Abstract
Background: Persons with chronic obstructive pulmonary disease (COPD) and/or asthma have great risk for morbidity. There has been sparse state-specific surveillance data to estimate the impact of COPD or COPD with concomitant asthma (overlap syndrome) on health-related impairment. Methods: The North Carolina (NC) Behavioral Risk Factor Surveillance System (BRFSS) was used to assess relationships between COPD and asthma with health impairment indicators. Five categories [COPD, current asthma, former asthma, overlap syndrome, and neither] were defined for 24,073 respondents. Associations of these categories with health impairments (physical or mental disability, use of special equipment, mental or physical distress) and with co-morbidities (diabetes, coronary heart disease, stroke, arthritis, and high blood pressure) were assessed. Results: Fifteen percent of NC adults reported a COPD and/or asthma history. The overall age-adjusted prevalence of any self-reported COPD and current asthma were 5.6% and 7.6%, respectively; 2.4% reported both. In multivariable analyses, adults with overlap syndrome, current asthma only, and COPD only were twice as likely as those with neither disease to report health impairments (p < 0.05). Compared to those with neither disease, adults with overlap syndrome and COPD were more likely to have co-morbidities (p < 0.05). The prevalence of the five co-morbid conditions was highest in overlap syndrome; comparisons with the other groups were significant (p < 0.05) only for diabetes, stroke, and arthritis. Conclusions: The BRFSS demonstrates different levels of health impairment among persons with COPD, asthma, overlap syndrome, and those with neither disease. Persons reporting overlap syndrome had the most impairment and highest prevalence of co-morbidities.
| Abbreviations | ||
| BMI Body mass index | = | |
| BRFSS Behavioral Risk Factor Surveillance System | = | |
| CDC Centers for Disease Control and Prevention | = | |
| COPD Chronic obstructive pulmonary disease | = | |
| SOB Shortness of breath. | = | |
Introduction
Due to the burden of chronic obstructive pulmonary disease (COPD) and asthma, defining and monitoring the prevalence and impact of these diseases is an important goal in healthcare (Citation1,2). In 2011, the Centers for Disease Control and Prevention (CDC) reported that chronic lower respiratory diseases, primarily COPD and asthma, surpassed stroke as the third-leading cause of death in the United States (Citation3), earlier than predicted (Citation4). In addition to the impact of COPD on healthcare costs and mortality, it is a leading cause of disability (Citation5–20).
Co-morbidities are common in COPD secondary to the advanced age of the typical patient, adverse health effects of tobacco, and because COPD is a systemic disease affecting multiple organ systems (Citation21–23). Asthma has been reported to be present in 20–40% of COPD patients (Citation24–27), and along with cardiovascular disease (Citation28, 29) are some of the most important co-morbidities in COPD as evidenced by more adverse clinical outcomes than COPD alone (Citation24–30).
The CDC (Citation31) and the Institute of Medicine (Citation32) recently published recommendations to expand COPD surveillance in the United States. The Behavioral Risk Factor Surveillance System (BRFSS) is a general population health survey used to define health behaviors and chronic diseases in U.S. adults and has been used for many years to define the epidemiology of asthma in the United States. As the BRFSS addresses many issues from the patient's perspective, it could provide substantial insight into COPD and relevant co-morbidities. In 2007 and 2009, the North Carolina (NC) COPD Taskforce and the State Center for Health Statistics of NC used the BRFSS to define the burden of COPD and has been reported elsewhere (Citation33). In this report, data from the NC BRFSS was used to examine characteristics and health-related impairment of persons with COPD, asthma, and concomitant COPD and asthma (overlap syndrome).
Methods
Survey
The 2007 and 2009 NC BRFSS questionnaires contained > 90 core health-related questions (including asthma prevalence) as well as the addition of COPD prevalence and impact questions (). Using a scripted BRFSS, trained interviewers collected data using an independent random-digit dialed probability sample of households through landline telephones. Persons in group homes or institutions were not included in the sample of non-institutionalized persons. A 5% random selection of completed surveys was validated by a separate interviewer for selected questions. In addition, the NC BRFSS oversampled 23 of the state's largest counties and Native American census tracts in six counties because of small sample size in these categories, and apportioned the remainder of the sample to three regions of the state: the Western, Piedmont and Eastern regions.
Table 1. Questions related to obstructive airways disease: Behavioral Risk Factor Surveillance System (BRFSS): North Carolina, 2007 and 2009
The BRFSS protocol includes up to 15 phone call attempts to individual respondent's telephone numbers. Response rates are calculated from those who are contacted and complete the survey; cooperation rates are calculated from those who are contacted and agree to do the survey. A detailed description of the survey's design and random sampling procedures is available elsewhere (Citation34). The response and cooperation rates from eligible households for NC in 2007 and 2009 were 55% and 62%, respectively and 75% and 80%, respectively (Citation35, 36) A cooperation rate less than 65% indicates a problem with interviewing techniques. The BRFSS has been approved as exempt research by the CDC's institutional review board.
Analysis
Of the 28,054 respondents in the combined surveys, there were 24,073 who had complete information for COPD, asthma history, current asthma, socio-demographic characteristics, cigarette smoking, body mass index, co-morbid conditions, and health-related impairment. Five obstructive airway disease categories were defined by responses to COPD and asthma prevalence questions ().
Table 2. Distribution of selected characteristics of the adult study population, aged ≥18 years: North Carolina, 2007 and 2009
Former asthma history only was defined as those who had ever reported having asthma but did not currently have either any history of asthma or COPD. COPD-asthma overlap syndrome was defined if the respondent answered affirmatively to both COPD and asthma questions. The age-adjusted prevalence (standardized to 2000 U.S. census population) of the five obstructive airway disease categories were similar between 2007 and 2009 (using pair-wise linear contrast t-test, p > 0.05); thus, data from the two survey years were combined.
For respondents reporting having COPD, we also compared between those with and without concomitant asthma, the percentage who agreed that shortness of breath (SOB) affected their quality of life and the percentage who reported having their condition diagnosed with a breathing test. Impaired health for each indicator was defined if the respondent reported ≥ 14 days in last 30 days for mental, physical, emotional impairment or use of special medical equipment. Disability was defined if the respondent reported being limited in any way in any activities because of physical, mental, or emotional problems. Body mass index (BMI) was calculated based on self-reported weight and height.
Respondents were also asked a series of questions () about whether they had ever been told by a health professional that they had diabetes, stroke, coronary heart disease (myocardial infarction, heart attack, coronary heart disease, or angina), high blood pressure, or arthritis (arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia). Women who reported high blood pressure or diabetes only during pregnancy and persons reporting having borderline high blood pressure, pre-hypertension, borderline diabetes, or pre-diabetes were not defined as having those co-morbid conditions.
For the statistical analyses, we first examined the distribution of selected characteristics in our study population. The comparison of the age-adjusted prevalence of obstructive airway disease categories among subgroups of the selected characteristics was also assessed. In addition, we also compared the age-adjusted percentage of each health impairment indicator, co-morbid conditions, and cigarette smoking between groups defined by obstructive airway disease category. Finally, we assessed the association of the various obstructive airway disease categories with each health impairment indicator and co-morbid condition.
The prevalence ratio (PR) and 95% confidence interval (CI) for each association were obtained from separate multivariate logistic regression models that included respiratory categories, age, sex, race/ethnicity, education, health care coverage, physician routine checkup status, and smoking status. All analyses were performed using SAS-callable SUDAAN (version Citation10, Research Triangle Institute, Research Triangle Park, NC) to account for the complex sampling design. The statistical significance level is denoted at 0.05.
Results
Distributions of respondent demographics, healthcare access, health-related impairment indicators, smoking status, BMI, co-morbid conditions, and obstructive airway disease categories are shown in . Based on 2010 U.S. census data in NC (Citation37), the 2007 and 2009 NC BRFSS represented an appropriate cross-section of NC adults based on a similar proportion of gender, age, race, and education levels. The overall prevalence of self-reported COPD, current asthma, and ever asthma were 5.6%, 7.6%, and 12.1%, respectively. Notably, among the 1,948 respondents with self-reported COPD, 41.4% reported COPD-asthma overlap syndrome. shows the prevalence of each obstructive airways disease category by age. Those reporting either former asthma or current asthma without concomitant COPD decreased between ages 18–44 and ages 45–54 years ( p < 0.05), whereas the prevalence of those with COPD only and those with overlap syndrome increased among successive age groups up until ages 65–74 years ( p < 0.05) where the prevalence appeared to decrease.
Figure 1. Prevalence (%) of selected obstructive airway disease categories among adults aged ≥18 years, by age groups: North Carolina, 2007 and 2009.
We further examined differences in the age-adjusted prevalence of each obstructive airway disease category by selected characteristics (). There were no differences in the prevalence of having former asthma only between groups defined by any of the selected characteristics ( p > 0.05). However, the prevalence of current asthma only was higher in women than men, Blacks than Whites, non-Hispanics than Hispanics, obese than non-obese, persons with a high school education than those with 4 or more years of college, and persons with arthritis than those without arthritis ( p < 0.05). In contrast, the age-adjusted prevalence of having COPD only decreased with increasing educational level, was higher in persons with coronary heart disease, arthritis, high blood pressure than in adults without those respective conditions, and was higher either in current smokers or former smokers compared to never smokers ( p < 0.05).
Table 3. Age-adjusted prevalence of obstructive airway disease categories among adults aged ≥18 years, by selected characteristics: North Carolina, 2007 and 2009
The age-adjusted prevalence of overlap syndrome was significantly higher in persons with obesity, coronary heart disease, stroke, diabetes, arthritis, or high blood pressure than persons without the respective co-morbid condition ( p < 0.05); in current smokers and former smokers than never smokers ( p < 0.05); and decreased with increasing educational level ( p < 0.05). Health care coverage and time since last routine doctor visit were not associated with any of the obstructive airway disease categories.
Notably, a significantly greater percentage ( p < 0.05) of a history of cigarette smoking was reported by respondents with COPD only (77.1%; 95% CI = 72.7–81.5%) and with overlap syndrome (71.5%; 95% CI = 65.1–77.9%) compared to those with a former asthma history only (51.8%; 95% CI = 46.3–57.3%), current asthma only (45.7%; 95% CI = 41.1–50.3%), or neither respiratory disease (45.7%; 95% CI = 44.6–46.9%). The prevalence of current smoking was significantly higher (p < 0.05) for overlap syndrome (41.4%; 95% CI = 32.7–50.0%) and COPD only (48.9%; 95% CI = 41.1–56.7%) compared to persons with neither respiratory disease (20.4%; 95% CI = 19.4–21.4%), but was not significantly different among those with current asthma only (21.8%; 95% CI = 18.0–25.7) or those with former asthma only (25.2%; 95% CI = 20.1–30.3%).
The age-adjusted prevalence of disability and requiring special equipment was significantly higher in the overlap syndrome compared to that in other categories ( and ) ( p < 0.05). Persons with the overlap syndrome also had a significantly higher prevalence of frequent mental distress and frequent physical distress than all other groups ( p < 0.05) except for those with COPD only. Adults with COPD only also did not differ significantly from those with current asthma only in terms of the four health impairment variables but both of these groups had higher age-adjusted levels of disability than persons with neither obstructive airway disease compared to persons with former asthma or no obstructive airway disease ( p < 0.05).
Figure 2. Age-adjusted percent (%) of adults aged ≥18 years reporting frequent mental distress, frequent physical distress, disability, and/or limitations requiring special equipment, by selected obstructive airway disease categories, North Carolina, 2007 and 2009.
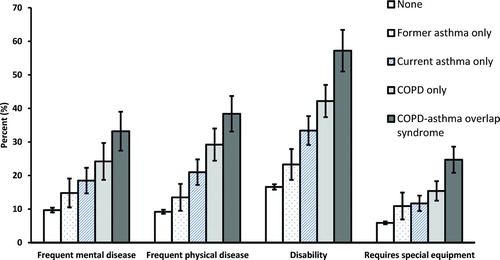
Table 4. Age-adjusted prevalence and adjusted prevalence ratio of selected health impairments and co-morbid conditions among adults aged ≥18 years, by obstructive airway disease categories: North Carolina, 2007 and 2009
In multivariable analyses, persons with either overlap syndrome or COPD only had twice the likelihood of frequent mental distress, frequent physical distress, disability, and a requirement for special equipment compared to adults with no airway disease (p < 0.05). Persons with current asthma only were over 75% more likely to also have frequent mental distress, frequent physical distress, disability, and to require special equipment than persons with no airway disease (p < 0.05) in multivariable analyses. Compared to persons with no airway disease, those with only a former history of asthma were also 87% more likely to require special equipment.
We examined the age-adjusted prevalence of other co-morbid conditions by obstructive airway disease categories ( and ). Persons with overlap syndrome had the highest age-adjusted prevalence of each co-morbid condition but comparisons with all four other obstructive airway groups reached statistical significance (p < 0.05) only for diabetes, stroke, and arthritis. Persons with COPD only had a significantly higher age-adjusted prevalence of coronary heart disease than persons with neither obstructive disease or persons in both asthma groups (p < 0.05). Compared to persons with neither obstructive disease, those with overlap syndrome and those with COPD were more likely to have coronary heart disease, stroke, arthritis, and high blood pressure after adjustment for other covariates (p < 0.05). Compared to persons with no obstructive airway disease, adults with current asthma only were more likely to have diabetes, coronary heart disease, and arthritis (p < 0.05).
Figure 3. Age-adjusted percent (%) of adults aged ≥18 years reporting co-morbidities, by selected obstructive airway disease categories, North Carolina, 2007 and 2009.
The age-adjusted prevalence of answering affirmatively that SOB affected their quality of life was higher among those with overlap syndrome (75.9%; 95% CI = 67.8–84.1%) than those with COPD only (56.6%; 95% CI = 49.3–63.9) ( p < 0.05). The prevalence of having a breathing test was not statistically different in persons with overlap syndrome (79.8%; 95% CI = 70.5–89.1%) compared to those with COPD only (65.7%; 95% CI = 58.0–73.4%).
Discussion
Using the NC BRFSS, we found that approximately 1 in 7 adults reported having COPD, asthma, or both. Tobacco use was frequent as approximately half of all adults and three-fourths of those with COPD and overlap syndrome reported a history of cigarette use. The prevalence of COPD only and overlap syndrome increased with advancing age, declined with educational attainment, were higher among persons who currently smoked, and were higher among those with coronary heart disease, arthritis, and high blood pressure. The age-adjusted prevalence of overlap syndrome was also significantly higher among persons with stroke, obesity, and/or diabetes. We found that disability, health impairment, and co-morbid conditions were common in adults with COPD or current asthma and were most pronounced in persons with overlap syndrome.
The BRFSS, an annual telephone health survey coordinated by the CDC and conducted by each state, has been used to help define the epidemiology of key chronic diseases in the US including asthma. It is a unique COPD surveillance tool because of the following: (Citation1) a large number of adults are surveyed (nationally ∼ 450,000); (Citation2) it includes a wide range of demographic and health-related questions; (Citation3) survey results are from the patient's perspective, and (Citation4) the survey is state-based. We incorporated a COPD prevalence question and impact module into the 2007 and 2009 NC BRFSS to help define the burden of COPD in NC. The overall age-adjusted prevalence of self-reported COPD (5.6%) and ever asthma (12.1%) are consistent with most other studies in the general US adult population (Citation1, Citation5, Citation38). These prevalence rates principally reflect persons with diagnosed COPD and/or asthma because of the survey questions’ wording (“Have you ever been told by a doctor…?) and the high proportion of persons reporting diagnostic breathing tests (66% with COPD only and 80% with overlap syndrome), thus underestimates the true prevalence of disease.
In 2011, the prevalence question and COPD module was adopted into all states’ BRFSS, and the overall prevalence of COPD was reported to be 6.1% in the United States (range 3.1–9.9%) and 6.9% in North Carolina (Citation39). Changes in respondent selection, expansion of sample selection to cellular telephone respondents, and changes in statistical weighting in 2011 likely explain the higher prevalence of COPD in 2011 than that reported in 2007 and 2009, particularly with regards to the prevalence of COPD in females.
There were important differences in subject characteristics among the North Carolina adults reporting asthma, COPD, and overlap syndrome. When evaluating the prevalence of disease according to age, current asthma remained stable after 45 years of age; former asthma tended to decline slightly with aging; whereas COPD only and overlap syndrome increased with age (). This suggests that when addressing both COPD and asthma in the same general population, some persons with asthma ultimately get a co-diagnosis of COPD.
More recently, a National Health Interview Survey showed the prevalence of asthma higher in teens as compared to older adults and the prevalence of asthma remained at 8% beginning in the mid-20s (Citation40). Another study in Finland reported the prevalence of asthma increased from early adulthood through ages ≥70 years (Citation41). None of these studies attempted to address the prevalence of COPD; therefore we speculate that it is possible that these studies were reporting some patients with overlap syndrome, which would explain why the prevalence of asthma did not decline with age.
There were apparent differences with regards to gender and race. In U.S. studies, adult asthmatics (Citation38) and COPD (Citation1, Citation5) are more likely to be female than male. The COPDGene study reported that persons with concurrent asthma and COPD were predominantly Black females (Citation30). Thus, it appears that a significant portion of females in the COPD population may have overlap syndrome, especially among those that have a smoking history; this may be a contributing factor to the rising prevalence and impact of COPD in women. The overlap syndrome was associated with obesity, consistent with others that have reported associations of asthma with obesity (Citation12, Citation42). The relationship between obesity, airway obstruction and restriction, as well as obstructive sleep apnea is complex and requires further investigation (Citation43).
As seen in other studies (Citation44–48), our state-based epidemiological data demonstrates that co-morbidities are common in COPD, in particular cardiovascular disease, diabetes, stroke and arthritis. This difference was more evident in those with overlap syndrome. Patients with overlap syndrome in the COPDGene study were more likely to be frequent healthcare utilizers and had a greater degree of air trapping than those with COPD alone (Citation30). A recent study in Spain reported that multiple co-morbidities, based on a higher Charlson co-morbidity index, were more frequent in those with overlap syndrome versus those with COPD alone (Citation47). In that study, when considering individual co-morbidities, only diabetes mellitus was more common in the overlap syndrome group.
Socioeconomics appeared to play an important role in the likelihood of tobacco use and thus development and impact of both COPD and overlap syndrome. In our study, 21.4%, 48.9%, 41.4% of persons with current asthma alone, COPD alone, and overlap syndrome, respectively, continued to smoke cigarettes despite relatively poor quality of life. Based on the 2009 NC BRFSS, adults with less than a high school education had 3 times higher rates of tobacco use than those with a college education (Citation49). Consistent with our study, others have reported that lower socioeconomic status is associated with higher COPD prevalence (Citation50–52).
A previous BRFSS study reported current smoking history was an important risk factor for poorly controlled asthma (Citation53). Tobacco use in asthma patients is known to lead to the development of chronic airflow obstruction but asthma has been found to be a significant risk factor for the subsequent development of COPD, even after adjusting for smoking history (Citation54). Tobacco cessation and other targeted strategies are imperative, especially in high-risk groups.
Few studies have compared health impairment between persons with and without COPD in population-based samples (Citation15, Citation47). In a population based study, strong inverse associations were found between physical and mental quality of life and the number of respiratory symptoms as well as with presence of COPD or impaired lung function (Citation15). A population based study in Spain reported that 17.4% of COPD patients had concomitant asthma, and these patients had worse respiratory-specific quality of life than COPD alone (Citation47).
Our study shows general measures of impaired health were worse in persons with COPD alone compared to persons with neither COPD nor asthma; and was most evident in overlap syndrome. Specific to obstructive lung disease, the measure of SOB was significantly worse in overlap syndrome than COPD alone. In the North Carolina BRFSS, half of persons with COPD and three-fourths of those with overlap syndrome reported that SOB affected their quality of life. One study suggested that respiratory symptoms were a better predictor of poor health-related quality of life than Global Initiative for Chronic Obstructive Lung Disease stage (Citation14), thus our question regarding SOB appears to be a reasonable measure of health impairment in COPD. However, with regards to SOB, we were unable to compare persons with asthma alone to those with COPD or overlap syndrome, as this question was only asked of respondents who had any history of COPD.
A number of studies have reported that persons with concurrent asthma and COPD have more severe disease, more substantial health impairment, and greater healthcare utilization than those with COPD only (Citation30, Citation55, Citation56). In the COPDGene study, COPD + asthma patients had greater health impairment than COPD alone based on the St George's Respiratory Questionnaire (Citation30). We previously reported that persons from the 2007 survey with concomitant asthma and COPD were more frequent utilizers of healthcare based on emergency department/hospital visits or prednisone use (Citation57).
The label of concomitant disease could occur for a variety of the following reasons including: 1) asthmatics who are long-term smokers, 2) patients who have both diseases as defined by clinical and other information, exclusive of tobacco use, such as severe long-term asthma, 3) patients who are frequent healthcare utilizers may be more likely to get multiple diagnoses by multiple providers, and/or 4) persons with both diseases who may reflect a COPD or asthma phenotype and who has wheezing and/or chronic productive cough.
In conclusion, BRFSS data provides significant insight into COPD, asthma, and the overlap syndrome. There were clear differences among these conditions with regards to age, gender, race, education level, and tobacco history. Compared to persons with no COPD nor asthma, persons with asthma or COPD had a greater prevalence of co-morbid conditions and more adverse health impairment as defined by mental distress, physical distress, disability, and use of special equipment. Persons with overlap syndrome were also more likely to report that SOB affected their quality of life, as compared to COPD alone. Clearly, clinical studies of obstructive lung diseases in adults should include patients with overlap syndrome. With the incorporation of the COPD prevalence question into every state's BRFSS (2011–2013), significant insight can be gained into patient characteristics and the burden of these diseases at national and state levels.
Declaration of Interests Statement
The authors report the following: RAP: Speaker for Astra Zeneca, Boehringer Ingelheim, Novartis, Pfizer: JOA: Advisory Board for Astra Zeneca and Glaxo Smith Kline; JBC: No conflicts of interest; YL: No conflicts of interest; MK: Research Grants: National Institutes of Health, Genentech, GlaxoSmithKline, Merck, Asthmatx (Boston Scientific), Eumedics, and Novartis. Stipend from American thoracic Society for leadership role; JFD: Consultant/advisor: Glaxo Smith Kline, Boehringer Ingelheim, Forest, Novartis, Mylan, and Sunovion. Research Grant Aerocrine; and HLK: No conflicts of interest.
No funding was associated with the conduct of this survey/study. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
All authors were involved in the development, conduct, and interpretation of study methods and manuscript development. The authors alone are responsible for the content and writing of the paper.
References
- Mannino DM, Buist AS. Global burden of COPD risk factors, prevalence, and future trends. Lancet 2007; 370:765–773.
- Meltzer EO, Blaiss MS, Nathan RA, Asthma burden in the United States: Results of the 2009 asthma insight and management survey. Allergy Asthma Proc. 2012; 33(1):36–46.
- Kochanek KD, Xu JQ, Murphy L, Deaths, preliminary data for 2009. Natl Vital Stat Report. 2011; 59(4). US Dept of Health and Human Services, CDC, National Center for Health Statistics; 2011. Available at http://www.cdc.gov/nchs/nvsr/nvsr59/nvsr59_04.pdf
- Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: global burden of disease study. Lancet 1997; 349:1436–1442.
- Akinbami LJ, Liu X. Chronic obstructive pulmonary disease among adults aged 18 and over in the United States, 1998–2009. NCHS data brief, no 63. Hyattsville, MD: National Center for Health Statistics, 2011.
- Verbugge LM, Patrick DL. Seven chronic conditions: their impact on US adults’ activity levels and use of medical services. Am J Public Health 1995; 85:173–182.
- Bousquet J, Khaltaev (eds). Global Surveillance, Prevention, and Control of Chronic Respiratory Diseases: a Comprehensive Approach. World Health Organization; 2007 Available at http://www.who.int/gard/publications/GARD%20Book%202007.pdf
- Eisner MD, Iribarren C, Blanc PD, Development of disability in chronic obstructive pulmonary disease: beyond lung function. Thorax 2011; 66:108–114.
- Braido BF, Baiardini I, Menoni S, Disability in COPD and its relationship to clinical and patient-reported outcomes. Curr Med Res Opin 2011; 27:981–986.
- Zhang MWB, Ho RCM, Cheung MWL, Prevalence of depressive symptoms in patients with chronic obstructive pulmonary disease: a systematic review, meta-analysis and meta-regression. Gen Hosp Psychiatry 2011; 33:217–223.
- Katz PP, Juliam LJ, Omachi TA, The impact of disability on depression among individuals with COPD. Chest 2010; 137:838–845.
- Cecere LM, Littman AJ, Slatore CG, Obesity and COPD: Associated symptoms, health-related quality of life, and medication use. J Chronic Obstruct Pulm Disease 2011; 8:275–284.
- Brown DW, Pleasants R, Ohar JA, Health-related quality of life and chronic obstructive pulmonary disease in North Carolina. N Am J Med Sci 2010; 2:60–65.
- Tsiligianni I, Kocks J, Tisanikas N, Siafakas N. Factors that influence disease-specific quality of life or health status in patients with COPD: a systematic review and meta-analysis Pearson correlations. Prim Care Res J 2011; 20:257–268.
- Voll-Aanerud M, Eagan TM, Wentzel-Larsen T, Respiratory symptoms, COPD severity, and health related quality of life in a general population sample. Respir Med 2008; 102:399–406
- Wijnhoven HA, Kriegsman DM, Hesselink AE, The influence of co-morbidity on health-related quality of life in asthma and COPD patients. Respir Med 2003; 97:468–475.
- Katsura H, Yamada K, Kida K. Both generic and disease specific health-related quality of life are deteriorated in patients with underweight COPD. Respir Med 2005; 99:624–630.
- Omachi TA, Katz PP, Elin EH Depression and health-related quality of life in chronic obstructive pulmonary disease. Am J Med 2009;122:778.e9-778.e15.
- Eisner MD, Iribarren C, Blanc PD, Development of disability in chronic obstructive pulmonary disease: beyond lung function. Thorax 2011; 66:108–114.
- Garcia-Rio F, Lores V, Mediano O, Daily physical activity in patients with chronic obstructive pulmonary disease is mainly associated with dynamic hyperinflation. Am J Resp Crit Care Med 2009; 180:506–512.
- Augusti A, Soriano JB. COPD as a systemic disease. COPD 2008; 5:133–138.
- Patel ARC, Hurst JR. Extrapulmonary co-morbidities in chronic obstructive pulmonary disease: state of the art. Expert Rev Respir Med 2011; 5:647–662.
- Barnes P, Celli B. Systemic manifestations and co-morbidites in COPD. Eur Resp J 2009; 33:165–85
- Shaya FT, Dongyi D, Akazawa MO, Burden of concomitant asthma and COPD in a Medicaid population. Chest 2008; 134:14–19.
- Mapel DW, Dutro MP, Marton JP, Identifying and characterizing COPD patients in US managed care: a retrospective, cross-sectional analysis of administrative claims data. BMC Health Services Res 2011; 11:43.
- Blanchette CM, Gutierrez B, Ory C, Economic burden in direct costs of concomitant chronic obstructive pulmonary disease and asthma in a Medicare advantage population. J Man Care Pharm 2008; 14:176–185.
- Soriano JB, Davis KJ, Coleman B, The proportional Venn diagram of obstructive lung disease: two approximations form the US and UK. Chest 2003; 124:474–481.
- Sidney S, Sorel M, Quesenberry CP, COPD and incident cardiovascular disease hospitalizations and mortality: Kaiser Permanente Medical Care Program. Chest 2005;128:2068–2075.
- Curkendall SM, DeLuise C, Jones JK, Cardiovascular disease in patients with chronic obstructive pulmonary disease, Saskatchewan Canada cardiovascular disease in COPD patients. Ann Epidemiol 2006; 16:63–70.
- Hardin M, Silverman EK, Barr G, The clinical features of the overlap between COPD and asthma. Respir Res 2011; 12:127–132.
- Centers for Disease Control and Prevention. Public Health Strategic Framework for COPD Prevention. Atlanta, GA: Centers for Disease Control and Prevention; 2011. Available at http://www.cdc.gov/copd/pdfs/Framework_for_COPD_Prevention.pdf
- Mannino DM. Institute of Medicine. A Nationwide Framework for Surveillance of Cardiovascular and Chronic Lung Diseases. Washington DC: The National Academies Press; 2011. Available at http://www.iom.edu/Reports/2011/A-Nationwide-Framework-for-Surveillance-of-Cardiovascular-and-Chronic-Lung-Diseases.aspx
- Herrick H, Pleasants R, Wheaton A, Liu Y Chronic obstructive pulmonary disease and associated health-care resource Use — North Carolina, 2007 and 2009. MMWR Morb Mortal Wkly Rep 2012; 61:143–146.
- Centers for Disease Control and Prevention –USA. Behavioral Risk Factor Surveillance System Operational and User's Guide (http://www.cdc.gov/brfss), Atlanta, GA, 1998.
- Centers for Disease Control and Prevention –USA. Behavioral Risk Factor Surveillance System 2007 Summary Data Quality Report (http://www.cdc.gov/brfss)
- Centers for Disease Control and Prevention –USA. Behavioral Risk Factor Surveillance System 2009 Summary Data Quality Report (http://www.cdc.gov/brfss)
- US Census Bureau, 2010 census, North Carolina. Accessed online March 12, 2012 at http://www.2010census.nc.gov
- Akinbami L, Moorman JE, Liu X. Asthma prevalence, healthcare use, and mortality: United States; 2005–2009. Hyattsville, MD, National Health Statistics Report No. 32, National Center for Health Statistics, 2011.
- Kosacz N, Punturieri A, Croxton T, Chronic obstructive pulmonary disease among adults –United States, 2011. MMWR Morb Mortal Wkly Rep 2012; 61:938–943.
- Zharan HS, Bailey C, Garbe P. Vital signs: asthma prevalence, disease characteristics, and self-management education—United States, 2001–2009. MMWR Morb Mortal Wkly Rep May 6, 2011 60:547–552.
- Haahtela T, Tuomisto LE, Pientinalho A, A 10 year asthma programme in Finland: major change for the better. Thorax 2006; 61:663–670.
- Ford ES, Mannino D. Time trends in obesity among adults with asthma in the US; findings from three national surveys. J Asthma 2005; 42(2):91–95.
- Poulain M, Doucet M, Major G, The effect of obesity on chronic respiratory diseases: pathophysiology and therapeutic strategies. Can Med J 2006; 174(9):1293–1299.
- Methvin J, Mannino D, Casey B. COPD prevalence in Southeastern Kentucky: the burden of lung disease study. Chest 2008; 135:102–107.
- Divo M, Cote C, de Torres J, Co-morbidities and mortality in patients with chronic obstructive pulmonary disease. Am J Resp Crit Care Med 2012; 186;155–161.
- Mannino D, Thorn D, Swensen A, Holguin F. Prevalence and outcomes of diabetes, hypertension, and cardiovascular disease in COPD. Eur Resp J 2008; 32:962–969.
- Miravitlles M, Soriano J Anchochea J, Characterisation of the overlap COPD–asthma phenotype. Focus on physical activity and health status. Resp Med 2013; 107:1053–1060.
- Putcha N, Puhan M, Hansel N, Drummond M, Boyd C. Impact of co-morbidities on self-rated health in self-reported COPD: An analysis of NHANES 2001–2008. COPD 2013: 10:324–332.
- State Center for Health Statistics. North Carolina Department of Health and Human Services. BRFSS 2009. http://epi.state.nc.us/SCHS/BRFSS/nc/all. Accessed April 22, 2012.
- Eisner MD, Blanc PD, Omachi A, Socioeconomic status, race, and COPD health outcomes. J Epidemiol Commun Health 2011; 65:26–34.
- Miravitlles M, Naberan K, Cantoni J, Azpeitia A. Socioeconomic status and health-related quality of life of patients with chronic obstructive pulmonary disease. Respiration 2011; 82:402–408.
- Kanervisto M, Vasankari T, Laitnen T, Low socioeconomic status is associated with chronic obstructive airways diseases. Resp Med 2011; 105:1140–1146.
- Nguyen K, Zahran H, ../../../Documents and Settings/ikd8/Local Settings/Temporary Internet Files/Content.Outlook/AppData/Local/Microsoft/Windows/pubmed%3fterm = %22Iqbal S%22%5bAuthor%5d et al. Factors associated with asthma control among adults in five New England states, 2006–2007. J Asthma 2011; 48:581–588.
- Silva GE, Sherrill DL, Guerra S, Barbee RA. Asthma as a risk factor for COPD in a longitudinal study. Chest 2004; 126:59–65.
- Kauppi P, Kupiainen KH, Lindqvist A, Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma 2011; 48:279–285.
- Shaya FT, Dongyi D, Akawaza MO, Burden of concomitant asthma and COPD in a Medicaid population. Chest 2008; 134:14–19.
- Pleasants R, Herrick H, Liao W, Ohar J. Use of a US population-based survey to describe the relationship of COPD and co-morbidities. Eur Resp J 2011; 38(Supp 55):182s.
