfacing. J Am Acad Dermatol. 2008; 58:719–737.
- Chrastil B, Glaich AS, Goldberg LH, Friedman PM. Second-generation 1,550-nm fractional photothermolysis for the treatment of acne scars. Dermatol Surg. 2008;34: 1327–1332.
- Geronemus RG. Fractional photothermolysis: current and future applications. Lasers Surg Med. 2006;38:169–176.
- Hu S, Hsiao WC, Chen MC, Huang YL, Chang SL, Shih PY, Gold MH. Ablative fractional erbium-doped yttrium aluminum garnet laser with coagulation mode for the treatment of atrophic acne scars in Asian skin. Dermatol Surg. 2011;37:939–944.
- Khatri KA, Victor R, Grevelink JP, Magro CM, Anderson RR. Comparison of erbium:YAG and carbon dioxide lasers in resurfacing of facial rhytides. Arch Dermatol. 1999;135:391–397.
- Karsai S, Czarnecka A, Jünger M, Raulin C. Ablative fractional lasers (CO(2) and Er:YAG): a randomized controlled double-blind split-face trial of the treatment of peri-orbital rhytides. Lasers Surg Med. 2010;42:160–167.