Abstract
Background: Anxiety and depression are common co-morbidities that can complicate the course of chronic obstructive pulmonary disease (COPD). The purpose of this study was to evaluate their impact on healthcare utilization and costs in a managed care COPD population. Methods: Administrative claims data were used to conduct a retrospective cohort study of COPD patients ≥40 years of age, including those with co-morbid COPD-Depression (including anxiety). COPD-Depression patients were matched to COPD patients without depression (COPD-Only cohort) using propensity scores. Conditional logistic regression models assessed the 1-year risk of COPD exacerbations (i.e., emergency room [ER] visit/inpatient hospitalization) between cohorts. Differences in annual all-cause and COPD-related utilization/costs, along with 2-year costs, were also compared between the cohorts. Results: There were 3,761 patients per cohort. Patients in the COPD-Depression cohort were 77% more likely to have a COPD-related hospitalization (odds ratio [OR] = 1.77, P < 0.001), 48% more likely to have an ER visit (OR = 1.48, P < 0.001), and 60% more likely to have hospitalization/ER visit (OR = 1.60, P < 0.001) compared to the COPD-Only cohort. Average annual all-cause medical cost per patient was $23,759 for COPD-Depression vs $17,765 for COPD-Only (P < 0.001) and total (medical plus pharmacy) cost was $28,961 vs $22,512 (P < 0.001), respectively; corresponding average annual COPD-related medical cost was $2,040 vs $1,392 (P < 0.001) and total cost was $3,185 vs $2,680 (P < 0.001). Similar trends were observed over the 2-year period. Conclusions: In the COPD population, patients with depression/anxiety have significantly higher risk of COPD exacerbations and annual all-cause and COPD-related costs than patients without these co-morbidities. These findings may have therapeutic implications and seem worthy of further exploration.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD), the fourth leading cause of death in the United States (US), is associated with substantial direct and indirect costs (estimated at $38.8 billion annually in 2005 $US) (Citation1–5). In 2000, COPD was estimated to account for 8 million physician office and outpatient (OP) hospital visits, 1.5 million emergency room (ER) visits, and 726,000 inpatient hospitalizations (Citation3,4). COPD is also associated with multiple co-morbidities, which contribute to its high economic burden (Citation3).
There is a high frequency of depression among patients with COPD, for which the prevalence has varied in the published literature (estimated to affect nearly two-thirds of patients with oxygen-dependent disease, with rates of approximately 10% to >40% for those with stable COPD) (Citation6). In a sample of patients aged ≥50 years from the 2004 Health and Retirement Survey in the US, depression symptoms were 2.7 times more likely to occur in those with COPD compared to those with no COPD (Citation7). This increased risk was higher than for most other chronic illnesses studied, including stroke, diabetes, coronary heart disease, arthritis, cancer, and hypertension, where the risk ranged from 1.3 to 2.1 times higher if a patient had the medical condition. Furthermore, data derived from the 1999 National Health Independent Survey showed a high annual prevalence of depression among COPD patients of 15.4%, yielding an increased risk of 3.2 times compared to patients without COPD (Citation8). Stein et al. evaluated the relative impact of major depressive disorder on 6 chronic physical conditions, including COPD, and found this co-morbidity nearly doubled the likelihood of healthcare utilization, functional disability, and work absence relative to patients with the same chronic condition but without depression (Citation9). It is also well appreciated that chronic conditions, including COPD, are frequently associated with anxiety disorders, with the potential to further escalate the cost of care (Citation10). In patients with stable COPD, the reported prevalence of anxiety disorders has generally ranged from 10% to 20% (Citation6). In a study in the United Kingdom in which the existence of depression and anxiety in the COPD population was assessed via the Hospital Anxiety Depression Scale (HADS), depression was designated as definite in approximately one-third of patients, and anxiety in 25%, with similar rates of both conditions when comparing the subsets receiving or not receiving long-term oxygen therapy (Citation11).
Despite the plethora of information linking depression/anxiety to COPD, the impact of COPD with co-morbid depression and anxiety on direct healthcare costs is not well documented. On this basis, we examined the economic impact of co-morbid depression and/or anxiety on COPD in a managed care population, and characterized healthcare resource use and direct medical, pharmacy, and total costs (both all-cause and COPD-related).
METHODS
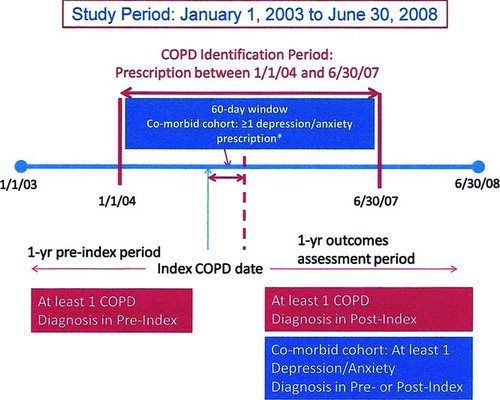
This observational, retrospective, matched cohort study () was conducted to assess healthcare resource utilization and costs among patients with co-morbid COPD and depression/anxiety and COPD alone.
Data source
This study utilized an integrated source of medical and pharmacy claims from the IMS LifeLink Database for the timeframe of January 2003 through June 2008 (Citation12). The database contains data from over 100 different managed healthcare plans encompassing over 60 million patients.
Medical, pharmacy, and eligibility component files were utilized to identify inpatient and outpatient diagnoses and procedures, prescription records, demographic characteristics, and eligibility information. Dates of service and amounts charged and paid for the service/drug were available for all claims. The data are fully de-identified and compliant with the Health Insurance Portability and Accountability Act.
Patient selection
COPD patients were identified using a pharmacy claim for a COPD maintenance medication (i.e., inhaled corticosteroids [beclomethasone dipropionate, budesonide, flunisolide, fluticasone propionate, triamcinolone acetonide], long-acting beta-agonists [formoterol fumarate, salmeterol xinafoate, arformoterol tartrate], anticholinergics [ipratropium (IPR) bromide, IPR bromide/albuterol, tiotropium bromide], fixed-dose combination therapy [fluticasone propionate + salmeterol xinafoate 250/50 mcg]) between January 1, 2004 and June 30, 2007 (COPD identification period); the date of the first COPD medication was deemed the index COPD date. Additionally, patients were required to be ≥40 years of age, eligible to receive healthcare services for 1 year pre- and post-index COPD date, and have at least 1 medical claim with a COPD diagnosis (International Classification of Diseases, Ninth Revision [ICD-9] codes 491.xx, 492.xx, or 496.xx) during the 1-year pre- and post-index COPD date. Patients were excluded if they had specific co-morbid conditions (i.e., respiratory cancer [160 to 163.xx, 231.xx], cystic fibrosis [277.0x], bronchiectasis [494.xx], pneumoconiosis [500 to 505.xx], pulmonary fibrosis [515.xx], pulmonary tuberculosis including fibrosis due to tuberculosis [011.xx], or sarcoidosis [135.xx]) any time during the study period.
Patients were placed in the COPD-Depression cohort if they had ≥1 prescription claim for a medication used to treat depression/anxiety (selective serotonin reuptake inhibitors, tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, monoamine oxidase inhibitors, and bupropion) within 60 days post-index COPD date. The date of the prescription was deemed the index depression date. Diagnosis of depression/anxiety (ICD-9 codes 293.89, 296.2x, 296.3x, 300.00, 300.01, 300.02, 300.21, 300.22, 300.23, 300.3x, 300.4x, 308.3x, 309.81, 311.xx) during the 1-year pre- or post-index depression date was also required to be included in the COPD-Depression cohort. Patients were placed in the COPD with no depression cohort (COPD-Only cohort) only if they had no diagnosis or medication for depression/anxiety any time in the study period. Eligible patients had a 1-year pre-index period for measurement of baseline characteristics and were then followed for 1 to 2 years post-index date depending on the outcome of interest.
Propensity score matching
As the intent of the research was to evaluate the effect of depression/anxiety on healthcare resource utilization and costs under the assumption of “all other factors being equal,” baseline differences between cohorts would have the potential to bias the results. Therefore, patients in the COPD-Depression and COPD-Only cohorts were matched in a 1:1 ratio using propensity scores, with the score for each patient defined as the probability of having co-morbid depression (i.e., date of the depression prescription medication after the COPD index date) conditional on baseline variables (measured in the 1-year pre-index COPD date), including demographics (i.e., age, gender), co-morbidity measures (i.e., Charlson co-morbidity index, presence of asthma, number of unique prescription classes, number of prescriptions, number of unique diagnoses, all-cause medical costs, and all-cause pharmacy costs), and proxies for COPD severity (i.e., number of oral corticosteroid [OCS] prescriptions, number of short-acting beta agonist [SABA] canisters, number of IPR canisters, use of home oxygen therapy, COPD-related medical costs, and COPD-related pharmacy costs). Matching proceeded using the technique of nearest available matching on the estimated propensity score, performed up to 3 decimal places (0.001). The success of the resulting propensity score to reduce bias was assessed by evaluating the balance in the covariates between the cohorts after matching.
Outcome measures
All-cause and COPD-related resource utilization and costs (adjusted to 2008 $US based on the medical component of the Consumer Price Index) were calculated in the 1-year post-index date (index depression date for the COPD-Depression cohort and index COPD date for the COPD-Only cohort). Specific resource utilization measures included annual number of all-cause and COPD-related physician office, ER, hospitalization, and hospital-based OP visits. Additionally, the presence of a COPD-related ER visit, COPD-related hospitalization, and a combined outcome of a COPD-related ER and/or COPD-related hospitalization, all of which were indicative of a COPD-related exacerbation, were also examined. Specific cost measures included annual all-cause and COPD-related medical, pharmacy, and total healthcare costs. Cost measures were also calculated for the 2-year post-index period. COPD-related physician office, ER, and OP visits were defined by claims with a primary diagnosis for COPD. Similarly, COPD-related hospitalization was defined by claims with a primary discharge diagnosis for COPD.
Statistical analysis
Baseline demographics and clinical characteristics were described with standard summary statistics (means and proportions). Covariates were compared using chi-square tests for categorical variables and t-tests or Mann-Whitney tests for continuous variables. After propensity score matching, baseline characteristics were compared between cohorts using paired t-tests or Wilcoxon signed rank tests (continuous variables) and McNemar's tests (categorical variables).
Adjusted resource utilization and costs were assessed using multivariate analyses. Covariates that were statistically different after matching were included in the statistical models. Generalized linear models using a gamma distribution with a log link were used to obtain predicted costs. Conditional logistic regression models assessed the risk of a COPD-related ER visit/hospitalization over a 1-year follow-up period, and conditional negative binomial regression models assessed the number of visits.
All statistical analyses tested a 2-sided hypothesis of no difference between treatment cohorts at a significance level of 0.05, and were carried out using SAS statistical software (version 9.1).
RESULTS
Study population
A total of 31,483 patients met all study criteria and were eligible for matching (COPD-Only = 25,521; COPD-Depression = 5,962). At baseline, patient demographics and characteristics differed significantly between cohorts (data not shown). Therefore, matched cohorts were created based on propensity scores, each containing 3,761 patients. Although matching reduced many cohort differences (and covariates were numerically similar), statistically significant differences remained in selected demographic information, co-morbidity measures, and COPD severity indicators ().
Table 1 Baseline characteristics (propensity score-matched cohorts)
Table 2 Adjusted annual all-cause and COPD-related visits
Specifically, patients in the COPD-Only cohort were older, more likely to be male, had higher co-morbidity measures, had greater all-cause medical and pharmacy costs, received more OCS prescriptions, and had greater COPD-related pharmacy costs compared to the COPD-Depression cohort. These differences were controlled for in the statistical models when assessing outcomes of interest.
Outcome measures
With statistically significant between-cohort differences in baseline characteristics post-matching, all outcome measures were analyzed by multivariate techniques, controlling for covariates for which differences were significant. Adjusted annual all-cause and COPD-related visits are summarized in . The average number of annual all-cause physician office visits was 17% higher (incidence rate ratio [IRR] = 1.17; 95% confidence interval [CI]: 1.13, 1.21) for the COPD-Depression cohort vs the COPD-Only cohort; likewise, average numbers were 43% higher for annual all-cause ER visits (IRR = 1.43; 95% CI: 1.29, 1.58), 6% higher for all-cause OP visits (IRR = 1.06; 95% CI: 1.01, 1.11), and 52% higher for all-cause hospitalizations (IRR = 1.52; 95% CI: 1.39, 1.67).
The average number of annual COPD-related physician office visits was 12% higher (IRR = 1.12; 95% CI: 1.07, 1.17) and the average number of annual hospitalizations was 2% higher (IRR = 1.02; 95% CI: 1.01, 1.03) for the COPD-Depression cohort vs the COPD-Only cohort. Differences in frequencies of COPD-related OP visits and ER visits (both higher with COPD-Depression) were not statistically significant.
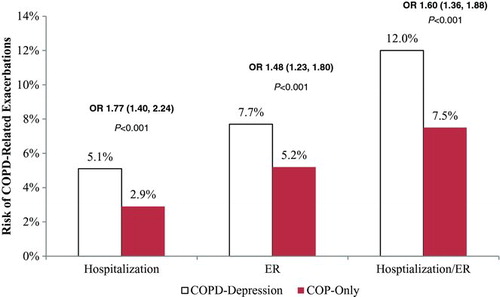
Patients with COPD-Depression were 77% more likely to have a COPD-related hospitalization (OR = 1.77 [1.40, 2.24]; P < 0.001), 48% more likely to have an ER visit (OR = 1.48 [1.23, 1.80]; P < 0.001), and 60% more likely to have a hospitalization/ER visit (OR = 1.60 [1.36, 1.88]; P < 0.001) compared with the COPD-Only cohort ().
Figure 2 Risk of COPD-related hospitalization/emergency room visit. Key: COPD –chronic obstructive pulmonary disease; ER –emergency room; OR –odds ratio.
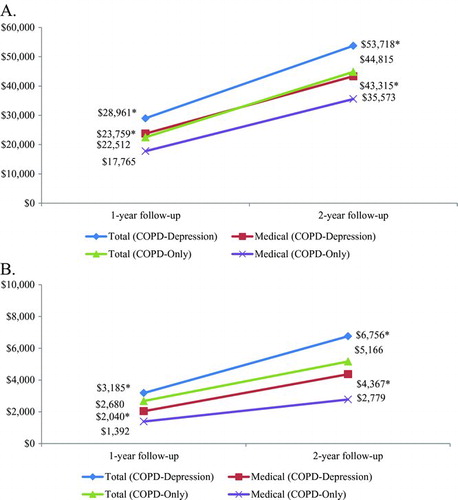
Mean predicted annual all-cause and COPD-related total healthcare costs were significantly higher for the COPD-Depression cohort vs the COPD-Only cohort (), with the difference in all-cause total healthcare costs ($28,961 vs $22,512; P < 0.001) largely attributable to the difference in all-cause medical costs ($23,759 vs $17,765; P < 0.001). Similarly, the difference in COPD-related total healthcare costs ($3,185 vs $2,680; P < 0.001) was driven by COPD-related medical costs ($2,040 vs $1,392; P < 0.001).
After 2 years of follow-up, the COPD-Depression cohort continued to have higher cumulative all-cause total healthcare and medical costs () and higher cumulative COPD-related total and medical costs () relative to the COPD-Only cohort.
DISCUSSION
To our knowledge, there have been no published studies focused on both healthcare resource utilization and costs for COPD patients with and without depression/anxiety. This study showed significant increases in the risk of COPD exacerbations (i.e., hospitalization and ER visits) and all-cause resource utilization examined in a commercial managed care setting for patients with COPD and depression/anxiety relative to those with COPD alone. Additionally, in the 1- and 2-year follow-up periods, the COPD-Depression cohort had higher average all-cause and COPD-related costs (total and medical) than the COPD-Only cohort. Our study confirms the hypothesis that the addition of depression/anxiety to COPD results in a substantial increase in overall and COPD-specific utilization and costs.
Table 3 Predicted annual all-cause and COPD-related healthcare costs
Numerous reports have documented the propensity for patients with COPD to exhibit depression and/or anxiety (Citation7,Citation12–20), which are co-morbidities shown to adversely affect physical functioning, overall health status, and self-perceived quality of life in the COPD population (Citation13,Citation19–22). In a Swedish observational study, patients with COPD had a significantly higher prevalence of depression and anxiety than patients with rheumatoid arthritis, diabetes, or healthy subjects, and were most likely to have a pessimistic view of the future (Citation13). The reason for the particularly high prevalence of depression and anxiety in the COPD population is not clear, but likely multifactorial in many cases, with various factors such as gender, current smoking status, socioeconomic variables, and disease-related factors (long-term use of oxygen, ability to walk) identified as underlying influencers (Citation6,7,Citation23).
Our findings within a managed care population are consistent with several recent reports collectively supporting a substantial influence of depression on healthcare utilization, including COPD exacerbation-related hospitalizations (Citation14,Citation24–27). Using the HADS in a prospective cohort study in patients with stable COPD, adjusted IRRs for symptom-based exacerbations, event-based exacerbations, and hospitalizations for the probable depression subset were 1.51, 1.56, and 1.72, respectively, compared with the non-depression subset (Citation27).
Figure 3 Predicted all-cause healthcare costs (A) and COPD-related healthcare costs (B) in 1-year and 2-year follow-up. Key: COPD –chronic obstructive pulmonary disease. Note: Significance testing was performed for COPD-Depression group vs COPD-Only group for each cost category. *P < 0.05, COPD-Depression cohort vs COPD-Only cohort.
In a cross-sectional primary care survey of 207 patients with COPD, moderate to high levels of depressive symptoms were common (60.4%), and over a 6-month period were associated with nonsignificant increases in physician visits (mean of 1.89 vs 1.13 for COPD-Only) and ER visits (0.28 vs 0.17) for lung disease, and significantly more hospitalizations (0.27 vs 0.06; P≤0.05) (Citation24). In a retrospective cohort study of Maryland Medicaid beneficiaries with COPD, which did not evaluate outcomes for a group without depression, but was similar to our study in that it was a claims-based analysis of a managed care population focused on both healthcare utilization (albeit limited to total physician office visits, OP services, and hospitalization) and associated direct costs, the prevalence of co-morbid depression was high at 63.4%, but similar to the 56.4% prevalence in an age/sex/race-matched non-COPD control group. (Citation26) Patients with COPD-Depression required significantly more healthcare utilization than the control group (incremental utilization of 17.7 visits; P = 0.001); however, the corresponding difference in annual medical costs approached but did not reach significance ($9,057 for COPD-Depression vs $7,725 for the control; P = 0.067).
Although our study could not draw any conclusions about the effects of treating depression on the burden of COPD, nor did it try to evaluate the effects of undiagnosed or untreated depression in the cohort, our findings support that depression screening and management should be included as a routine component of care in the COPD population. In this regard, clinical studies to characterize the relative benefits of initial depression/anxiety medication vs nonpharmacologic interventions would be worthwhile. Currently, only limited nonpharmacologic interventions have been shown to be effective, including pulmonary rehabilitation and cognitive behavioral therapy. (Citation6) However, the effect of antidepressants in COPD has not been fully explored.
As the intent of the current research was to evaluate the effect of depression/anxiety on healthcare resource utilization and costs under the assumption of “all other factors being equal,” it was necessary to ensure that both populations were similar at baseline. Therefore, the propensity score-matching technique was employed, which substantially reduced the variation in baseline characteristics between the cohorts. However, there were still statistically significant differences between the matched cohorts with respect to several pretreatment characteristics. In fact, these statistical differences suggest the COPD-Only cohort may have worse health status than the COPD-Depression cohort. It is important to note, however, that some of the differences in characteristics may not be clinically meaningful, since the characteristics are numerically similar. For example, the average number of OCS prescriptions received was 0.7 and 0.6 for COPD-Only and COPD-Depression, respectively. Although the difference of 0.1 is statistically significant, it may not be clinically relevant. Other characteristics that followed a similar trend were age and co-morbidity measures. To attenuate the potential bias in pretreatment characteristics, these factors were adjusted for in the multivariate analysis. This is one of the advantages of the current analysis.
Another advantage of our design is that we required a diagnosed and treated population for both conditions. This is a conservative approach in cost-of-illness analyses, since it excludes patients who are diagnosed but not treated, and those treated but not diagnosed. We also required depression/anxiety treatment to occur in close proximity with the COPD treatment (within 60 days) to ensure greater confidence in capturing a truly co-morbid population. We also ensured the COPD-Only group did not receive any depression/anxiety medication or diagnoses throughout the study period, in order to achieve a cleaner cohort.
Our study permitted us to examine a large patient population; however, as with any observational study, conclusions must be interpreted within the context of its limitations. Despite matching and multivariate adjustment, the possibility of groups not being matched on all unobserved characteristics exists (i.e., residual confounding). Another limitation is the potential misidentification and misclassification of patients into the cohorts of interest. Due to the lack of clinical parameters available in the data, a combination of ICD-9 diagnosis codes and medications were used to identify patients, which is the standard for claims database research (Citation28–31). For example, Mapel et al. have conducted a validation of administrative data using clinical measures and concluded that variables used in observational research of these administrative databases were fairly accurate and robust (28).
Another potential limitation is that the cost of co-morbid depression may be underestimated, as our study provides no insight into the indirect costs of COPD and co-morbid depression/anxiety. These costs may be substantial, but are difficult to compute within this observational study design. A final limitation may exist with respect to the calculation of propensity scores. This score was based on propensity to receive depression/anxiety treatment within the 60-day window after the index COPD date. However, the variables used to calculate this score were obtained from the 1-year pre-index period. This resulted in a small bias, although mitigated by most treatment occurring close to the index COPD date.
In conclusion, the presence of co-morbid depression/anxiety increases the risk of COPD-related exacerbations and imposes incremental and higher all-cause and COPD-related expenditures than those encountered in the general COPD population. For a multifactorial condition like COPD, which has substantial economic implications, further understanding of key co-morbidities like depression may add to the evaluation and management of COPD for the benefit of patients.
DECLARATION OF INTEREST
Funding for this study and resultant publication was provided by GlaxoSmithKline (GSK, study number ADC112645). Each author was involved in the design/analysis of the study and data interpretation, critically reviewed/edited drafts of the manuscript, and approved the final version of the manuscript for submission. Manan Shah is the guarantor of the paper and takes responsibility for the integrity of the work as a whole, from inception to published article. Laurie Orloski provided editorial contributions to this manuscript and received compensation from Xcenda.
REFERENCES
- Foster TS, Miller JD, Marton JP, Caloyeras JP, Russell MW, Menzin J. Assessment of the economic burden of COPD in the U.S.: A review and synthesis of the literature. COPD 2006; 3(4):211–218.
- Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S. The health and productivity cost burden of the “top 10” physical and mental health conditions affecting six large U.S. employers in 1999. J Occup Environ Med 2003; 45(1):5–14.
- Mannino DM, Braman S. The epidemiology and economics of chronic obstructive pulmonary disease. Proc Am Thorac Soc 2007; 4(7):502–506.
- Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance—United States, 1971–2000. MMWR Surveill Summ. 2002; 51(6):1–16.
- Schneider KM, O'Donnell BE, Dean D. Prevalence of multiple chronic conditions in the United States’ Medicare population. Health Qual Life Outcomes 2009; 7:82.
- Maurer J, Rebbapragada V, Borson S, Goldstein K, Kunik ME, Yohannes AM, Hanania NA; ACCP Workshop Panel on Anxiety and Depression in COPD. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest 2008; 134(4 Suppl):43S–56S.
- Schane RE, Walter LC, Dinno A, Covinsky KE, Woodruff PG. Prevalence and risk factors for depressive symptoms in persons with chronic obstructive pulmonary disease. J Gen Intern Med. 2008; 23(11):1757–1762. Erratum in: J Gen Intern Med 2008; 23(11):1930.
- Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psych 2007; 29(5):409–416.
- Stein MB, Cox BJ, Afifi TO, Belik SL, Sareen J. Does co-morbid depressive illness magnify the impact of chronic physical illness? A population-based perspective. Psychol Med 2006; 36(5):587–596.
- McLaughlin T, Geissler EC, Wan GJ. Co-morbidities and associated treatment charges in patients with anxiety disorders. Pharmacotherapy 2003; 23(10):1251–1256.
- Lewis KE, Annandale JA, Sykes RN, Hurlin C, Owen C, Harrison NK. Prevalence of anxiety and depression in patients with severe COPD: similar high levels with and without LTOT. COPD 2007; 4(4):305–312.
- IMS LifeLink® Health Plan Claims Database, PharMetrics, Inc., a unit of IMS, Watertown, MA. Copyright 2009, All Rights Reserved.
- Arne M, Janson C, Janson S, Boman G, Lindqvist U, Berne C, Emtner M. Physical activity and quality of life in subjects with chronic disease: chronic obstructive pulmonary disease compared with rheumatoid arthritis and diabetes mellitus. Scand J Prim Health Care 2009; 27(3):141–147.
- Cully JA, Graham DP, Stanley MA, Ferguson CJ, Sharafkhaneh A, Souchek J, Kunik ME. Quality of life in patients with chronic obstructive pulmonary disease and co-morbid anxiety or depression. Psychosomatics 2006; 47(4):312–319.
- FitzGerald JM, Haddon JM, Bradly-Kennedy C, Kuramoto L, Ford GT; RUSIC Study Group. Resource use study in COPD (RUSIC): a prospective study to quantify the effects of COPD exacerbations on health care resource use among COPD patients. Can Respir J 2007; 14(3):145–152.
- Katon W, Lin EH, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psych 2007; 29(2):147–155.
- Lyness JM, Niculescu A, Tu X, Reynolds CF 3rd, Caine ED. The relationship of medical co-morbidity and depression in older, primary care patients. Psychosomatics 2006; 47(5):435–439.
- Fan VS, Ramsey SD, Giardino ND, Make BJ, Emery CF, Diaz PT, Benditt JO, Mosenifar Z, McKenna R Jr, Curtis JL, Fishman AP, Martinez FJ; National Emphysema Treatment Trial (NETT) Research Group. Sex, depression, and risk of hospitalization and mortality in chronic obstructive pulmonary disease. Arch Intern Med 2007; 167(21):2345–2353.
- Gudmundsson G, Gislason T, Janson C, Lindberg E, Suppli Ulrik C, Brøndum E, Nieminen MM, Aine T, Hallin R, Bakke P. Depression, anxiety and health status after hospitalisation for COPD: a multicentre study in the Nordic countries. Respir Med 2006; 100(1):87–93.
- Ng TP, Niti M, Tan WC, Cao Z, Ong KC, Eng P. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med 2007; 167(1):60–67.
- Hynninen MJ, Pallesen S, Nordhus IH. Factors affecting health status in COPD patients with co-morbid anxiety or depression. Int J Chron Obstruct Pulmon Dis 2007; 2(3):323–328.
- Felker B, Katon W, Hedrick SC, Rasmussen J, McKnight K, McDonnell MB, Fihn SD. The association between depressive symptoms and health status in patients with chronic pulmonary disease. Gen Hosp Psych 2001; 23(2):56–61.
- Carrasco-Garrido P, de Miguel-Díez J, Rejas-Gutierrez J, Martín-Centeno A, Gobartt-Vázquez E, Hernandez-Barrera V, de Miguel AG, Jimenez-Garcia R. Characteristics of chronic obstructive pulmonary disease in Spain from a gender perspective. BMC Pulm Med 2009; 9:2.
- Cao Z, Ong KC, Eng P, Tan WC, Ng TP. Frequent hospital readmissions for acute exacerbation of COPD and their associated factors. Respirology 2006; 11(2):188–195.
- Coultas DB, Edwards DW, Barnett B, Wludyka P. Predictors of depressive symptoms in patients with COPD and health impact. COPD 2007; 4(1):23–28.
- Lin PJ, Shaya FT, Scharf SM. Economic implications of co-morbid conditions among Medicaid beneficiaries with COPD. Respir Med 2010; 104(5):697–704.
- Xu W, Collet JP, Shapiro S, Lin Y, Yang T, Platt RW, Wang C, Bourbeau J. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am J Respir Crit Care Med 2008; 178:913–920.
- Mapel DW, McMillan GP, Frost FJ, Hurley JS, Picchi MA, Lydick E, Spencer MD. Predicting the costs of managing patients with chronic obstructive pulmonary disease. Respir Med 2005; 99:1325–1333.
- Eaddy M, Shah M, Lunacsek O, Stanford R. The burden of illness of hypertension and co-morbid diabetes. Curr Med Res Opin 2008; 24(9):2501–2507.
- Katon W, Cantrell CR, Sokol MC, Chiao E, Gdovin JM. Impact of antidepressant drug adherence on co-morbid medication use and resource utilization. Arch Intern Med 2005; 165:2497–2503.
- Dalal AA, Shah M, D'Souza AO, Mapel DW. COPD-related healthcare utilization and costs after discharge from a hospitalization or emergency department visit on a regimen of fluticasone propionate-salmeterol combination versus other maintenance therapies. Am J Manage Care 2011 Mar 1; 17(3):e55–65. [epub ahead of print]