Abstract
Objective: To evaluate the effectiveness of a screening programme for COPD in primary care. Material/Methods: Subjects aged 65 years or older registered with a general practitioner in Copenhagen were asked to complete a questionnaire on smoking status and symptoms of COPD. If they were smokers or former smokers or if morning cough with sputum and/or dyspnoea was present, subjects were defined as “at risk of COPD” and were invited to undergo spirometric examination. Results: Of the 7103 subjects who met the study criteria, 81.2% responded to the questionnaire. Of these, 58.5% were at risk of COPD. Of those at risk, 40% underwent a spirometric examination. COPD was classified as mild in 252 (42.3%), moderate in 258 (43.3%) and severe-very severe in 86 subjects (14.4%). The participation rate was significantly higher among subjects invited for spirometry at a healthcare centre compared to general practice. Conclusions: Our findings suggest that a questionnaire can be used as a screening tool to identify subjects at risk of COPD. Furthermore, the study shows that more than half the subjects aged 65 years and above were at risk of COPD and required clinical assessment. Willingness to undergo spirometric examination depends on the location of the screening.
Introduction
Chronic obstructive pulmonary disease (COPD) is a slowly progressing chronic disease characterized by airflow limitation, cough, sputum production, and dyspnoea at later stages. It is among the leading causes of chronic morbidity and mortality throughout the world and is currently the fourth-leading cause of death worldwide (Citation1–6). Underdiagnosis of COPD is a global problem, delaying adequate treatment and the possibility of preventing physical, emotional and socioeconomic consequences of the disease (Citation7–9). A recent Danish study shows that approximately 430,000 (total population of Denmark: 5.5 million people) people in Denmark have COPD, of whom only about two-thirds are diagnosed (Citation10).
COPD warrants more attention, especially in general practice. General practitioners (GP) often represent the first point of contact for a COPD patient in the healthcare system, thus providing the possibility of early diagnosis and intervention in general practice. The first Danish guidelines on the diagnosis and treatment of COPD aimed at general practice were published in 1998 (Citation11). In recent years several other guidelines, including the international GOLD guidelines, have emphasized the importance of early detection of COPD confirmed by spirometry (Citation3, Citation12–15). A Danish study from 2006 including 2549 patients, showed that spirometry data documenting the presence of airway obstruction were available in only 50% of patients diagnosed with COPD. Furthermore, it showed that severity assessment (based on FEV1 % predicted value) was available in only 30% of the patients. This low figure was observed despite more than 80% of the 154 included GPs having a spirometer in their practice (Citation16).
Early detection of COPD is crucial for promoting smoking cessation and instituting pharmacological and non-pharmacological therapy before patients reach symptomatic and costly stages of disease (Citation3,4). It is a widespread impression that the underdiagnosis of COPD and lack of spirometry measures in patients diagnosed with COPD are due to delay caused by both physician- and patient-related factors. The reasons for GPs not performing spirometry may be limited access to the equipment, lack of adequate training and time constraints (Citation8, Citation16–19). On the patients’ side, underdiagnosis might be a result of the gradual adaptation to increasing shortness of breath due to decreasing lung function and a reluctance to seek medical advice before severe symptoms or significant impairment occur (Citation9, Citation16, Citation17). Consequently, smoking often continues and by the time of diagnosis, patients will usually have lost 50% or more of their normal lung capacity (Citation3).
In previous studies, two different methods have mainly been used to increase the rate of early diagnosis of COPD: high-risk population screening and case finding. Both methods have their advantages and disadvantages (Citation20–27). The present study highlights the importance of the general practitioner's (GP) role in the early diagnosis of COPD.
Aim of the study
The first aim of the study was to assess whether a simple, postal questionnaire with six short questions can serve as a first-stage screening tool for identifying individuals at risk of COPD. The second aim was to assess whether the self-administrated questionnaire can be used to invite individuals at risk to undergo spirometric testing at their GP for an early diagnosis. Further aims were to assess the prevalence and severity of COPD in subjects tested for COPD and to assess possible differences in subjects offered spirometry at their GP's clinic and at a local healthcare centre.
Methods
Patient selection
The study was performed in the eastern part of Copenhagen, Denmark during February 2008–February 2009. The area was served by 45 general practices. Of these practices, 80% were run by single GPs and the rest by two or more partners; 55% of GPs were women. All subjects aged 65 years or older who were registered with one of the 45 general practices were selected for the study. The regional authorities provided the subjects and their addresses from the Danish Civil Registration System (CPR). A total of 8155 eligible subjects were initially identified for the study. Of these, 1052 were excluded from the study for various reasons; deceased at time of submission (366), in residential care (326), changed GP during the study period (242), other (118). The study population thus comprised 7103 subjects: 63% women and 37% men, with a mean (± SD) age of 74.7 ± 7.8 years.
The study included a simple questionnaire and a spirometric examination performed in general practice or at a local healthcare centre. shows the complete selection process.
Figure 1. Flowchart of the screening model. Number of the study population, respondents, non-respondents, study participants at risk of COPD, individuals intending/ not intending/ intention unknown, number of individuals undergoing/ not undergoing spirometry and number with and without COPD.
The Danish Scientific Ethics Committee, the Danish Data Protection Agency and the Committee of Multi-Practice Studies in General Practice approved the study.
Questionnaire
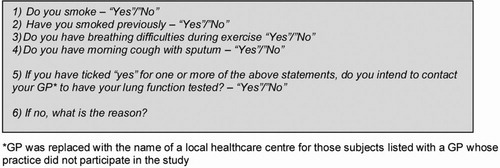
All subjects in the study population received an invitation letter by post. The letter contained a booklet about the study and general information was given about COPD, its prevalence and the relation between the disease and smoking. All subjects were asked to complete a questionnaire about their smoking status and symptoms of COPD (). Subjects were defined as being at risk if they were current or former smokers or if morning cough with sputum and/or dyspnoea was present irrespective of smoking status. Subjects who met at least one of these criteria were asked whether they intended to contact their GP or a local healthcare for a lung-function test. The intented participation was measured to assess the immediate interest in undergoing spirometry. Subjects with no smoking history or symptoms were asked to return the questionnaire with no further action. To facilitate return of the questionnaire, a pre-addressed, postage-paid envelope was included in the letter. A first (and, if necessary, a second) reminder was sent to those who did not return the questionnaire. Identification numbers were used to track respondents.
To achieve a high participation rate, advertisements were placed in local newspapers three times during the study period, and the project manager visited local senior citizen clubs to give information about the project and encourage subjects to participate.
Spirometry in General Practice or at a local healthcare centre
Study participation was voluntary for GPs. Those GPs not possessing a spirometer before study start were lent a handheld EasyOne® spirometer. Of the 45 practices, 35 agreed to perform spirometries, and of these, 17 practices used the handheld EasyOne® spirometer; the remaining practices used their own spirometers. Subjects listed with a GP whose practice did not participate in the study were requested to contact a local healthcare centre for a spirometry test. An experienced nurse performed all the tests, and the results were sent to the GP. Of the total study population, 24.5% of participants attended a healthcare centre for spirometry. No significant differences in age and sex (age: P = 0.7, sex: P = 0.3) were found between those undergoing spirometry at their GP and those attending a healthcare centre.
A 2-hour training course was held by a chief respiratory physician and 15 GPs and 9 practice nurses attended. The course included aspects of diagnosis, management of COPD, and training in spirometry as well as interpretation of the test results. Technical and methodological support was available to the participating GPs throughout the screening period. In addition to the course offer, all GPs were provided with a list of names and CPR numbers of patients invited to the study. GPs also received written instructions on how to perform spirometry and interpret results and information about medical treatment and referral procedures for pulmonary rehabilitation.
According to a scale of fees agreed upon by the Organisation of General Practitioners and the Local Health Authorities, a special fee-for-service payment for performing spirometry was created. To ensure a small economic incentive for participation, the payment for performing spirometry in the study was slightly higher than the standard compensation. The higher payment compensated GPs for collecting the necessary data and is known from the literature to have a positive effect (Citation28).
Diagnostic criteria of COPD
The spirometric parameters used in the study were: forced vital capacity (FVC), forced expiratory volume in one second (FEV1) and FEV1/FVC ratio. Post-bronchodilator FEV1 and FEV1/FVC measurements were not performed. Reference values were those of the European Respiratory Society (Citation29). Diagnosis of COPD and assessment of severity were made according to the GOLD guidelines (Citation3). In patients diagnosed with COPD, the GP was responsible for initiating medical treatment and for referral to pulmonary rehabilitation in accordance with local guidelines for COPD.
Statistical analysis
The data were analysed with the statistical program SAS. The response rate to the questionnaire and the number of people at risk were analysed using descriptive statistics. The relation between patient characteristics and location of spirometry, intention to undergo spirometry, having spirometry performed and the diagnosis of COPD were analysed with univariate logistic regression. The odds ratios were calculated and interpreted using Bland and Altman [Citation30]. Lastly, the prevalence and severity of COPD was analysed using descriptive statistics.
Results
Questionnaire response
Of the 7103 subjects, 5767 responded to the questionnaire (81.2%) (). Of these, 4173 (72.4%) returned the questionnaire after the first invitation, 1172 (20.3%) after the first reminder and 422 (7.3%) after the second reminder. There was no significant difference between respondents and non-respondents regarding age and sex (age: P = 0.9, sex: P = 0.7). The response rate to the questionnaire was not correlated to the location of the spirometric examination.
Risk of COPD
Of the 5767 subjects who responded to the questionnaire, 3376 (58.5%) were at risk of COPD. shows the correlations between smoking status and presence of symptoms. Subjects at risk of COPD are highlighted in . The prevalence of symptoms was the highest among current smokers (49.1%) and the lowest among never smokers (17.2%). Overall, 29.8% of respondents had morning cough with sputum and/or dyspnoea.
Table 1. Smoking status and presence of symptoms (subjects at risk of COPD are highlighted in the table). Numbers (N).
Intended participation among subjects at risk
Of the 3376 subjects at risk, 1931(57.2%) subjects indicated in the questionnaire that they intended to contact their GP or a local healthcare centre for a spirometric examination. However, the intended participation was significantly different between subjects invited for spirometric examination at a local healthcare centre and those invited for examination at their GP. Intended participation as the dependent variable yielded an odds ratio (OR) of 2.1 (CI = 1.8–2.5) for subjects invited for spirometric examination at a local health care centre compared with those invited for examination at their GP.
Of the 3376 subjects at risk, 1322 indicated in the questionnaire that they did not intend to undergo spirometry. These subjects gave a variety of reasons for their reluctance to participate. The main reason was “not interested” followed by “age” and “already diagnosed with COPD” (). In total, 123 subjects did not state in the questionnaire whether they intended to undergo spirometry.
Actual participation among subjects at risk
A total of 1352 spirometric tests were performed, indicating a gap between the intended participation (indicated on the questionnaire) and the actual participation rate (spirometry). Of the subjects tested, 43.4% were men and 56.6% women. The mean age was 72.5 years. The actual participation was significantly different between subjects invited for spirometric examination at a local healthcare centre and those invited for examination at their GP. Subjects invited for spirometric examination at a local healthcare centre were more likely to undergo spirometry (OR = 2.5, CI = 2.2–2.9) than those invited for examination at their GP.
shows the results of the univariate logistic regression analysis. For the intended participation, age appeared to be crucial, with a significantly lower intended participation in the older age groups compared with the age group 65–68 years (OR 0.15 versus 0.77, respectively). The same tendency was found for the actual participation, except for the age group 69–73 years where no significant difference was found compared with the reference group. With regard to sex, men were more likely to intend to participate than women were (OR 1.24). No significant sex difference was found regarding actual participation.
Table 2. Factors (odds ratios, OR and 95% confidence intervals, CI) influencing the intended participation, actual participation (spirometry) and the diagnosis of COPD. The independent variables include age, sex and smoking status with or without the presence of symptoms.
Current and former smokers with symptoms were slightly more likely to intend to participate than were never smokers with symptoms (). The same tendency was found for former smokers with actual participation as the dependent variable. However, never smokers with symptoms were significantly more likely to intend to participate and subsequently undergo spirometry than were current and former smokers without symptoms. Thus the presence of symptoms seemed to be decisive for participation.
Prevalence and severity of COPD
Of the 1352 subjects tested, 596 (44%) were diagnosed with COPD according to the GOLD classification (), indicating an overall frequency of COPD among the population of respondents of 10.3% (596*100/5767). COPD was classified as mild in 252 (42.3%), moderate in 258 (43.3%) and severe to very severe in 86 subjects (14.4%). The prevalence of COPD was related to increasing age with 37.2% diagnosed with COPD in the age group 65–68 years, 45.1% in the age group 69–73 years, 44.7% in the age group 74–78 years, 55.3% in the age group 79–83 years and 57.3% in the age group 84+ years. The overall prevalence of COPD was highest among women in all age groups except for the age 79–83 years. In general, more women than men had mild COPD and more men than women had moderate and severe to very severe COPD in all age groups with exception for the age 74–78 years (Tables and ).
Table 3. Prevalence and severity of COPD in different age groups for both men and women and in total. The number of subjects diagnosed with COPD in each age group (n) and the total number of subjects tested in the age group (N) shown in brackets.
Discussion
Interpretation of the main findings
In this study we evaluated a screening model for early detection of patients with chronic obstructive pulmonary disease. The study shows that a simple postal questionnaire can be used to identify subjects at risk of COPD. The study also shows that more than half the subjects aged 65 years and above were at risk of COPD (58.5%). Our results are consistent with the findings of other studies and highlight the need for a simple tool to assist general practitioners in identifying individuals requiring diagnostic assessment (Citation31,32).
The organisation of the screening was crucial for both the intended and actual participation. We found that the participation rate was significantly higher among subjects invited for spirometry at a local healthcare centre than among those invited for spirometry at their GP. Several factors are likely to play a role. Firstly, making an appointment for spirometry and the subsequent test are expected to be less time-consuming at healthcare centres than in general practice. Secondly, people may experience less anxiety regarding testing at healthcare centres than in general practice because GPs tend to deal more with existing illness.
Even though the participation rate was nearly 60% (56.7%) among those invited for spirometry at a healthcare centre, overall participation (40%) must be tempered by the fact that only subjects at risk of COPD received an invitation. If the participation rate is assessed in relation to the entire population aged 65 years and above, it (1352/7103*100 = 19%) is significantly lower than the participation rate obtained in other population-based screening programmes in Denmark, for example, breast cancer screening (particitation rate: 78.2%), cervical cancer screening (participation rate: 64,9%) and bowel cancer screening (participation rate: 48%) (Citation33–35). A high participation rate is crucial for the effect to be felt in a whole population and for a requirement to implement organized screening. Thus further research is needed on factors that impede or enable high participation rates before implementing organized screening programmes for COPD in general practice.
In our study, the prevalence of COPD was considerably higher than the 24.6% (age adjusted) found in another Danish study (Citation10). The difference is mainly because the ØBUS IV study used population-based sampling, whereas we recruited only patients at risk of COPD. Furthermore, smokers and former smokers with symptoms were more likely to undergo spirometry than those without symptoms, making the participation group not only at risk but at high risk of COPD.
Limitations of the study
According to WHO “Screening is the presumptive identification of unrecognized disease or defect by the application of tests, examinations, or other procedures which can be applied rapidly” (Citation36). In this respect, subjects already diagnosed with COPD should not have been invited. The reason for including these subjects was the aim to report the prevalence and severity of COPD in people aged 65 years or older in a local area of Copenhagen. Unfortunately, we do not have information on the number of people that were already diagnosed with COPD. Most people with COPD are diagnosed at their GP, and GPs in Denmark do not have an obligation to report on diagnosis to central diagnoses registries. This obligation only count for patients in hospitals.
The high prevalence of COPD found in our study can be questioned and may arise from our diagnostic criteria for COPD. Since the FEV1/FVC ratio falls with age, the use of a fixed cut-off point for defining COPD becomes more inaccurate with increasing age. Several authors have recommended the use of the lower limit of normal (LLN) to avoid misclassification (Citation37,38). Accordingly, our use of the GOLD criteria may have led to a degree of overdiagnosis of both the presence and the severity of COPD; nevertheless, the GOLD criteria were used as they were the recommendations when the study started. Furthermore, the use of spirometry without post-bronchodilator measurement may have resulted in overestimation of the prevalence of airflow obstruction (Citation3).
In Denmark there is a lack of consistently performed spirometry and spirometry training in primary care. For this reason and because of time pressures on GPs, which impact adversely on their capacity to manage patients proactively, we decided only to perform pre-bronchodilator measurements. Hill excluded people with GOLD Stage 1 disease to optimize the likelihood of identifying individuals with disease-specific impairment in health status (Citation39). If we had done this, our prevalence of COPD would have been 25.4% instead of 44%. However, taking into consideration that the prevalence increases with age and that the mean age is lower in Hill than in our study, the 25.4% is relatively close to that Hill found (20.7%).
In general, when comparing our results with those of other studies, the age of our study population has to be taken into consideration. There is a paradox between our aim of securing early detection of COPD and the focus on subjects aged 65 years and older. We were unable to change this as the study was supported by grants from the Ministry of Health and Prevention with the appropriation coming from a pool aimed at elderly people aged 65 years and above.
Conclusions
Underdiagnosis of COPD in the primary care setting is a worldwide problem. Our findings suggest that a simple postal, self-administrated questionnaire can be used as a screening tool to identify subjects at risk of COPD. Furthermore, the study showed that more than half the subjects aged 65 years and above were at risk of COPD and required clinical assessment. The high number of subjects at risk and their immediate interest in undergoing spirometry calls for a wider use of spirometry for diagnosis. The organisation of the screening seems crucial for the actual participation among subjects at risk, and further research is needed to define more clearly the reasons for the higher interest in undergoing spirometry at a local healthcare centre rather than in general practice.
Declaration of Interests
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper. AML drafted the manuscript. AML, AF, VG, MSØ, BN and VB participated in the design of the study. AF and AML obtained funding for the project. AML, VG and HLJ performed the statistical analysis. AML, AF, VG, MSØ, BN, HLJ and VB read, commented on, and approved the final version of the manuscript.
References
- WHO. World Health Report 2002. http://www.who.int/whr/2002.
- Murray CJL, Lopez AD. Alternative visions of the future: projecting mortality and disability, 1990–2020. In The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Volume 1. Edited by Murray CJL, Lopez AD. Cambridge, Massachusetts, USA: Harvard University Press; 1996:361–395.
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. [http://www.goldcopd.org] (accessed January 15, 2010).
- Celli BR, MacNee W, Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004; 23: 932–946.
- Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet 2004; 365:613–620.
- Price D, Duerden, M. Chronic obstructive pulmonary disease. The lack of a national service framework should not allow us to ignore it. BMJ 2003; 326:1046–1047.
- Den Otter JJ, Van Diijk B, Van Schayk CP, Molema J, Van Wheel C. How to avoid underdiagnosed asthma/chronic obstructive pulmonary disease? J Asthma 1998; 35:381–387.
- Freeman D, Nordyke RJ, Isonaka S, Nonikov DV, Maroni JM, Price D, Halbert RJ. Questions for COPD diagnostic screening in a primary care setting. Respir Med 2005; 99:1311–1388.
- Price DB, Tinkelman DG, Halbert RJ, Nordyke RJ, Isonaka S, Nonikov D, Juniper EF, Freeman D, Hausen T, Levy ML, Østrem A, Van der Molen T, Van Schayck CP. Symptom-based questionnaire for identifying COPD in smokers. Respiration 2006; 73:285–295.
- Løkke A, Fabricius PG, Vestbo J, Marott JL, Lange P. Forekomst af kronisk obstruktiv lungesygdom i København. Ugeskr Læger 2007; 169:3956–3960.
- Lange P, Hansen JG, Iversen M. Diagnosis and treatment of COPD. Ugeskr Læger 1998, 1.
- Sundhedsstyrelsen. KOL - Kronisk Obstruktiv Lungesygdom: Anbefalinger for tidlig opsporing, opfølgning, behandling og rehabilitering. København; 2007.
- Forløbsprogram for KOL. Hospitaler, almen praksis og kommunerne i Region Hovedstaden. http://www.regionh.dk/NR/rdonlyres/5B1B6F6B-B369-4636-82DF-01785D198CCE/0/Forloebsprogram_KOL_LR.pdf.
- KOL i almen praksis. Diagnostik, behandling, opfølgning, rehabilitering. Dansk Selskab for Almen Medicin i samarbejde med Fonden for Tidsskrift for Praktisk Lægegerning, 2008.
- Lange P, Rasmussen FV, Borgeskov H, Dollerup J, Jensen MS, Roslind K, Nielsen LM. The quality of COPD care in general practice in Denmark: the KVASIMODO Study. Primary Care Respir J 2007; 16(3):174–181.
- Van den Boom G, Rutten-van Molken MP, Tirimanna PR, Van Schayck CP, Folgering H, Van Weel C. Association between health-realted quality of life and consultation for respiratory symptoms: results from the DIMCA programme. Eur Respir J 1998; 11:67–72.
- Van Schayck CP, Van der Heijden FMMA, Van den Boom G, Tirimanna P, Van Herwaarden CLA. Underdiagnosis of asthma: is the doctor or the patient to blame? The DIMCA project. Thorax 2000; 55:562–565.
- Clotet J, Gómez-Arbonés X, Ciria C, Albalad JM. Spirometry Is a good method for detecting and monitoring chronic obstructive pulmonary disease in high-risk smokers in primary health care. Arch Bronconeumol 2004; 40(4):155–159.
- Chavannes N, Schermer T, Akkermans R, Jacobs JE, Van de Graaf G, Bollen R, Van Schayck O, Bottema B. Impact of spirometry on GPs diagnostic differentiation and decision-making. Respir Med 2004; 98(11):1124–1130.
- DeJong SR, Veltman RH. The effectiveness of a CNS-led community-based COPD screening and intervention program. Clin Nurse Spec 2004; 18(2):72–79.
- Stratelis G, Jakobsson P, Molstad S, Zetterstrom O. Early detection of COPD in primary care: screening by invitation of smokers aged 44 to 55 years. Br J Gen Pract 2004; 54:201–206.
- Tinkelman DG, Price DB, Nordyke RJ, Halbert RJ. COPD screening efforts in primary care: what is the yield? Primary Care Respir J 2007; 16(1):41-48.
- Hansen JG, Pedersen L, Overvad K, Omland Ø, Jensen HK, Sørensen HT. Prævalensen af kronisk obstruktiv lungesygdom –sekundærpublikation. Ugeskr Læger 2009; 171(41):2986.
- Vandevorde J, Verbanck S, Gijssels L, Schuermans D, Devroey D, De Backer J, Kartounian J, Vincken W: Early detection of COPD: A case finding study in general practice. Respir Med 2007; 101:525–530.
- Vrijhoef HJM, Diederiks JPM, Wesseling GJ, Van Schayck CP, Spreeuwenberg C. Undiagnosed patients and patients at risk for COPD in primary health care: early detection with the support of non-physicians. J Clin Nurs 2003; 12:366–373.
- Van Schayck CP, Loozen JMC, Wagena E, Akkermans RP, Wesseling GJ. Detecting patients at a high risk of developing chronic obstructive pulmonary disease in general practice: cross sectional case finding study. BMJ 2002; 324:1370–1374.
- Smith-Sivertsen T, Rortveit G. Should general practitioners screen smokers for COPD? Scand J Prim Health Care 2004; 22:196–201.
- Hickson GB, Altemeier WA, Perrin JM. Physician reimbursement by salary or fee-for-service: effect on physician practice behavior in a randomized prospective study. Pediatrics 1987; 80(3):344–350.
- Quanjer PHH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. Eur Respir J 1993; 6(16):5–40.
- Bland JM, Altman DG. The odds ratio. Br Med J 2000; 320:1468.
- Price D, Freeman D, Cleland J, Kaplan A, Cerasoli F. Earlier diagnosis and earlier treatment of COPD in primary care. Primary Care Respir J 2011; 20(1):15–22.
- Price DB, Tinkelman DG, Halbert RJ, Nordyke RJ, Isonaka S, Nonikov D, Juniper EF, Freeman D, Hausen T, Levy ML, Østrem A, Molen T, Schayck CP. Symptom-based questionnaire for identifying COPD in smokers. Respiration 2006; 73:285–295.
- Styregruppen for DKMS. Årsrapport DKMS 2010 vedr. den første nationale screeningsrunde. Dansk Kvalitetsdatabase for Brystkræftscreening. Denmark, 2010.
- Styregruppen for DKLS. Årsrapport DKLS 2010. Dansk Kvalitetsdatabase for Livmoderhalskræftscreening. Denmark, 2011.
- Sundhedsstyrelsen. Screening for tarmkræft. Deltagelsesprocentens betydning –En medicinsk teknologivurdering. København, 2008.
- Wilson JMG, Junger G. Principles and practice of screening for disease. In Public Health Papers, 34. Geneva: World Health Organisation, 1968.
- American Thoracic Society. Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis 1991; 144(5):1202–1218.
- Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, Grinten CPM, Gustafsson P, Hankinson J, Jensen R, Johnson DC, MacIntyre N, McKay R, Miller MR, Navajas D, Pedersen OF, Wanger J. Interpretative strategies for lung function tests. Eur Respir J 2005; 26(5):948–968.
- Hill K, Goldstein RS, Guyatt GH, Blouin M, Tan WC, Davis LL, Heels-Ansdell DM, Erak M, Bragaglia PJ, Tamari IE, Hodder R, Stanbrook MB. Prevalence and underdiagnosis of chronic obstructive pulmonary disease among patients at risk in primary care. CMAJ 2010; 182(7):673–678.