Abstract
Affecting an estimated 12.6 million people and causing over 100,000 deaths per year, chronic obstructive pulmonary disease (COPD) exacts a heavy burden on American society. Despite knowledge of the impact of COPD on morbidity, mortality, and health care costs, little is known about the association of the disease with economic outcomes such as employment and the collection of disability. We quantify the impact of COPD on Americans aged 51 and older—in particular, their employment prospects and their likelihood of collecting federal disability benefits—by conducting longitudinal regression analysis using the Health and Retirement Study. Controlling for initial health status and a variety of sociodemographic factors, we find that COPD is associated with a decrease in the likelihood of employment of 8.6 percentage points (OR = 0.58, 95% CI 0.50–0.67), from 44% to 35%. This association rivals that of stroke and is larger than those of heart disease, cancer, hypertension, and diabetes. Furthermore, COPD is associated with a 3.9 percentage point (OR 2.52, 95% CI 2.00–3.17) increase in the likelihood of collecting Social Security Disability Insurance (SSDI), from 3.2% to 7.1%, as well as a 1.7 percentage point (OR 2.87, 95% CI 2.02–4.08) increase in the likelihood of collecting Supplemental Security Income (SSI), from 1.0% to 2.7%. The associations of COPD with SSDI and SSI are the largest of any of the conditions studied. Our results are consistent with the hypothesis that COPD imposes a substantial burden on American society by inhibiting employment and creating disability.
Introduction
Chronic obstructive pulmonary disease, or COPD, exacts a heavy and growing burden on American society. With an estimated 12.6 million people diagnosed, and likely at least as many undiagnosed, COPD is a common affliction (Citation1–3). COPD has just surpassed stroke as the third-leading cause of death in the United States, causing over 100,000 deaths annually (Citation4).
Numerous studies have attempted to assess the economic burden of COPD. Foster and co-authors provide a fairly recent review of the literature in the United States (Citation5). However, most studies have focused on the direct, or medical, cost burden of the illness. Moreover, the few studies that have looked at indirect costs such as reduced productivity and employment have faced some limitations, which we seek to address in this paper. Darkow and co-authors as well as Goetzel and co-authors assess the indirect costs of COPD, but their findings have limited applicability due to the non-nationally representative nature of their sample (Citation6, 7).
In contrast, Druss and co-authors provide a nationally representative assessment of the disability burden of COPD and other major illnesses, and compare that burden to the direct (medical) costs of the same conditions (Citation8). They find evidence to suggest the social burden of COPD is substantial. Using the 1996 Medical Expenditure Panel Study (MEPS), they find that COPD is associated with reduced work days and increased bed days. What is needed is evidence from more recent years that focuses on employment and disability.
In this study, we quantify three aspects of the indirect economic burden of COPD: reduced employment, increased uptake of Social Security Disability Insurance (SSDI), and increased uptake of Supplemental Security Income (SSI). The effects of an illness such as COPD on outcomes like employment and disability are difficult to accurately gauge, because illnesses are not randomly assigned to individuals but rather tend to be correlated with personal characteristics that also affect labor market outcomes. This problem is compounded in a cross-sectional data set such as the MEPS, as it is difficult to disentangle the effect of illness from the effect of personal characteristics on labor market outcomes.
For this reason, we conduct our analysis using the Health and Retirement Study (HRS), a panel data set that follows a representative sample of Americans from age 50 until death. In this setting we can more appropriately control for individual characteristics to better isolate the impact of illnesses such as COPD on employment and disability. This enables us to calculate attributable costs. In this way, we can better avoid under-reporting problems, which stem from self-reporting and identify which costs are due to COPD (or other illnesses) rather than underlying personal characteristics.
Methods
We first provide some background on the federal disability programs featured in our analysis. The Social Security Act of 1935 created a pension system to pay benefits to retirees in their old age, without any provision for workers who became disabled before retirement age. The system was reformed with the Social Security Amendments of 1954, which created the Social Security Disability Insurance (SSDI) program (Citation9). SSDI is similar to the traditional Social Security pension benefits, in that it is funded through dedicated payroll taxes and administered by the Social Security Administration. To collect SSDI, an applicant must be insured (which typically means having a long enough work history of paying Social Security payroll taxes), under the full retirement age (which is 65 for our HRS sample), and have an approved disability (Citation9). The disability must be severe enough to prevent the applicant from performing “substantial gainful activity” (Citation9).
Although the SSDI program was originally intended to provide a safety net for individuals during temporary spells of disability (Citation9), in recent years the rolls of SSDI beneficiaries have been growing, and few beneficiaries have been rehabilitated and returned to work (Citation10). As a consequence, the share of the Social Security spending going to the SSDI program (rather than pension benefits) has risen from 10.1% in 1990 to 16.6% in 2005 (Citation10). Because SSDI beneficiaries are eligible for Medicare 24 months after the onset of their disability, growing SSDI rolls have also put an increasing burden on Medicare's budget. In 2005, SSDI recipients accounted for 15.1% of Medicare beneficiaries, and that portion has been growing (Citation10).
In contrast, Supplemental Security Income (SSI) is a federal program funded with general tax revenue (rather than Social Security payroll taxes) intended to provide cash to meet basic needs for food, shelter, and clothing among the aged, blind, and disabled. Unlike SSDI, an applicant does not need to have paid Social Security payroll taxes to be eligible for SSI, although the definition of disability is similar (Citation11). Both SSDI and SSI are administered by the Social Security Administration. SSDI benefits tend to be more generous than SSI benefits (Citation9, Citation12).
We conduct our analysis using the Health and Retirement Study (HRS) (Citation13). The HRS is a long-term panel of Americans approaching and past retirement age. The survey enables researchers to study Americans’ health and socioeconomic status as they transition from their prime working years to retirement. The HRS began in 1992 with a nationally representative survey of 51-to-61 year-olds and their spouses, and has continued with follow-up surveys every two years since then. New birth cohorts have been added, and since 1998, the survey has been designed to be nationally representative of the population aged 50 and older (and their spouses), with the survey being “refreshed” with a new cohort of 50-to-55 year-olds every 6 years.
For this analysis, we used data from the nine waves of the HRS from 1992 to 2008. The birth cohorts featured in this data include the AHEAD cohort (born 1923 and earlier), the Children of the Depression, or CODA (born 1924–1930), the original HRS cohort (born 1931–1941), the War Babies (born 1942–1947), and the Early Boomers (born 1948–1953).
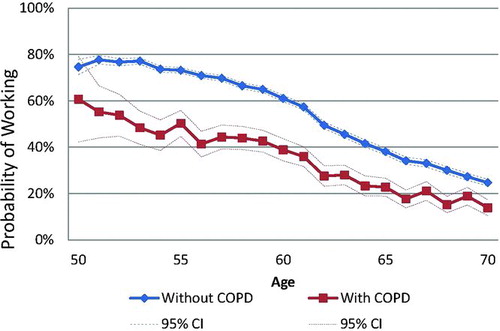
The variables contained in the HRS enable us to study employment and disability while adjusting for a variety of controls. Employment is measured by asking respondents whether they are currently working for pay. As shows, employment is highest among the youngest HRS respondents and declines with age. It is also consistently lower among respondents with COPD than those without.
Figure 1. Probability of employment by age and COPD status. Mean (unadjusted) employment probabilities among HRS respondents by age and COPD status.
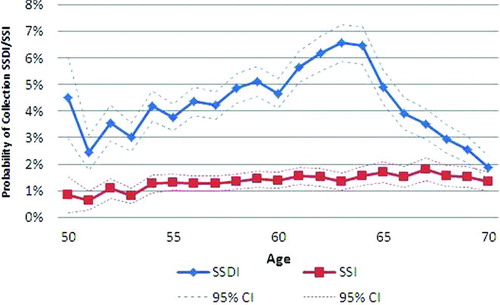
Participation in the federal Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI) programs is measured by asking respondents whether they are currently collecting either benefit. SSDI is a much larger program in terms of the number of beneficiaries, but it is mostly supplanted by Social Security pension benefits for those 65 and over (shown in ). In contrast, SSI is a much smaller program, but it is available to some people who would not be able to collect Social Security pension benefits.
Figure 2. Probability of collecting SSDI or SSI by age. Mean (unadjusted) probabilities of collecting SSDI or SSI among HRS respondents by age.
COPD is referred to as “chronic lung disease” in the HRS. Specifically, respondents are asked, “Has a doctor ever told you that you have chronic lung disease such as chronic bronchitis or emphysema?” and are specifically told not to include asthma in their response. Other common diseases are measured in the same way, by asking the respondent, “Has a doctor ever told you that you have …?” The HRS definition of COPD is quite similar to the one used in the National Health Interview Survey (NHIS).Footnote1 The NHIS is the gold standard for determining the national prevalence of various diseases (Citation14, 15). The NHIS definition of COPD has been validated by comparing its estimated prevalence to prevalence estimates obtained using spirometry (Citation16).
To explore the association of COPD and other conditions with respondents’ likelihood of employment, collecting SSDI, and collecting SSI, we performed logistic regression analyses (using the survey weights) of those three outcome variables on having COPD, other medical conditions, and an extensive set of sociodemographic and health controls. (Results were similar whether we used linear or logistic regression.) Other conditions included self-reported stroke, heart disease, cancer, diabetes, and hypertension in each HRS wave.Footnote2 (These conditions were consistently measured in the HRS over time.)
Demographic controls included Hispanic, White, Black, male, age, age squared, age upon entering panel, age upon entering panel squared, BMI, BMI upon entering panel, and education.Footnote3 In addition, sensitivity analyses included individual earnings and household assets as explanatory variables, as these are likely to have some effect on the likelihood of working or collecting disability benefits; the base case analyses excluded earnings and assets because they are likely related to unobserved factors (e.g., attitudes toward work).
To proxy for unobserved factors, we also included age and health conditions (including COPD) at baseline, that is, at the time of entering the HRS.Footnote4 As a consequence, the reported odds ratios for health conditions first reported after the baseline reflect the onset of new cases. This approach follows Michaud, Goldman, Lakdawalla, Gailey, and Zheng (Citation17). Their strategy in turn is based on work by Wooldridge (Citation18, 19). Because this approach reflects the association of COPD and other illnesses with employment and disability based on the onset of new cases, its estimates will be conservative, especially in the case of a progressive illness such as COPD. The statistical software we used to perform our analyses was Stata (version 11). For further detail on methods, see the appendix.
Results
Our final sample is comprised of 28,863 persons and 147,040 person-years. Of 4095 persons who ever had COPD in the analysis sample, 1807 had it upon entering the panel. The prevalence of COPD in the HRS varies from year to year, attaining a low of 5.4% in 1992 and a high of 11.4% in 2008 (shown in ). The 2008 NHIS prevalence of COPD, adjusted to match the age distribution of the HRS population, is 7.8%. Much of the variation in COPD prevalence in the HRS is due to the fact that the mean age varies from wave to wave, especially in the early years of the panel before it was decided in 1998 that the survey should be nationally representative of the entire U.S. population ages 50 and older.
Table 1. Prevalence of COPD in the HRS
The average HRS respondent with COPD is considerably different from the average HRS respondent without COPD, as can be seen in . The average respondent with COPD is older, less wealthy, and lower-earning than the typical HRS respondent. The average respondent with COPD is also less likely to be working for pay (39% [p < 0.001, 95% CI 37.5%–40.4%] versus 64% [p < 0.001, 95% CI 63.7%–64.4%] for respondents under 65 years) and more likely to be collecting federal disability benefits (14% [p < 0.001, 95% CI 12.8%–14.8%] versus 4.2% [p < 0.001, 95% CI 4.0%–4.3%] for SSDI collection among respondents under age 65, 4.5% [p < 0.001, 95% CI 3.9%-5.1%] versus 1.1% [p < 0.001, 95% CI 1.0%–1.2%] for SSI collection in the same age group). These statistics, while notable, do not distinguish the impact of COPD from the impact of other factors that may be related to COPD, such as age and education.
Table 2. Characteristics of the average HRS respondent by COPD status
The logistic regression analyses demonstrate that COPD is significantly associated with the likelihood of employment and the likelihood of collecting SSDI and SSI. As summarized in the first column of , individuals with COPD have 0.58 (p < 0.001, 95% CI 0.50–0.67) times the odds of working for pay compared to individuals without COPD. COPD is associated with an 8.6 percentage point reduction in the likelihood of employment (p < 0.001), from 44% to 35% (or 20% in relative terms). The relationships between the six illnesses studied and the probability of employment are illustrated in . As the figure shows, the odds ratio associated with COPD is smaller than that of cancer, diabetes, heart disease and hypertension, and rivals that of stroke.
Figure 3. Probability of employment according to the presence of COPD and other chronic conditions. * indicates a statistically significant regression coefficient for the condition at the 5% level, ** at the 1% level. Note: Results are predicted probabilities from a logistic regression of working for pay on a set of control variables using the 1992–2008 Health and Retirement Study. Controls included: Hispanic, white, black, male, age, age squared, education, BMI, year, COPD, hypertension, diabetes, cancer, and stroke. The regression also included comorbid conditions at the time of entry into the HRS. Error bars give 95% confidence intervals.
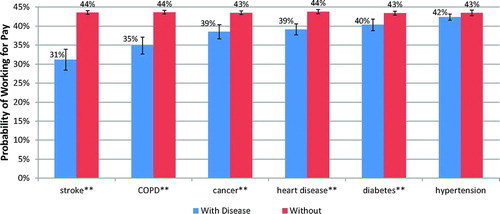
Table 3. Details of the logistic regressions with initial characteristics controls: Probability of working for pay
As a sensitivity analysis, we performed logistic regressions which included earnings and assets as controls, in addition to all the controls of the baseline specifications. When we adjusted for household assets and earned income, individuals with COPD had 0.65 (p < 0.001, 95% CI 0.57–0.75) times the odds of working for pay compared to individuals who did not have COPD. Results from the specification including assets and earnings are given in the second column of .
summarizes the association between the 6 diseases and a respondent's probability of collecting SSDI. As the table shows, an individual with COPD has over twice the odds of collecting SSDI as an individual without COPD (OR 2.52, p < 0.001, 95% CI 2.00–3.17). COPD is associated with a greater likelihood of collecting SSDI than any other condition. The next most disabling conditions are stroke (p < 0.001, OR 2.27, 95% CI 1.74–2.97) and heart disease (OR 1.98, p < 0.001, 95% CI 1.51–2.44). The large positive relationship between COPD and receipt of SSDI is apparent in , which compares the relationships between the various conditions and the likelihood of collecting SSDI. As the figure shows, COPD is associated with a 3.9 percentage point (p < 0.001), or 121%, increase in the likelihood of collecting Social Security Disability Insurance (SSDI), from 3.2% to 7.1%. Results of the sensitivity analysis, with additional assets and earnings controls, did not change the character of the results. COPD again had the largest odds ratio of the six conditions (OR 2.01, p < 0.001, 95% CI 1.60–2.52).
Figure 4. Probability of collecting SSDI according to the presence of COPD and other chronic conditions. * indicates a statistically significant regression coefficient for the condition at the 5% level, ** at the 1% level Note: Results are predicted probabilities from a logistic regression of collecting SSDI on a set of control variables using the 1992–2008 Health and Retirement Study. Controls included: Hispanic, white, black, male, age, age squared, education, BMI, year, COPD, hypertension, diabetes, cancer, and stroke. The regression also included comorbid conditions at the time of entry into the HRS. Error bars give 95% confidence intervals.
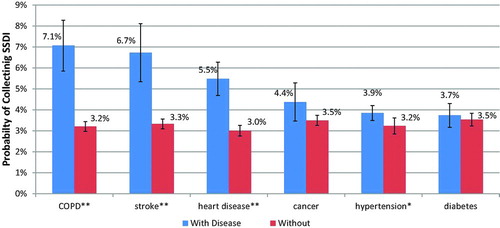
Table 4. Details of the logistic regressions with initial characteristics controls: Probability of collecting SSDI
The association between the six diseases and a respondent's probability of collecting SSI is given in Appendix . The results here are similar to the case of SSDI. COPD is associated with nearly three times the odds of collecting SSI (OR 2.87, p < 0.001, 95% CI 2.02–4.08), while the next most disabling condition is heart disease (OR 1.60, p = 0.002, 95% CI 1.19–2.15). None of the other health conditions were statistically significant in this analysis. These associations are illustrated in . As the figure shows, COPD is associated with a 1.7 percentage point (p < 0.001), or 166%, increase in the likelihood of collecting Supplemental Security Income (SSI), from 1.0% to 2.7%. Results of the sensitivity analysis, with earnings and assets controls, were similar, with COPD associated with 2.14 times the odds of collecting SSDI (p < 0.001, 95% CI 1.50–3.04). As in the baseline specification, COPD was first among the six diseases when ranked by odds ratio.
Figure 5. Probability of collecting SSI according to the presence of COPD and other chronic conditions. * indicates a statistically significant regression coefficient for the condition at the 5% level, ** at the 1% level Note: Results are predicted probabilities from a logistic regression of collecting SSI on a set of control variables using the 1992–2008 Health and Retirement Study. Controls included: Hispanic, white, black, male, age, age squared, education, BMI, year, COPD, hypertension, diabetes, cancer, and stroke. The regression also included comorbid conditions at the time of entry into the HRS. Error bars give 95% confidence intervals.
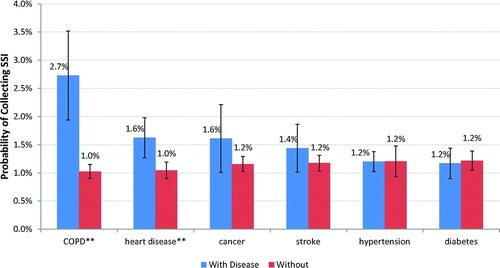
Table 5. Details of the logistic regressions with initial characteristics controls: Probability of collecting SSI
Discussion
Our results suggest that despite its seemingly lower profile, COPD is even more disabling than other important diseases such as cancer and heart disease, and rivals stroke in the burden it imposes. One might be concerned that the burden of particularly debilitating conditions, such as stroke, would be underestimated if respondents with greater deficits were less likely to be included in the survey. However, this concern is mitigated by the design of the HRS, which requires that care be taken to find proxies to respond on behalf of disabled respondents (Citation20). Therefore, our results suggest that COPD is a serious cause of disability in the United States. Yet as studies show that COPD is both underdiagnosed (Citation3) and undertreated (Citation21), there should be room to lessen this burden by identifying the affected population and providing proper treatment.
One contribution of our analysis is that it assesses the employment and disability burden of COPD and other major illnesses in a nationally representative setting. In this sense it augments what we learn from studies that quantify the costs of COPD in a less representative population, as Darkow and co-authors (Citation6) and Goetzel and co-authors (Citation7) have done.
We also update the work of Druss and co-authors, who compared the disability costs of major illnesses including COPD to their direct medical costs using the nationally representative MEPS of 1996 (Citation8). They found that, compared to other conditions, COPD was in the middle of the pack in terms of its disability impact; that is, it was neither the most nor the least disabling. This difference may reflect several factors. First, we have access to a long panel of data, which allowed us to control for a variety of factors. Second, we look at employment and disability, which–while related–are not perfectly correlated with the Druss et al. outcomes (sick days and bed days). Finally, their data come from 1996. It may be that society has done a good job mitigating the social consequences of other illnesses they found to have a greater impact.
We can use our results to provisionally estimate the impact of COPD on an aggregate basis. Our finding that COPD reduces employment by 20% translates to an 8.8 percentage point reduction in an individual's probability of working. Multiplying this reduction in the probability of working by average wages of $38,844 in 2010 (Citation22) by an estimated 12.6 million adult Americans with COPD gives an approximate $43 billion loss from reduced work among those with COPD.
Our finding that COPD causes individuals to be 121% more likely to collect SSDI translates to a 3.9 percentage point increase in the probability of collecting SSDI. Given an average annual benefit to workers of $14,507 in 2010 dollars (Citation9), this translates to a total cost to the SSDI program of over $7 billion. Similarly, our finding that COPD causes individuals to be 166% more likely to collect SSI equates to a 1.7 percentage point increase in the probability of collecting SSI. Given an average annual benefit of $6008 in 2010 (Citation12), this implies that COPD imposes an over $1 billion burden on that program.
Of course, one should exercise caution in interpreting these figures, as they project results from the aged 50-plus population to the population as a whole. However, any problems posed by this extension should be mitigated by the fact that the typical person with COPD is in fact in this age range. Therefore, when we project estimates from our aged 50-plus sample to the full COPD population, few of the people we are projecting to are actually too young to be represented by our aged 50-plus sample. Moreover, it is possible, especially in the case of the employment, that the impact of COPD could be even larger in the younger population. This would be true, for example, if people younger than 50 are in general more likely to be working than the 50-plus population, which does not seem implausible. So, it is possible that our aggregate figures are in fact underestimates.
Conclusion
Our analysis supports the hypothesis that COPD imposes a heavy burden on U.S. society. Those with COPD are less likely to work, and more likely to collect federal disability benefits, either in the form of SSDI or SSI. Our estimates suggest a steep aggregate cost. Because we obtained our estimates from the nationally representative, long-term panel data of the HRS, we were able to control for much of the unobserved personal characteristics which tend to confound estimates of indirect costs of illness. Because COPD tends to be undertreated, there is reason for hope despite the evidence of this heavy burden. Programs that identify people with COPD and improve their treatment have the potential to reap large rewards for U.S. society in terms of greater employment and reduced disability.
Declaration of Interest
This research was conducted by Precision Health Economics under contract with Novartis Pharmaceuticals. JAR has a consulting relationship with Precision Health Economics; DPG is a partner with the firm. The authors alone are responsible for the content and writing of the paper.
Notes
1 To estimate the prevalence of COPD, the NHIS asks respondents, “During the past 12 months, have you been told by a doctor or other health professional that you had chronic bronchitis?” and “Have you ever been told by a doctor or other health professional that you had emphysema?” The prevalence of chronic bronchitis and the prevalence of emphysema are added to obtain a prevalence estimate for COPD.
2 In our baseline specification, we included indicator variables for COPD, stroke, heart disease, cancer, diabetes, and hypertension during each HRS wave. In an alternative specification, we included an indicator for COPD as well as a count variable giving the number of other conditions. Results were similar.
3 Education was coded as a discrete variable indicating whether the respondent's highest level of educational attainment was less than high school (0), high school (1), or college (2).
4 Specifically, we included as covariates the values of all time-varying covariates at the time of a respondent's entry to the panel. This included dummies indicating whether the respondent had any of the six diseases at the time of panel entry.
References
- U.S. Census. Population distribution and change: 2000 to 2010 Washington, DC: U.S. Census; 2011 [cited 2011 April 15]. Available from: http://www.census.gov/prod/cen2010/briefs/c2010br-01.pdf.
- U.S. Census. USA QuickFacts from the US Census Bureau Washington, DC: U.S. Census; 2011 [cited 2011 April 15]. Available from: http://quickfacts.census.gov/qfd/states/00000.html.
- Stang P, Lydick E, Silberman C, Kempel A, Keating ET. The prevalence of COPD: using smoking rates to estimate disease frequency in the general population. Chest 2000;117(5 Suppl 2):354S–9S. Epub 2000/06/10. PubMed PMID: 10843976.
- Kochanek K, Xu J, Murphy S, Miniño A, Kung H. Deaths: Preliminary Data for 2009. Hyattsville, MD: National Center for Health Statistics, 2011 Contract No.: 4.
- Foster TS, Miller JD, Marton JP, Caloyeras JP, Russell MW, Menzin J. Assessment of the economic burden of COPD in the U.S.: a review and synthesis of the literature. COPD 2006;3(4):211–8. Epub 2007/03/17. PubMed PMID: 17361502.
- Darkow T, Kadlubek PJ, Shah H, Phillips AL, Marton JP. A retrospective analysis of disability and its related costs among employees with chronic obstructive pulmonary disease. J Occup Environ Med 2007;49(1):22–30. Epub 2007/01/12. doi: 10.1097/JOM.0b013e31802db55f 00043764–200701000-00003 [pii]. PubMed PMID: 17215710.
- Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S. The health and productivity cost burden of the “top 10” physical and mental health conditions affecting six large U.S. employers in 1999. J Occup Environ Med 2003;45(1):5–14. Epub 2003/01/30. PubMed PMID: 12553174.
- Druss BG, Marcus SC, Olfson M, Pincus HA. The most expensive medical conditions in America. Health Aff (Millwood) 2002;21(4):105–11. Epub 2002/07/16. PubMed PMID: 12117121.
- Social Security Administration. Annual statistical report on the Social Security Disability Insurance Program, 2009 Washington, DC: Social Security Administration; 2010 [cited 2011 April 1]. Available from: http://www.ssa.gov/policy/docs/statcomps/di_asr/2009/di_asr09.pdf.
- Autor DH, Duggan MG. The growth in the social security disability rolls: A fiscal crisis unfolding. J Econ Perspect 2006;20(3):71–96. PubMed PMID: ISI:000240392200004.
- Social Security Administration. Supplemental Security Income Home Page Washington, DC 2011 [cited 2011 May 1]. Available from: http://www.ssa.gov/ssi/.
- Social Security Administration. SSI Federally Administered Payments: Table 7. Average monthly payment Washington, DC: Social Security Administration; 2011 [cited 2011 March 10]. Available from: http://www.ssa.gov/policy/docs/statcomps/ssi_monthly/2011–02/table07.pdf.
- Health and Retirement Study, public use dataset. In: Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). editor. Ann Arbor, MI, 2011.
- Nelson DE, Powell-Griner E, Town M, Kovar MG. A comparison of national estimates from the National Health Interview Survey and the Behavioral Risk Factor Surveillance System. American journal of public health. 2003;93(8):1335–41. Epub 2003/08/02. PubMed PMID: 12893624; PubMed Central PMCID: PMC1447966.
- U.S. Department of Health and Human Services. Healthy People 2020 Objectives 2012 [cited 2012 February 18]. Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf.
- Mannino DM. COPD: epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest. 2002;121(5 Suppl):121S–6S. Epub 2002/05/16. PubMed PMID: 12010839.
- Michaud PC, Goldman D, Lakdawalla D, Gailey A, Zheng Y. Differences in health between Americans and Western Europeans: Effects on longevity and public finance. Soc Sci Med. 2011;73(2):254–63. Epub 2011/07/02. doi: 10.1016/j.socscimed.2011.05.027. PubMed PMID: 21719178.
- Wooldridge JM. A framework for estimating dynamic, unobserved effects panel data models with possible feedback to future explanatory variables. Econ Lett 2000;68(3):245–50. PubMed PMID: ISI:000088888100003.
- Wooldridge JM. Simple solutions to the initial conditions problem in dynamic, nonlinear panel data models with unobserved heterogeneity. J Appl Econom 2005;20(1):39–54. doi: Doi 10.1002/Jae.770. PubMed PMID: ISI:000227252400003.
- Health and Retirement Study. Survey design 2008 [cited 2012 April 4]. Available from: http://hrsonline.isr.umich.edu/sitedocs/surveydesign.pdf.
- Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax 2008;63(9):831–8. Epub 2008/08/30. doi: 63/9/831 [pii] 10.1136/thx.2007.086041. PubMed PMID: 18728206.
- Bureau of Labor Statistics. Household data annual averages: 39. Median weekly earnings of full-time wage and salary workers by detailed occupation and sex Washington, DC: Bureau of Labor Statistics; 2011 [cited 2011 April 1]. Available from: http://www.bls.gov/cps/cpsaat39.pdf.
Appendix - Analysis Details
Regressions were of the form
where logit (z) =
 Yit is the binary outcome variable (employment status, SSDI status, SSI status); ®0 is a constant; Comorbit is a vector of indicators of various diseases (COPD, stroke, heart disease, cancer, diabetes, and hypertension) with accompanying coefficient vector ®1; Demogit is a vector of demographic controls (Hispanic, white, black, male, age, age squared, age upon entering panel, age upon entering panel squared, BMI, BMI upon entering panel, education, and in some specifications, income and assets) with accompanying coefficient vector ®2; Initi is a vector of initial disease status at the time of entering the panel for the six conditions (COPD, high blood pressure, diabetes, cancer, heart disease, and stroke) with accompanying coefficient ®3, ™t is a year dummy, and ∑it is the error term. Standard errors were adjusted for repeated observations of the same individual.
Yit is the binary outcome variable (employment status, SSDI status, SSI status); ®0 is a constant; Comorbit is a vector of indicators of various diseases (COPD, stroke, heart disease, cancer, diabetes, and hypertension) with accompanying coefficient vector ®1; Demogit is a vector of demographic controls (Hispanic, white, black, male, age, age squared, age upon entering panel, age upon entering panel squared, BMI, BMI upon entering panel, education, and in some specifications, income and assets) with accompanying coefficient vector ®2; Initi is a vector of initial disease status at the time of entering the panel for the six conditions (COPD, high blood pressure, diabetes, cancer, heart disease, and stroke) with accompanying coefficient ®3, ™t is a year dummy, and ∑it is the error term. Standard errors were adjusted for repeated observations of the same individual.
The effect of COPD, heart disease, hypertension, stroke, cancer, and diabetes on employment was computed as follows: