Abstract
For more than a century, exogenous lipids and injectable silicone have been used by nonmedical personnel or even licensed physicians to correct body defects and augment parts of the human body. Any skin-implanted exogenous substances can trigger an inflammatory response in individuals. Notably, oily substances have commonly been reported to produce a foreign body granulomatous reaction known as “sclerosing lipogranuloma”. Despite local and systemic complications, injections of illegal materials by unlicensed practitioners are widespread and are still a problem throughout East Asian Countries. We herein present a unique case of sclerosing lipogranuloma following illegal filler injection.
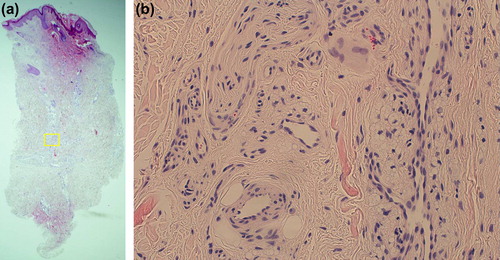
A 62-year-old Korean woman came in with a disfigured nose. On close inspection, we could see extreme thickening and lichenification of the nasal root as well as the upper two-thirds of the nose (, inlet). Such features, especially when seen from sideways, closely mimicked that of an “Elephant's Trunk” (). Forty years prior to this photo, the patient received filler injection to the nose by an illegal practitioner. Since the injection, there was gradual thickening of the nose which dramatically worsened following injection of a “dissolving agent” which was again performed by a nonmedical person in an attempt to resolve the lesion. Although our patient recalled the injected materials as liquid agents, she was not able to identify the exact nature of the substances. On histology, there was increased fibrosis resulting in an apparent increased dermal thickness (). The main pathological findings were overt granulomatous response to foreign substances with mononuclear cells, lipid laden macrophages, and foreign-body giant cells (). Spherioles of washed out artifact confirmed former presence of an oily substance. Following histological confirmation of sclerosing lipogranuloma, the patient was asked to undergo treatment but is currently lost for follow-up.
Figure 1. (inlet) There is extreme thickening and lichenification of the nasal root as well as the upper two-thirds of the nose. Such features, especially when seen from sideways, closely mimic that of an “Elephant's Trunk”.

Figure 2. (a) On histology, we can see increased fibrosis with an apparent increased dermal thickness. (b) The main pathological findings are overt granulomatous response to foreign substances with mononuclear cells, lipid laden macrophages, and foreign-body giant cells. Spherioles of washed out artifact confirms former presence of an oily substance. Hematoxylin and eosin, original magnification (a) × 40; (b) × 400.
Many patients in East Asia have a problem of a flat nasal bridge and find a way to have their nose augmented. Not surprisingly, in addition to the penis, breast, and certain parts of the face, the nasal dorsum is one of the most popular locations for filler injection (Citation1). Generally, the success of injection rhinoplasty relies on fibrosis of the tissue around the injected material, which creates a tissue prominence and prevents migration. However, problems related to uncontrolled granulomatous and fibrous reaction around the injected substance may occur, resulting in a distorted nose contour. Such disfigurement leads patients to seek medical attention. Common clinical presentations are palpable mass on the nose, erythema with or without telangiectasia on the overlying skin, and nodularity of the nose, but extreme features can be seen as in our case.
In a previous study, sclerosing lipogranuloma of the nose was reported to have an onset of 1–16 years after the injection (Citation1). Such variation in onset time is said to be largely dependent on the constitution of the injected materials, individual responses, trauma, etc. Injection of a “dissolving agent” in our patient may have caused secondary trauma to the nose. The resultant fragmentation and spread of the original material likely have irritated the surrounding tissue, aggravating the preexisting lipogranuloma. In addition to the local inflammatory reaction, systemic complications such as pulmonary edema and autoimmune disease can follow injection of modelants (Citation2). However, this is rare in cases of nose augmentation as only small amounts of material are injected into a relatively hypo-vascular area of the nasal dorsum.
Local steroid injection or oral steroids, as well as anti-inflammatory and anti-mitotic drugs such as minocycline and 5-FU have been used for the treatment of foreign-body granuloma. However, it is felt that an appropriate surgical excision is the treatment of choice in our case (Citation1,Citation3). Saddle-nose deformity following lipogranuloma removal can be corrected by various methods including a cartilaginous graft and a free fat graft.
Dermatologists should be vigilant about the various complications associated with fillers and be equipped to treat the complications when they do arise. It is also equally important that physicians advocate patients to see reputable physicians who use FDA-approved, purified products for an injection.
Notice of Correction
Changes have been made to this article since its original online publication date of 10 January 2014.
Declaration of interest: The authors report no declarations of interest. The authors alone are responsible for the content and writing of the paper.
References
- Sinrachtanant C, Tantinikorn W, Warnnissorn M, Assanasen P. Sclerosing lipogranuloma of the nose: a new treatment using adipose tissue transplantation. Facial Plast Surg. 2003;19: 363–367.
- Cabral AR, Alcocer-Varela J, Orozco-Topete R, Reyes E, Fernández-Domínguez L, Alarcón-Segovia D. Clinical, histopathological, immunolocial and fibroblast studies of 30 patients with subcutaneous injections of modelants including silicone and mineral oils. Rev Invest Clin. 1994;46: 257–266.
- Park TH, Seo SW, Kim JK, Chang CH. Clinical outcome in a series of 173 cases of foreign body granuloma: improved outcomes with a novel surgical technique. J Plast Reconstr Aesthet Surg. 2012;65:29–34.
