Abstract
Background: Chronic obstructive pulmonary disease (COPD) is among the leading causes of death globally, accounting for about 3 million deaths worldwide in 2011. We aimed to estimate the prevalence of COPD in Africa in the year 2010 to provide the information that could assist health policy in the region. Methods: We conducted a systematic review of Medline, EMBASE and Global Health for studies on COPD published between 1990 and 2012. We included original population based studies providing estimates of the prevalence of COPD. We considered the reported estimates in terms of the mean age of the sample, sex ratio, the year of study and the country of the study as possible covariates. Results from two different types of studies, i.e., based on spirometric and non-spirometric diagnosis of COPD, were further compared. The United Nation Population Division's population figures were used to estimate the number of COPD cases in the year 2010. Results: Our search returned 243 studies, from which only 13 met our selection criteria and only five were based on spirometry. The difference in the median prevalence of COPD in persons aged 40 years or older based on spirometry data (13.4%; IQR: 9.4%–22.1%) and non-spirometry data (4.0%; IQR: 2.1%–8.9%) was statistically significant (p = 0.001). There was no significant effect of the gender or the year of the study on the reported prevalence of COPD in either set of studies. The prevalence of COPD increased with age in spirometry-based studies (p = 0.017), which is a plausible finding suggesting internal consistency of spirometry-based estimates, while this trend was not observed in studies using other case definitions. When applied to the appropriate age group (40 years or more), which accounted for 196.4 million people in Africa in 2010, the estimated prevalence translates into 26.3 million (18.5–43.4 million) cases of COPD. Comparable figures for the year 2000 based on the same prevalence rates would amount to 20.0 million (14.1–33.1), suggesting an increase of 31.5% over a decade that is attributable to ageing of the African population alone. Conclusion: Our findings suggest that COPD is likely to already represent a very large public health problem in Africa. Moreover, rapidly ageing African population should expect a steady increase in the number of COPD cases in the next decade and beyond. The quantity and quality of available evidence does not match the size of the problem. There is a need for more research on COPD prevalence, but also incidence, mortality and risk factors in Africa. We hope this study will raise awareness of COPD in Africa and encourage further research.
Introduction
The burden of non-communicable diseases (NCDs) is rapidly increasing worldwide. A general consensus at the 2011 United Nations high level meeting on NCDs affirmed that they jointly became the leading causes of deaths globally, and are expected to account for about 52 million deaths by 2030 (Citation1, 2). The focus of the World Health Organization (WHO) and many stakeholders has turned towards addressing this burden more actively, especially in Africa and other low- and middle-income countries (LMIC), where a large public health burden is still being caused by infectious diseases (Citation2). Africa is currently experiencing the fastest rate of urban development worldwide (Citation2, Citation4). With increasing standard of living and improved care seeking, life expectancy across many African nations will continue to rise (Citation4). The growing burden of NCDs in Africa is partly due to demographic changes and ageing of the population, and partly to rapid urbanization and adoption of urban lifestyles (Citation2, Citation5). In combination, these two main drivers of the pandemics of NCDs are likely to increase both the prevalence and the absolute number of cases for many NCDs across Africa in the near future (Citation2).
Chronic respiratory diseases (CRDs) rank among the leading causes of morbidity and mortality among NCDs worldwide, accounting for 4.7% of global disability-adjusted life years (DALYs), of which chronic obstructive pulmonary disease (COPD) is responsible for about two-thirds (Citation5). According to 2008 global burden of disease (GBD) estimates, over 600 million have allergic rhinitis, 300 million people have asthma, and 210 million people have COPD (Citation1, Citation6, Citation7). The WHO also estimates that COPD is responsible for about 3 million deaths globally in 2011, accounting for about 9.1% of all NCDs deaths (Citation8). COPD is currently the fourth leading cause of death globally and is projected to be the third leading cause of death by 2030 (Citation8), by which point it is expected to overtake HIV/AIDS as the leading cause of death in Africa (Citation9).
The increasing burden of COPD in Africa can be attributed to factors such as tobacco smoking, environmental pollution, exposure to combustion products of biomass fuels (from coal, firewood and agricultural residue), occupational dusts, tuberculosis, and long-term sequelae of childhood respiratory infections (Citation10). Attempts at reducing this burden have been hindered mainly due to: inadequate standards of health promotion and other health services; insufficient attention from health planners, government regulators and media; absence of national guidelines on the management of COPD and lack of funds (Citation11, 12). In fact, in many urban African settings, reports reveal an increasing consumption of tobacco products (Citation10), which is made worse due to lack of government regulations on tobacco sales and use (Citation10, 11). In some mixed, urban and rural settings, most households still use firewood and charcoal for domestic cooking and many countries are yet to implement control strategies for biomass fuel exposure (Citation10, Citation12).
The treatment of COPD in many resource-poor settings has also been a huge challenge (Citation13). Inhaled steroids, which are an effective treatment of COPD, have been included in the amended WHO list of essential medicines (Citation10). However, these are mostly unavailable and/or unaffordable in many African settings (Citation9, Citation14). In fact, policymakers in some African countries have stated that it may be unrealistic to assume that essential drugs for treating COPD and other CRDs can be given free to patients (Citation11, Citation14). This raises critical questions of equity and priority setting, since drugs for HIV/AIDS and tuberculosis are typically supplied free in Africa (Citation9, Citation11).
Moreover, there is a lack of standard treatment guidelines and protocols for the management of COPD, and when available, health workers have not been adequately trained to identify and treat the disease (Citation15). Lung function assessment is vital to COPD diagnosis and in quantifying airflow obstruction, and this is often needed to differentiate COPD from other obstructive airway diseases (Citation11). It has been reported that spirometer, peak flow meter, and simple lung function test apparatus are scarcely available in many African settings and most treatments have mainly been based on acute exacerbations rather than an overall disease management plan (Citation11, Citation16). Therefore, delayed diagnosis of COPD typically follows lengthy periods of hesitation from doctors and concerns raised by patients and their families (Citation10, Citation17).
The understanding of the epidemiology of COPD on the African continent is still very limited (Citation11). Although systematic reviews have been conducted on COPD in Africa (Citation10–12), only one of them is about the continent-wide burden of COPD, while two other two focused on sub-Saharan Africa. These reviews mainly provided a systematic presentation of the available evidence, but there is still a need to further analyse the available studies to understand the appropriateness of the case definition used (spirometry vs non-spirometry data) and the effects of covariates such as sex, age, year of the study and country of the study. Researchers, policy makers and other stakeholders in Africa could be assisted with such information in designing further studies. Therefore, in this paper we aim to provide a deeper insight in the problem of COPD in Africa, by examining and comparing the two available types of data (spirometry-based and other) and investigating the role of covariates on the prevalence of COPD in Africa.
Methods
Search strategy and data sources
After identifying the relevant Medical Subject Headings (MeSH) and keywords, a systematic search of Medline, EMBASE and Global Health was conducted. The publication period studied was from January 1990 up to September 2013. Further relevant studies were identified through searching the references of all selected studies. African countries were included based on the World Bank list of economies (July 2012) (Citation22). The search terms employed are shown in Table . No language restrictions were applied.
Table 1. Search terms
Characteristic features of the identified African studies
Primary research on COPD in Africa has been very limited. This has in part been linked to challenges in the accurate diagnosis of this condition and the heterogeneity of published research protocols (Citation18). Various published reports have noted that symptoms of COPD, asthma and other obstructive airway diseases do overlap, which often complicates the case ascertainment in research studies (Citation3). COPD has been previously described in terms of its clinical and pathological presentation, mainly as “chronic bronchitis” and “emphysema” (Citation19). These, however, have not adequately explained the basic physiological impairment of the lungs in a COPD patient that, according to pulmonologists, can be traced to a reduced expiratory volume compared to the vital capacity of the lungs (Citation10, Citation19). The Global Initiative on Obstructive Lung Disease (GOLD) and the ‘American Thoracic Society/ European Respiratory Society’ (ATS/ERS) have provided clear definitions of COPD based on spirometry (defined as a ratio of forced expiratory volume in one second to forced vital capacity less than 70% (FEV1/FVC <0.7) (Citation20, 21), see Table .
Table 2. GOLD and ATS/ERS COPD diagnostic criteria
Since the publication of GOLD and ATS/ERS criteria, research outputs from Africa have still remained low, with the few COPD studies from Africa being mainly non-spirometric studies (Citation11). Furthermore, existing reviews have identified only ten countries in Africa that have conducted and published research findings on COPD and these are mainly from selected populations and occupational settings where the case definitions were mostly based on respiratory symptoms (Citation10). These have all limited on-going research efforts towards determining the true burden of COPD in Africa.
Study selection
A parallel search and double extraction of data was conducted by the first two co-authors. We retained original population-based studies on COPD and/or chronic bronchitis conducted in urban, rural or occupational settings within African population groups. We also ensured that the retained studies provided numerical estimates on the prevalence of COPD and/or chronic bronchitis, and had clearly defined methodologies. We excluded studies that were hospital-based, had non-human subjects, have been conducted before 1990, or that were review publications.
Case definitions needed to comply with:
the Global Initiative on Obstructive Lung Disease (GOLD) criteria (Citation20);
the American Thoracic Society/ European Respiratory Society (ATS/ERS) criteria (Citation21), {with GOLD and ATS/ERS criteria both broadly defined as a post-bronchodilatory (PBD) ratio of forced expiratory volume in one second to forced vital capacity of less than 70% (PBD FEV1/FVC < 0.7)}; and/or
the 1965 British Medical Research Council (BMRC) definition of chronic bronchitis, defined as “chronic productive cough on most days for 3 months in 2 consecutive years in a person in whom other causes of chronic productive cough have been excluded” (Citation20, 21), see Table for detailed diagnostic criteria.
Data extraction and analysis
Data have been extracted from the retained studies and included information concerning the corresponding country, the study period, the mean age (and any age groups that were studied specifically), the number of cases, the sample size and the prevalence of COPD. Studies were broadly grouped into “spirometric” (defined as complying with case definitions ‘i and ii’, as mentioned above) and “non-spirometric” (defined as complying with case definitions ‘iii’). For studies conducted on the same study site, population or cohort, the first chronologically published study has been considered, with all additional new data from more recent studies further added.
For our analysis, the prevalence of COPD was separately investigated from “spirometric” and “non-spirometric” sets of studies and the effect of covariates (e.g., mean age, gender, year of study and the country). In addition, the prevalence of COPD from the two types of studies was compared. We used Pearson correlation coefficients, t-test on equality of means, and the Mann-Whitney test for equality of medians to study the effects of case definition and other covariates on the prevalence of COPD. We used the median and inter-quartile range from spirometry-based studies and the United Nation Population Division's population figures to estimate the number of COPD cases in the year 2010.
Results
Systematic review
Our search has returned 243 studies: Medline (Citation66), EMBASE (144), and Global Health (Citation33). After screening the titles for relevance and excluding duplicates, 134 publications were selected. Sixty-nine abstracts satisfied our inclusion criteria. After applying the quality criteria, i.e. studies with clear case definitions and sampling methods, 58 studies were excluded. Two additional studies have been included from the search of the reference lists of the selected studies. A total of 13 studies met the quality criteria and thus have been included in our study (Figure ).
Study characteristics
From the retained studies (Citation23–35), 7 were conducted in South Africa and Nigeria. Other countries represented were Algeria, Ethiopia, Malawi, Morocco, Rwanda and Tunisia. There were 5 spirometric (Citation23, Citation27–29, Citation31) and 10 non-spirometric studies (Citation24–26, Citation28, Citation30–35), with 13 and 20 data points, respectively; two studies reported both spirometric and non-spirometric estimates (Citation28, Citation31) (Tables and ). All studies focussed on subjects with a mean age of 55.2 years and 49.2 years in spirometric and non-spirometric studies, respectively. Across many studies, birth certificates were usually employed in determining the age of subjects, and in the absence of valid age-verification documents, historical landmarks were employed. Studies were conducted mostly within one year (7 studies), overall mean sample size was 1241 (median 416), and study settings were predominantly mixed (urban and rural) (6 studies).
Table 3. Overall study characteristics
Table 4. Distribution of studies
Prevalence estimates
First, we report separately the estimates of the prevalence of COPD for the two types of data: spirometry-based and all other studies (Table ; Figure ). The median prevalence of COPD from spirometry-based studies is 13.4% (IQR: 9.4%–22.1%), while for all other studies it is 4.0% (IQR: 2.1%–8.9%). This difference is statistically significant (p = 0.001 for comparison of medians and p = 0.003 for comparison of means). The descriptive statistics for other covariates, such as the year of study, mean age, the number of cases and sample size are shown in Table .
Figure 2. Boxplots of the prevalence of COPD for the studies based on spirometry and all other studies.
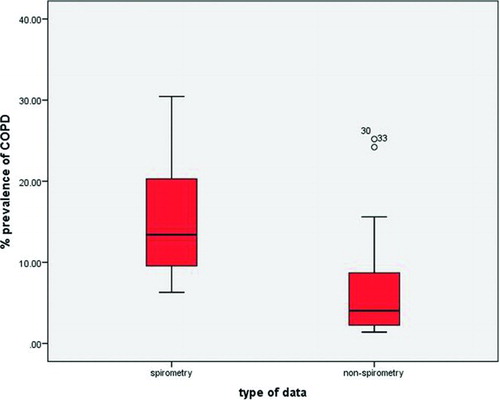
Table 5. Statistics for year, mean age, number of cases, sample size and prevalence of COPD for the spirometry-based studies and all other studies
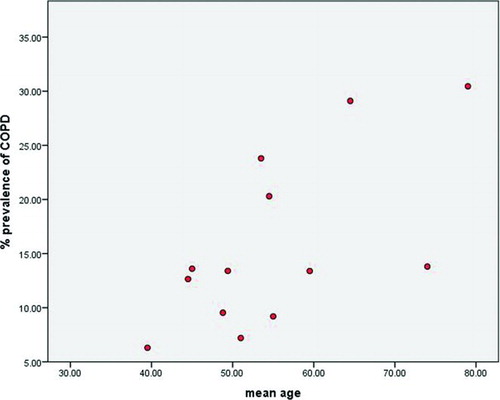
A significant positive correlation has been demonstrated between the prevalence of COPD and the mean age in the spirometry-based set of studies (see Figure ), with the Pearson correlation coefficient of 0.645 (p-value = 0.017). This is a plausible finding that suggests internal consistency of spirometry-based estimates, while this trend was not observed in studies using other case definitions. Moreover, no significant correlation could be demonstrated between the prevalence of COPD and the year of study or gender for both data sets (see Supplementary Online Material).
When applied to the appropriate age group (40 years or more), which accounted for 196.4 million people in Africa in 2010, the estimated prevalence translates into 26.3 million (18.5–43.4 million) cases of COPD. Comparable figures for the year 2000 based on the same prevalence rates would amount to 20.0 million (14.1–33.1), suggesting an increase of 31.5% over a decade that is attributable to ageing of the African population alone.
Discussion
Although we recognize that there may be on-going efforts to estimate the prevalence of COPD in Africa by other research groups, among which the BOLD initiative is particularly prominent (Citation36), this study—to the best of our knowledge—provides the first systematic continent-wide estimates of COPD prevalence in Africa. Our results show a significant association between patient's age and COPD prevalence in a spirometry-based data set (Citation4, Citation37–39), and further point out the statistically significant differences between spirometry and non-spirometry data, among which spirometry-based estimates generally appear more homogenous and internally consistent.
The 2006 BOLD study (conducted across 12 sites globally) reported a global COPD prevalence of 10.1% (male 11.8%; female 8.5%) using GOLD criteria (Citation23). They did not quote overall estimates for Africa, as South Africa was the only African study site (Citation23). However, that study reported a COPD prevalence of 22.2% and 16.7% in South Africa among men and women aged ≥40 years, respectively, which seems very high and it's unlikely to be representative for the rest of Africa (Citation23). In other studies, conducted among community-based population samples, a spirometric prevalence of 13.6% was estimated in Malawi and 9.2% in Algeria (Citation27, Citation29). Other studies conducted in Africa were mainly non-spirometric with low recorded prevalences (Nigeria 5.6%, South Africa 2.6% and Algeria 1.7%) (Citation24, Citation26, Citation29). These are the major population-based studies on COPD conducted in Africa, with no systematic continent-wide prevalence estimates published.
Our mean and median prevalences from all study populations were higher for the spirometric studies compared to non-spirometric studies (Table ), which supports previous reports on the under-estimation of COPD from non-spirometric studies (Citation23).
Based on the retained studies, we note that the prevalence of smoking was high in some study populations, with odds of having COPD among current smokers estimated at 6.37 (Nigeria), 3.22 (Rwanda), and 1.15 and 2.84 (South Africa) (Citation23, 24, Citation30, Citation33) (Table ). It is important to note that this study is not a comprehensive review of smoking prevalence in Africa, as there were only four studies reporting COPD risks among current smokers (Citation23, 24, Citation30, Citation33); it may therefore be inappropriate to draw conclusions based on this. However, some authors warned that Africa is on the verge of a smoking epidemic due to a rapidly spreading tobacco market in the continent, and could be contributing to the growing burden of chronic respiratory diseases in the region (Citation43).
Table 6. Prevalence of COPD in terms of smoking from selected studies
For example, Jha and colleagues reported an increasing prevalence of smoking in Africa with an overall prevalence of 18% in 1995 (Citation44). In addition, a systematic review of studies conducted among persons aged 15 years or more, across 14 countries in sub-Saharan Africa (SSA), reported smoking prevalence ranging from 6% to 24% between 1996 and 2005, with a high proportion of young smokers (Citation45). The increasing prevalence was further underpinned in a 2006 demographic health survey, also conducted across 14 countries in SSA, with reported smoking prevalence ranging from 8% to 27% (Citation46). Moreover, some other research findings have shown that COPD prevalence in many parts of the world increases along with the increasing number of cigarette packs per year, with findings in some African population groups suggesting they could be more prone to the health risks from tobacco smoke than people living in other world regions (Citation10, Citation23, Citation47).
Meanwhile, according to the 2010 Institute for Health Metrics and Evaluation (IHME) global burden of disease studies, the DALYs and deaths for COPD decreased between 1990 and 2010 by 2.0% and 6.4% respectively (DALYs decreased from 78.3 to 76.7 million, and deaths from 3.1 to 2.9 million) (Citation5, Citation48). These are global estimates based on complex modelling, and we appreciate that these may not necessarily reflect the COPD prevalence in Africa for many different reasons, including (but not limited to) contextual, socio-economic, demographic and ethnic differences in many regions of the world. Furthermore, many concerns have been raised about the choice of data and modelling methods used in the GBD 2010, so we should treat their estimates with caution until they are independently confirmed (Citation49, 50).
Although we aimed to provide an evidence-based and data driven prevalence estimate of COPD in Africa, the current low research output and the major gaps in data availability from many countries have greatly limited our analysis. We thus understand there could be uncertainties surrounding the estimates of the prevalence of COPD, such as variations in population structures, diagnoses, sampling methods, and effects of other health determinants (beyond the age of patients). First, the number of retained studies was very low, with only 8 African countries represented, and over 50% of data-points originating from South Africa and Nigeria. Our results may therefore tend to reflect more the COPD burden in these two countries and limit their generalizability to other African countries, given that those are relatively wealthy countries in African terms. Second, the overall sample size was relatively small (at 24,747), with a mean and median sample size per study of 1,767 and 416, respectively. Third, there were significant variations in diagnostic criteria and survey methodologies across studies. Most retained studies were population-based cross-sectional studies. However, due to the very limited evidence base and due to the published reports that occupational COPD contributes significantly to the global burden of chronic respiratory diseases (Citation51), we also included studies conducted in occupational settings. As this is strictly within a population where subjects have been exposed over time to COPD risks, we understand this may potentially increase our prevalence estimates. Finally, we mention that across all studies, data on age- and sex-specific prevalence, including corresponding data on urban-rural settings were not always provided, although they are of vital importance to perform further comparisons and reach conclusions about the prevalence of COPD in specific age groups or settings.
Public health response to COPD in Africa
A major setback in the fight against the growing burden of COPD in Africa is the relative neglect by the governments of many African nations. COPD is thought to be a rather complex disease, usually self-inflicted, irreversible, and difficult to treat (Citation52, 53). Many African governments have not set up awareness campaigns and preventive programmes that can help address these issues (Citation9). There is also the problem of unchecked urbanization, with no policies and or legislation to protect citizens from adverse effects, such as increase tobacco sales and use, and air pollution from industrial effluents, smoke and smog (Citation10). For example, a study showed that less than 10% of the global population, especially in Africa, is fully protected by any form of tobacco-demand reduction measures (Citation52). Addressing this is even more difficult because tobacco companies, which can be important drivers of some African economies, are using several tactics to resist regulation against its products, including: stressing the importance of tobacco to the economy of the countries that grow it, funding political parties, lobbying and influencing policies on tobacco products, preventing anti-smoking adverts and campaigns and buying off researchers and experts to create controversies on established facts on smoking (Citation54, 55).
Furthermore, research findings have also shown that the risk of developing COPD from exposure to biomass fuels is comparable to the risk from tobacco smoking (Citation6, Citation56). This is particularly significant in Africa, as about 90% of rural settings still rely on unprocessed biomass fuel for domestic cooking and heating, a situation made worse due to inadequate health awareness and intervention programmes reaching these settings (Citation25). In fact, evidence is now emerging that due to erratic power supply and high costs of cooking gas in many African nations, the use of charcoal and firewood is gradually increasing among many urban dwellers, as this is now considered a cheap alternative for domestic cooking (Citation3, Citation10). It is believed that an improved biomass stove and cooking environment remain the most cost-effective intervention for reducing the prevalence of COPD in sub-Saharan Africa (Citation10).
Experts have reported that health sector reform programmes targeted at COPD and other chronic diseases in many African countries have not been very effective (Citation16, 17). The Global Alliance against chronic Respiratory Diseases (GARD), an initiative of the WHO, recommends that a framework for chronic respiratory diseases surveillance should involve monitoring the exposures, outcomes and health system capacity response, and technically supporting appropriate interventions where and when necessary (Citation57). According to WHO African Regional Office, GARD functions in Africa, but insufficient government support at a country level often leads to non-implementation of programmes (Citation10). In addition, while appreciable health reforms and intervention programmes have been conducted in parts of Africa, adherence to these programmes at a community and individual level is low (Citation3). For example, biomass stove intervention programmes in some areas have not been effective; reports show there are a wide range of national, regional, community and individual reasons why people may not adhere to the intervention programmes (Citation9, Citation13). This further underscores the importance of understanding cultural backgrounds and social systems in an African setting towards improving acceptability of many interventions (Citation10).
The delayed health care seeking behaviour in many African populations has also affected the management of COPD (Citation10). For example, in a study of 298 patients attending respiratory clinics in rural South Africa, the observed median total delay to health facility was about 10 weeks, despite many being at severe stages of disease (Citation58). This has been linked to high cost of health care, illiteracy and inherent cultural beliefs, with all these resulting in increased patronage of traditional (herbal) healers (Citation9). Patients often present back at health centres with complications from improper management given by the traditional healers (Citation59).
In health service delivery, studies have reported that many health workers are ill-equipped in diagnosing COPD, making the under-diagnosis of COPD a problem confronting many African nations (Citation40). Moreover, it is believed that the under-recognition of COPD in African countries may be because patients present late and, even after presentation to health services, diagnoses are typically delayed until the disease is relatively advanced (Citation40, 41). Research findings have shown that lack of (use of) spirometers poses a very important practical challenge in rural settings with the main reasons being due to unavailability, improper usage, and low awareness of their importance (Citation11). The unavailability and unaffordability of drugs have also affected health service delivery (Citation10). Many countries provide free tuberculosis and HIV treatments, while essential drugs for COPD and other CRDs, such as inhaled beclomethasone, are either unavailable or unaffordable (Citation6, Citation60). This unavailability of drugs may reflect lack of funds but may also be partly due to available limited funds being used inappropriately for expensive drugs that have no proven value in the management of COPD (Citation10).
The relatively low income status in Africa is also contributory to the overall burden of COPD in Africa, especially at the family and individual levels. According to clinicians, poor living conditions, such as overcrowded homes, poor domestic cooking environment, and poorly ventilated houses, may worsen COPD; and due to the low income status, patients may still lack the financial resources to seek proper treatment (Citation61, 62). Personal healthcare expenses in Africa are mostly out-of-pocket; there are no standard health insurance schemes as found in high-income settings (Citation13).
The low level of published research on COPD and other CRDs has posed a major challenge to policymakers and many stakeholders, as there are not yet enough evidenced-based findings that can contribute to informed policy making to tackle this disease burden (Citation59). The limited amount of published research in Africa may be due to challenges in conducting studies that would fully adhere to internationally agreed case definitions (Citation40). For example, many studies now use post-bronchodilatory spirometry as a gold standard (Citation42); whereas others state that using post-brochodilator estimates may result in a 5–50% reduction in prevalence compared to pre-bronchodilator values (Citation39). It has been suggested that the low research output reflects the poor recent availability of research funding for COPD by funding agencies, which in turn reflects their lack of priority given to COPD (Citation11, Citation16). The research priorities of many African governments still focus on communicable diseases, notably HIV/AIDS, tuberculosis and malaria (Citation63, 64). In addition, the influence of the tobacco industry, which financially supports many governments in Africa, may also have negatively affected research output in the field (Citation10, Citation65, Citation66).
Conclusion
The data on COPD in Africa is limited, with the few published studies only available from some countries in Africa. However, it is evident from those studies that the burden of COPD in Africa is significant. With continued urbanization, rapid ageing and lack of corresponding measures to check the effects on the population, the burden of COPD will continue to grow and it is set to become one of the major public health problems in Africa.
There is need for more research on COPD prevalence, incidence, sequelae and mortality, along with well-designed trials, to identify how to effectively reduce risks from exposure to biomass fuels and tobacco smoking. With improved awareness of this problem, policy makers and governments of many African nations should give more attention to NCDs such as COPD, fund relevant research to improve evidence for decision making, and thus make informed decisions on preventive and treatment strategy options, and so help counter the rising disease burden over the next decade.
Declaration of Interests Statement
All co-authors designed and conducted the study and contributed to the writing of the paper.
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author). The authors declare no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities that could appear to have influenced the submitted work; apart from that declared under “funding.”
Supplementary Online Material
Download MS Word (133.7 KB)Supplementary materials are available in the online version of this article.
References
- WHO. The global burden of disease: 2004 update. Geneva: WHO, 2008.
- Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P. The Lancet NCD Action Group and the NCD Alliance. Priority actions for the non-communicable disease crisis. Lancet. 2011; 377:1438–1447.
- Musafiri S, Joos G, Van Meerbeeck JP. Asthma, atopy and COPD in sub-Saharan countries: the challenges. East Afr J Publ Health. 2011; 8(2):161–163.
- Chan KY, Adeloye D, Grant L, Kolčić I, Marušić A. How big is the ‘next big thing’? Estimating the burden of non-communicable diseases in low- and middle-income countries. J Glob Health. 2012; 2(2):20101.
- Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380(9859):2197–2223.
- Ait-Khaled N, Enarson D, Bousquet J. Chronic respiratory diseases in developing countries: the burden and strategies for prevention and management. Bull World Health Org 2001; 79(10):971–979.
- Chermiti Ben Abdallah F, Taktak S, Chtourou A, Mahouachi R, Ben Kheder A. Burden of chronic respiratory diseases (CRD) in middle east and North Africa (MENA). World Allergy Organization J 2011; 4 (SUPPL. 1):S6–S8.
- WHO. Global status report on noncommunicable diseases 2010. Geneva: World Health Organization, 2011.
- Chan-Yeung M, Ait-Khaled N, White N, Ip MS, Tan WC. The burden and impact of COPD in Asia and Africa. Inter J Tuberculosis Lung Dis 2004; 8 (1):2–14.
- van Gemert F, van der Molen T, Jones R, Chavannes N. The impact of asthma and COPD in sub-Saharan Africa. Primary Care Respir J 2011 Sep; 20(3):240–248.
- Mehrotra A, Oluwole AM, Gordon SB. The burden of COPD in Africa: a literature review and prospective survey of the availability of spirometry for COPD diagnosis in Africa. Trop Med Inter Health 2009 Aug; 14(8):840–848.
- Finney LJ, Feary JR, Leonardi-Bee J, Gordon SB, Mortimer K. Chronic obstructive pulmonary disease in sub-Saharan Africa: a systematic review. Int J Tuberc Lung Dis 2013; 17(5):583–589.
- Stanciole AE, Ortegon M, Chisholm D, Lauer JA. Cost effectiveness of strategies to combat chronic obstructive pulmonary disease and asthma in sub-Saharan Africa and South East Asia: mathematical modelling study. BMJ 2012; 344:e608.
- El Hasnaoui A, Rashid N, Lahlou A, Salhi H, Doble A, Nejjari C. Chronic obstructive pulmonary disease in the adult population within the Middle East and North Africa region: Rationale and design of the BREATHE study. Respiratory Medicine. 2012; 106 (SUPPL. 2):S3–S15.
- IUATLD. The Global Asthma Report 2011. Paris, France: The International Union Against Tuberculosis and Lung Disease; 2011.
- Abdool-Gaffar MS, Ambaram A, Ainslie GM, Bolliger CT, Feldman C, Geffen L, et al. Guideline for the management of chronic obstructive pulmonary disease—2011 update. S Afr Med J. 2011; 101(1 Pt 2):63–73.
- Aisanov Z, Bai C, Bauerle O, Colodenco FD, Feldman C, Hashimoto S, et al. Primary care physician perceptions on the diagnosis and management of chronic obstructive pulmonary disease in diverse regions of the world. Inter J COPD 2012; 7:271–282.
- Gjevre JA, Hurst TS, Taylor-Gjevre RM, Cockcroft DW. The American Thoracic Society's spirometric criteria alone is inadequate in asthma diagnosis. Can Respir J 2006; 13(8):433–437.
- Viegi G, Pistelli F, Sherrill DL, Maio S, Baldacci S, Carrozzi L. Definition, epidemiology and natural history of COPD. Euro Respir J 2007; 30(5):993–1013.
- GOLD. Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease Revised. 2011 [23 April 2012]; Available from: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2011_Feb21.pdf.
- ERS-ATS. ERS-ATS COPD Guidelines. Switzerland: European Respiratory Society; 2005 [25 May 2012]; Available from: www.ersnet.org.
- World Bank. World Bank List of Economies (July 2012)2012: Available from: http://librarians.acm.org/sites/default/files/world%20bank%20List%20of%20Economies%20%28as%20of%20July%202012%29.pdf.
- Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, et al. International variation in the prevalence of COPD (The BOLD Study): a population-based prevalence study. Lancet 2007; 370(9589):741–750.
- Desalu OO. Prevalence of chronic bronchitis and tobacco smoking in some rural communities in Ekiti state, Nigeria. Niger Postgrad Med J 2011; 18(2):91–97.
- Desalu OO, Adekoya AO, Ampitan BA. Increased risk of respiratory symptoms and chronic bronchitis in women using biomass fuels in Nigeria. J Brasileiro De Pneumologia: Publicacao Oficial Da Sociedade Brasileira De Pneumologia E Tisilogia 2010; 36(4):441–446.
- Ehrlich RI, White N, Norman R, Laubscher R, Steyn K, Lombard C, et al. Predictors of chronic bronchitis in South African adults. Inter J Tuberculosis Lung Dis 2004; 8(3):369–376.
- Fullerton DG, Suseno A, Semple S, Kalambo F, Malamba R, White S, et al. Wood smoke exposure, poverty and impaired lung function in Malawian adults. Inter J Tubercul Lung Dis 2011 Mar; 15(3):391–398.
- Gathuru IM, Bunker CH, Ukoli FA, Egbagbe EE. Differences in rates of obstructive lung disease between Africans and African Americans. Ethnic Dis 2002; 12(4):S3-107–113.
- Khelafi R, Aissanou A, Tarsift S, Skander F. [Epidemiology of chronic obstructive pulmonary disease in Algiers]. Revue Maladies Respir 2011; 28(1):32–40.
- Musafiri S, van Meerbeeck J, Musango L, Brusselle G, Joos G, Seminega B, et al. Prevalence of atopy, asthma and COPD in an urban and a rural area of an African country. Respir Med 2011; 105(11):1596–1605.
- Girdler-Brown BV, White NW, Ehrlich RI, Churchyard GJ. The burden of silicosis, pulmonary tuberculosis and COPD among former Basotho goldminers. Amer J Indust Med 2008; 51(9):640–7.
- Laraqui Hossini CH, Laraqui Hossini O, Rahhali AE, Tripodi D, Caubet A, Belamallem I, et al. Respiratory symptoms and ventilatory disorders among a group of cement workers in Morocco. [French]. Revue Maladies Respir 2002; 19 (2 I):183–189.
- Ayo-Yusuf OA, Reddy PS, van den Borne BW. Association of snuff use with chronic bronchitis among South African women: implications for tobacco harm reduction. Tob Control 2008; 17(2):99–104.
- Mengesha YA, Bekele A. Relative chronic effects of different occupational dusts on respiratory indices and health of workers in three Ethiopian factories. Am J Ind Med 1998; 34(4):373–380.
- Tabka F, Mrizek N, Tabka Z, Choudat D, Conso F. [Respiratory diseases related to cereal dust exposure in Tunisia]. Archives des maladies professionnelles et de médecine du travail. 1999; 60:101–106.
- Burney P. The Burden of Obstructive Lung Disease (BOLD) study prepares for African Surveys. Africa Health 2011; 33(2): 12.
- Mufunda J, Chatora R, Ndambakuwa Y, Nyarango P, Kosia A, Chifamba J, et al. Emerging Non-communicable Disease Epidemic in Africa: Preventive Measures from the WHO Regional Office for Africa. Georgia: International Society on Hypertension in Blacks.
- Silva-Matos C, Beran D. Non-communicable diseases in Mozambique: Risk factors, burden, response and outcomes to date. Globalization and Health. 2012; 8(37).
- Lopez Varela MV, Montes de Oca M, Halbert RJ, Muino A, Perez-Padilla R, Talamo C, et al. Sex-related differences in COPD in five Latin American cities: the PLATINO study. Eur Respir J. 2010 Nov; 36(5):1034–41.
- Martins P, Rosado-Pinto J, do Ceu Teixeira M, Neuparth N, Silva O, Tavares H, et al. Under-report and underdiagnosis of chronic respiratory diseases in an African country. Allergy 2009; 64(7):1061–1067.
- Menezes A, Macedo SC, Gigante DP, da Costa JD, Olinto MT, Fiss E, et al. Prevalence and risk factors for chronic obstructive pulmonary disease according to symptoms and spirometry. COPD 2004; 1(2):173–179.
- Talamo C, de Oca MM, Halbert R, Perez-Padilla R, Jardim JR, Muino A, et al. Diagnostic labeling of COPD in five Latin American cities. Chest 2007; 131(1):60–67.
- Jagoe K, Edwards R, Mugusi F, Whiting D, Unwin N. Tobacco smoking in Tanzania, East Africa: population based smoking prevalence using expired alveolar carbon monoxide as a validation tool. Tob Control 2002; 11(3): 210–214.
- Jha P, Ranson MK, Nguyen SN, Yach D. Estimates of Global and Regional Smoking prevalence in 1995, by Age and Sex. Am J Public Health 2002; 92(6):1002–1006.
- Townsend L, Flisher AJ, Gilreath T, King G. A systematic literature review of tobacco use among adults 15 years and older in sub-Saharan Africa. Drug Alcohol Depend 2006; 84(1):14–27.
- Pampel F. Tobacco use in sub-Saharan Africa: estimates from the demographic health surveys. Soc Sci Med 2008; 66(8):1772–1783.
- Chatila WM, Wynkoop WA, Vance G, Criner GJ. Smoking patterns in African Americans and whites with advanced COPD. Chest 2004; 125(1):15–21.
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380 (9859):2095–2128.
- Fan V, Lam F. Malaria Estimate Sausages by WHO and IHME. Washington, DC, USA: Centre for Global Development; 2012 [cited 2013 22 June]; Available from: http://www.cgdev.org/blog/malaria-estimate-sausages-who-and-ihme.
- Whiteford HA, Ferrari AJ, Baxter AJ, Charlson FJ, Degenhardt L. How did we arrive at burden of disease estimates for mental and illicit drug use disorders in the Global Burden of Disease Study 2010? Curr Opin Psych 2013; 26(4):376–383.
- Boschetto P, Quintavalle S, Miotto D, Lo Cascio N, Zeni E, Mapp CE. Chronic obstructive pulmonary disease (COPD) and occupational exposures. J Occup Med Toxicol 2006; 1:11.
- Barnes PJ. Chronic Obstructive Pulmonary Disease: A Growing but Neglected Global Epidemic. PLoS Med 2007; 4(5):e112.
- Bousquet J, Mantzouranis E, Cruz AA, Ait-Khaled N, Baena-Cagnani CE, Bleecker ER, et al. Uniform definition of asthma severity, control, and exacerbations: document presented for the World Health Organization Consultation on Severe Asthma. J Allergy Clin Immunol. 2010; 126(5):926–938.
- Otañez MG, Mamudu HM, Glantz SA. Tobacco companies’ use of developing countries’ economic reliance on tobacco to lobby against global tobacco control: the case of Malawi. Am J Public Health 2009; 99(10):1759–1771.
- Saloojee Y, Dagli E. Tobacco industry tactics for resisting public policy on health. Bull World Health Organ 2000; 78(7):902–910.
- Kiraz K, Kart L, Demir R, Oymak S, Gulmez I, Unalacak M, et al. Chronic pulmonary disease in rural women exposed to biomass fumes. Clinical & Investigative Medicine –Medecine Clinique et Experimentale. [Comparative Study]. 2003; 26(5):243–248.
- WHO. Global surveillance, prevention and control of Chronic Respiratory Diseases: A comprehensive approach. Geneva: WHO; 2007. Available from: http://www.who.int/gard/publications/GARD_Manual/en/index.html.
- Pronyk RM, Makhubele MB, Hargreaves JR, Tollman SM, Hausler HP. Assessing health seeking behaviour among tuberculosis patients in rural South Africa. Int J Tuberc Lung Dis 2001; 5(7):619–627.
- Laraqui CH, Caubet A, Laraqui O, Benghalem A, Harourate K, Bichara M, et al. [Prevalence of respiratory systems and evaluation of sensitization levels in traditional grain market workers in Casablanca]. Rev Mal Respir 2000; 17(5):947–955.
- Ait-Khaled N, Enarson DA, Ottmani S, El Sony A, Eltigani M, Sepulveda R. Chronic airflow limitation in developing countries: burden and priorities. Int J Chron Obstruct Pulmon Dis 2007; 2(2):141–150.
- Poyser MA, Nelson H, Ehrlich RI, Bateman ED, Parnell S, Puterman A, et al. Socioeconomic deprivation and asthma prevalence and severity in young adolescents. Euro Respir J [Research Support, Non-U.S. Gov't]. 2002; 19(5):892–898.
- Lamprecht B, McBurnie MA, Vollmer WM, Gudmundsson G, Welte T, Nizankowska-Mogilnicka E, et al. COPD in never smokers: Results from the population-based burden of obstructive lung disease study. Chest 2011; 139 (4):752–763.
- de-Graft Aikins A, Boynton P, Atanga LL. Developing effective chronic disease interventions in Africa: Insights from Ghana and Cameroon. Global Health 2010; 6(6).
- Erhabor GE, Kolawole OA. Chronic obstructive pulmonary disease: a ten-year review of clinical features in O.A.U.T.H.C., Ile-Ife. Niger J Med 2002; 11(3):101–104.
- Sitas F, Urban M, Bradshaw D, Kielkowski D, Bah S, Peto R. Tobacco attributable deaths in South Africa. Tobacco Cont 2004; 13(4):396–399.
- Adejuwon GA. Tobacco use and second hand smoke as risk factors for diseases in Nigeria: implications for collaborative research and multilevel tobacco control strategies. Afr J Med Med Sci 2009; 38 Suppl 2:21–29.