Abstract
Rationale: There is a paucity of population-based data on COPD prevalence and its determinants in Bangladesh.
Objective: To measure COPD prevalence and socioeconomic and lifestyle determinants among ≥40 years Bangladeshi adults.
Methods: In a cross-sectional study, we measured lung function of 3744 randomly selected adults ≥40 years from rural and urban areas in Bangladesh, using a handheld spirometer. COPD was defined according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria as post-bronchodilator ratio of Forced Expiratory Volume in 1st second (FEV1) to Forced Vital Capacity (FVC) < 0.7. In addition, COPD was also assessed by the lower limit of normal (LLN) threshold defined as lower fifth percentile for the predicted FEV1/FVC.
Results: The prevalence of COPD was 13.5% by GOLD criteria and 10.3% by LLN criteria. Prevalence of COPD was higher among rural than urban residents and in males than females. More than half of the COPD cases were stage II COPD by both criteria. Milder cases (Stages I and II) were over estimated by the GOLD fixed criteria, but more severe cases (Stages III and IV) were similarly classified. In multiple logistic regression analysis, older age, male sex, illiteracy, underweight, history of smoking (both current and former), history of asthma and solid fuel use were significant predictors of COPD.
Conclusion: COPD is a highly prevalent and grossly underdiagnosed public health problem in Bangladeshi adults aged 40 years or older. Illiteracy, smoking and biomass fuel burning are modifiable determinants of COPD.
Introduction
Chronic obstructive pulmonary disease (COPD) is a largely preventable and treatable condition characterized by irreversible and gradually progressive airflow limitation (1). According to WHO estimates 64 million people have moderate to severe COPD and more than 3 million or 5% of deaths globally in 2005 were attributable to COPD (2). Almost 90% of COPD deaths occur in low- and middle-income countries (3). COPD deaths have been increasing and it is projected that it will be the third-leading cause of death by 2030 (4).
Global prevalence of COPD was estimated to be 10.1% among individuals aged over 40 with a noticeable increase with age (5), although considerable variations, ranging from 6.5% to 17.9%, have been reported from South-East Asia (6), China (Citation7) and India (8). Population-based COPD data are rarely available in low-income countries as epidemiological data are often difficult to collect and is prohibitively expensive in those settings. The only hospital based study in Bangladesh reported the prevalence of COPD as 11.4% among urban population aged 35 years or older (9).
The major risk factor for COPD is tobacco smoking (10), which is highly prevalent in Bangladesh. A recent national survey reported about 23% of Bangladeshi adults aged ≥15 years smoke, but there is a large gender difference that 44.7% of males and only 1.5% of females self-reported as current smokers (11, 12). Exposure to passive smoking at home or work and indoor air pollution due to biomass fuel burning have also been reported to be significant risk factors for COPD (13, 14). Over 80% of households in Bangladesh use biomass fuel for heating and cooking (15). Sociodemographic factors such as rural residence and low level of education have also been reported to increase the risk for COPD (6, 13).
In this article we report the prevalence of COPD using objective measures of lung function parameters at the population level, following the lower limit of normal (LLN) (Citation16, Citation17) as well as the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria (18). To our knowledge this is the first population-based epidemiologic assessment of COPD and its socioeconomic and lifestyle determinants in Bangladesh and we believe it will pave the way for future research and preventive strategies including risk reduction for COPD.
Methods
Between February 2011 and March 2012 we conducted a cross-sectional study in rural Matlab (Chandpur district) and semi-urban Kamlapur (Dhaka district) to measure the prevalence of COPD. The International Center for Diaarhoel Disease Research, Bangladesh (icddr,b) has maintained demographic surveillance since 1966 in Matlab (Citation19,Citation20) and since 1995 in Dhaka (21). Our study population consisted of males and females who were 40 years or older males and females. The participants were selected from an icddr,b surveillance database at random from a total population of approximately 400,000 in both sites. Adequate numbers of age- and sex-specific participants were enrolled to fulfil the required sample size. Written informed consent was obtained from each of the respondents before enrolment. This study was approved by the Research Review Committee and the Ethical Review Committee of the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b).
Interviews were conducted by trained field workers at participants’ homes using a structured questionnaire designed for this study. Demographic and socioeconomic data was collected that included age, sex, education, occupation (manual or non-manual work) and income. Lifestyle variables included detailed smoking history (current/former, type of tobacco use, intensity and duration), environmental exposure to tobacco smoke at home or workplace, and household fuel type use. Participants’ weight and height was measured and BMI calculated.
Lung function was measured by spirometry using a hand-held portable, diagnostic Spirometer (ndd EasyOneTM Medizintechnik, Zurich, Switzerland), which is uninfluenced by gas composition, pressure, temperature, and humidity and can provide accurate measurements under varying environmental conditions. Field research assistants(FRA) (with minimum qualification of a bachelor degree) were trained on spirometry for 2 weeks (1 week in the clinic and 1 week in the community), and we evaluated their performance of administration of spirometry. We provided a spirometry manual translated into the local language (Bengali). FRAs initially conducted tests on volunteers under the supervision of physicians before starting actual data collection.
In the community, FRAs first evaluated if the participant was eligible for spirometry and then explained and demonstrated the procedure to each eligible participant. The FRA then asked the participant to perform spirometry to demonstrate whether she/he could perform it satisfactorily. If failed, the FRA provided further training to the participant. The participant performed at least three maneuvers, which the spirometer graded as A, B or C. If a participant failed to perform spirometry successfully within a session of a maximum of 8 blows, then another session was attempted after a few minutes of rest. If the participant failed to complete spirometry after 2 successive sessions, the test was rescheduled for another day.
The spirometer showed the value of the lung function parameters including Forced Vital Capacity (FVC), Forced Expiratory Volume in 1 second (FEV1), and ratio of FEV1 and FVC. Each spirometry report (spirogram) was printed and reviewed by a research investigator or physician and if found unacceptable, the procedure was repeated.
Participants who demonstrated a ratio of FEV1 to FVC <0.70 found during spirometry at home were considered potential COPD cases. They were then invited to the clinic for a reversibility test comprising of pre- and post-bronchodilator spirometry. Those who had FEV1 to FVC ratio <0.70 at pre-bronchodilator test underwent nebulisation with short-acting bronchodilator (5 mg salbutamol) followed by spirometry after 10 to 15 minutes. Participants with post-bronchodilator ratio of FEV1 to FVC < 0.70 were defined as COPD cases.
The US National Health and Nutrition Examination Survey (NHANES) III reference equations were used with Asian population corrections (100%) to detect percent predicted values. Severity of COPD was defined as stage I if FEV1 ≥80% predicted, as stage II if ≥50% FEV1 < 80% predicted, and stage III ≥30% FEV1 <50% predicted and as stage IV if FEV1 ≤30% predicted. As the GOLD fixed criteria is prone to overestimating COPD prevalence particularly in older population, we also assessed the prevalence using the lower limit of normal (LLN) defined as lower fifth percentile for the predicted FEV1/FVC in post-bronchodilator spirometry. The prevalence of COPD estimates provided by both fixed criteria of GOLD (Post-bronchodilator FEV1/FVC < 0.70) and the LLN method were compared. Participants were informed about their lung function status. Those diagnosed with COPD were given general health advices and they were counselled to seek care from qualified medical practitioner.
The sample size estimate was based on a reported prevalence of COPD of between 3.7 to 6.8%, which were observed in two studies that used spirometry to define COPD (22, 23). A sample size of 3660 participants were enrolled (1830 in each site, considering 10% refusal rate) to detect the COPD prevalence with 80% power at 5% significance level. Age and sex specific differences in COPD prevalence were considered that assumed a higher rate in older age groups and 25% higher among males than females in each stratum of age groups.
Data was entered on computers using MS Access with built in range and consistency checks. Categorical variables were presented as frequencies with percentages and continuous variables as mean with standard deviation. The chi-square test was used to assess the association between categorical variables and Student's t-test for comparing the means of continuous variables.
Conditional logistic regression was performed to determine independent factors associated with COPD defined by both fixed cutoff and LLN criteria. It included COPD as binary outcome variable (y/n) and age, sex, area of residence (rural, urban), educational attainment (illiterate, literate), household income (low, high), body mass index (BMI), ever smokers (current, former), solid fuel use, and history of asthma as independent variables. A conditional logistic regression model was used with a maximum likelihood estimation to compare models and identify confounders. Statistical analyses were carried out using SPSS for Windows version 17 (SPSS, Chicago, IL, USA). A p-value < 0.05 was considered statistically significant.
Results
Sample demographics
A total of 3759 respondents were interviewed from two study sites, both rural (n = 1910) and urban (n = 1849), and lung function was measured from 3744 (99.6%) individuals (urban n = 1895 and rural n = 1849). Lower limit of normal (LLN) of different lung function parameters was available for 3594 spirometry reports (urban: n = 1761, rural: n = 1833), which were considered for COPD prevalence estimation (Figure ). Sociodemographic characteristics of the participants with complete data are presented in Table . On average, respondents were 54 years old and 46% of them were male. The majority of the participants were non manual workers, illiterate and low income. The urban and rural sample differed significantly by age, occupation, education, income and lung function parameters (FEV1, FVC, ratio of FEV1/FVC) (Table ).
Table 1. Characteristics of the respondents by area of residence
Smoking
Overall, 37% of the respondents were ever smokers (22.7% current smoker and 14.6% former) with average smoking intensity of about 20 pack-years (Table ). Among the study participants 78% of men and 3% of women were smokers. Men were also heavier smokers than women (20.2 pack-years vs. 7.4 pack-years). Smoking status or intensity of smoking did not differ significantly between rural and urban participants (Table ), although the type of cigarette differed; rural participants consumed more bidis (small, thin, hand-rolled cigarettes) and urban smokers consumed more conventional cigarettes (filtered, national and international brands).
Prevalence of COPD
The overall prevalence of COPD was 13.5% (95% CI, 12.4–14.6) ( ) according to GOLD diagnostic criteria and 10.3% (95% CI, 9.3–11.3) by LLN criteria (Figure 2b). Prevalence was three times higher in males compared to females (22% VS 6.4% by GOLD criteria and 16.2% VS 5.3% by LLN criteria) and about 60% higher in rural than urban populations (17% VS 9.9% by GOLD criteria and 12.5% VS 8% by LLN criteria) (Table ). COPD was higher among individuals from households using biomass fuel compared to clean fuel (natural gas) users (17.3% VS 9.9% by GOLD criteria and 12.7% VS 7.9% by LLN criteria) (Table ). The prevalence of stage I (mild), stage II (moderate), stage III (severe), and stage IV (very severe) COPD was 2.7, 8, 2.3, and 0.6%, and by the GOLD severity criteria and 1.2, 6.4, 2.2 and 0.5% by the LLN criteria. Increase in GOLD-defined COPD relative to the LLN largely occurred in those aged 60–69 years (Table ), More than half of the COPD cases were stage II COPD by both criteria (-2b). More severe forms of COPD were more prevalent among male than female participants. The prevalence of COPD stage I and stage II was higher when classified by GOLD fixed cut-off compared to the LLN criteria. However, the prevalence of more severe forms of COPD (Stage III and IV) were similarly classified by both criteria.
Figure 2 a. Prevalence and stage of COPD (by GOLD criteria). b. Prevalence and stage of COPD (by LLN criteria).
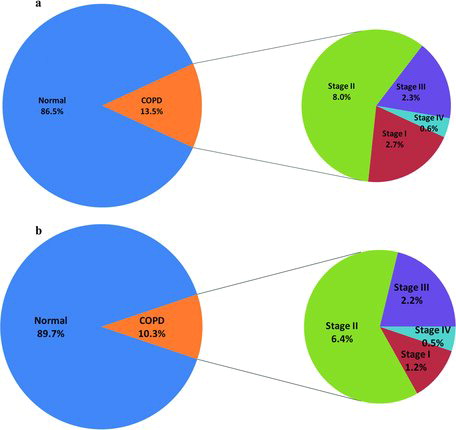
Figure 3 a. Prevalence of COPD by smoking status and type of fuel use (by GOLD criteria). b. Prevalence of COPD by smoking status and type of fuel use (by LLN criteria).
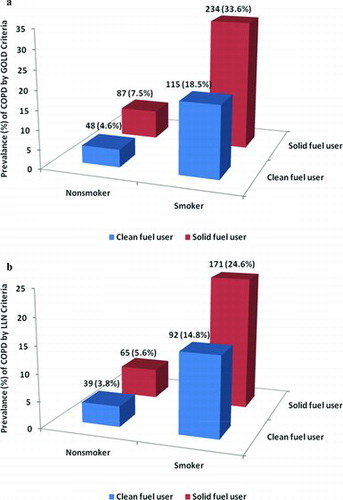
Table 2. Prevalence of COPD by different criteria and sociodemographic characteristics
Determinants of COPD
Higher prevalence of COPD was observed among older age groups, males, rural participants, illiterate individuals, manual workers, low income groups, smokers (current or former), those with a history of asthma, and solid fuel users (Table ). Conditional logistic regression identified independent determinants of COPD (Table ). The odds of having COPD increased with age but was inversely associated with the level of literacy. Both current smokers and ex-smokers had a higher probability of developing COPD. Biomass fuel use in households was also significantly associated with COPD (Table ). A history of asthma increased the odds of having COPD by seven fold, while being underweight was associated with a higher probability of COPD than normal or overweight.
Table 3. Determinants of COPD (adjusted model)
Discussion
This is the first population-based study that measured the community prevalence of COPD in both urban and rural settings in Bangladesh using objective lung function measures. Besides identifying community prevalence of COPD, this study also explored socioeconomic and lifestyle factors associated with COPD. We found 10.3 to 13.5% of people (based on LLN/GOLD) of 40 years of age or older in Bangladesh suffered from COPD, although only 1.2% reported having COPD (emphysema, chronic bronchitis) suggesting the condition is largely unrecognized and undiagnosed despite the high burden of COPD in the population. This has significant implications for health, quality of life and survival for a significant proportion of Bangladeshi adults aged 40 years or older. Under-diagnosis of COPD, particularly in milder stages, is common. In one study in the United States, 65% of COPD cases, including 44% with FEV1<50% predicted, were never diagnosed (19).
The observed overall prevalence of COPD in this study is higher compared to similar studies conducted in Japan (10.9%)(24) and Poland (10.7%)(25). Prevalence is also higher than the expected range of prevalence (4% to 10%) reported in a recent review of literature on COPD prevalence (26). However, the prevalence was within the range reported in resource poor settings such as cities in Latin America (12.1–19.7%) (27). It is expected that objective definitions using spirometry data tend to overestimate the prevalence compared to patient self-reported diagnoses (6).
Our findings are consistent with other studies that reported COPD being more prevalent in men, rural communities, and in older age groups (5, 7, 28). Such gender and community variability in prevalence may result from differences in tobacco smoking and other risk factors such as higher exposure to indoor air pollution in rural settings due to extensive use of biomass fuel in the traditional cook stove, for both cooking and heating.
Age is a well-established risk factor for COPD and we observed nearly three to five times higher prevalence of COPD among ages 60 years or older compared to ages 40 to 49 years. A similar steep increase in COPD prevalence by age has also been reported by others (29). Bangladesh is undergoing a rapid demographic and epidemiological transition in which mortality and morbidity due to non-communicable diseases are increasing (30). These shifts have great implications for COPD as it occurs more often in older than younger people. Older males in Bangladesh appear to be especially more susceptible to COPD. More than 50% of adult males over 25 years in Bangladesh (20 million men) smoke compared to less than 2% of females (12). In a recent study it was shown that 25% of all deaths in Bangladeshi men aged 25 to 69 are attributed to smoking. In 2010, this amounted to 42,000 excess adult male deaths due to smoking (31).
Smoking is an established risk factor for COPD. Studies revealed that 10 to 15% of all smokers develop COPD and smokers are three times more at risk of developing COPD compared to never/non-smokers (18, 32). The type of tobacco smoking, duration and quantity of smoking are also strong predictors of COPD (32, 33). In our study we found that 20 to 26% of the smokers had COPD (26.1% by GOLD; 19.6% by LLN). Despite significant differences in smoking history between males and females, more than 90% of the males with COPD (93.4% by GOLD; 94.4% by LLN) and about 11% of the females with COPD were smokers (10.4% by GOLD; 12.6% by LLN).
Our unadjusted data showed that ex-smokers had higher COPD prevalence by GOLD criteria than current smokers, which is consistent with findings from other studies (7, 13), but after adjustment for other variables, current smokers had higher odds of having COPD. This might be due to the longer duration and higher intensity of smoking as current smokers smoked 21.6 pack-years compared to ex-smokers who smoked 16.5 pack-years. Nearly a third of patients with COPD were non-smokers, and the overall prevalence of COPD among never smokers was 6.1% by GOLD criteria and 4.7% by LLN criteria, suggesting risk factors other than smoking might also play a significant role in the development of COPD in Bangladesh. This requires further investigation.
A significantly higher rate of COPD was found among individuals from households using biomass fuel compared to clean fuel (natural gas) users irrespective of smoking habits (Figures 3a–3b). We observed almost 98% of the rural participants and only 4% of the urban participants used biomass fuel for cooking and heating. Among non-smoker males, COPD prevalence was not significantly different by fuel type (3.4% in clean fuel users vs 4.6% in solid fuel users). However, COPD was 70% more common among non-smoker females from biomass fuel using households compared to clean fuel using households (3.8% in clean fuel users VS 5.8% in solid fuel users).
In Bangladesh, males rarely cook and commonly spend most of their time outdoors. Females are likely to experience greater exposure to indoor air pollution caused by biomass burning in traditional cook stoves as most of Bangladeshi females cook for the family. This may explain the higher rate of female COPD observed in solid fuel using households. Our findings are consistent with other studies that found the use of solid fuel poses a higher risk of developing COPD, especially in women (34, 35). A recent retrospective cohort study in Bangladesh reported 2.4-fold higher respiratory mortality associated with biomass fuel use compared to clean fuel use (36).
In this study, we found a strong association between history of asthma and COPD. History of asthma had 7-times-higher probability of having COPD, even after adjusting for smoking history and other potential confounders. A similar association was reported in a 20-year follow-up study in which active asthmatics were found 12.5 times more likely to fulfill criteria consistent with COPD (37). As shown in the present study, the risk of COPD was significantly higher in those with both lower BMI and less education. It has been established that COPD is linked to socioeconomic status (SES), which is usually measured by income or educational level (34). However, the causal relationship between BMI and COPD remains largely unexplored.
In our study, the prevalence estimates are drawn from a representative subset of the population (adults ≥40 years) using objective measures of lung function parameters taken with a high quality, robust spirometer by trained personnel following standard protocol. All suspected COPD cases in the community were confirmed in the clinic by post-bronchodilator spirometry, which ensured exclusions of those with reactive airway diseases or asthma. We ensured all spirograms were carefully examined against preset criteria by the investigators before inclusion for assessment.
One of the limitations of defining COPD through the GOLD fixed criteria was overestimation among the elderly population (38), which is reflected in our study both by prevalence (Table ) and odds ratios (Table ). Such overestimation by GOLD compared to LLN criteria mostly occurred in milder forms of COPD (stage I and II)(Figures 2a–2b). The lower limit of normal threshold (LLN) was also evaluated to define COPD. The absence of a reference equation for this particular population was also a concern and major challenge. However, the NHANES-III equation with Asian population correction (100%) was the closest acceptable equation to detect predicted percentages of different lung function parameters which we used to define different stages of COPD.
The American Thoracic Society's publication, Lung Function Testing: Selection of Reference Values and Interpretative Strategies (Citation39) does not have a separate calculation for Asian or mixed ethnic group which limited us to consider the default adjustment of 100% of the Caucasian values for Asian population correction by the EasyOne spirometer (40). Few of the suspected COPD cases (9%) in the community, who could be potentially confirmed as COPD cases did not turn up to the clinic for the post-bronchodilator test which may have led to a slight underestimation of the true prevalence. Nonetheless, this study revealed an enormous burden of chronic obstructive pulmonary disease (COPD) existing as undiagnosed cases in Bangladesh and we hope this information will help design targeted interventions for this disease and to curb future increases.
Conclusion
COPD constitutes a huge hidden burden of disease in people of 40 years of age or older in Bangladesh. Our results highlight COPD as a major public health problem in Bangladesh and call for more research and action to be directed toward preventive measures and intensive efforts to target smoking cessation and reduction of indoor air pollution due to biomass fuel burning.
Acknowledgement
We gratefully acknowledge the study participants and Health and Demographic Surveillance staff at Matlab and Kamalapur sites. icddr,b acknowledges with gratitude the commitment of the it’s donors for their generous support to its research efforts.
Declaration of Interest Statement
The authors declare that they have no competing interests. This project has been funded in part with Federal funds from the United States National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, under the Contract No. HHSN26820900032C. The authors alone are responsible for the content and writing of the paper.
References
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of COPD: updated 2010. Global Initiative for Chronic Obstructive Lung Disease, 2010. Available from: http://www.goldcopd.com/Guidelines/guideline-2010-gold-report.html (Accessed October 12, 2013).
- World Health Organization (WHO). Chronic obstructive pulmonary disease (COPD) fact sheet 2013 [updated October 2013; cited 2013 12 Oct]. Available from: http://www.who.int/mediacentre/factsheets/fs315/en/ (Accessed October 12, 2013).
- Lopez AD, Shibuya K, Rao C, Mathers CD, Hansell AL, Held LS, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J 2006; 27(2):397–412. Epub 2006/02/03. doi: 27/2/397 [pii] 10.1183/09031936.06.00025805. PubMed PMID: 16452599.
- Mathers CD, Fat DM, Boerma JT. The global burden of disease: 2004 update: World Health Organization; 2008, Geneva, Switzerland.
- Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, et al. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet 2007; 370(9589):741–750. Epub 2007/09/04. doi: S0140-6736(07)61377-4 [pii] 10.1016/S0140-6736(07)61377-4. PubMed PMID: 17765523.
- Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J 2006; 28(3):523–532. Epub 2006/04/14. doi: 09031936.06.00124605 [pii] 10.1183/09031936.06.00124605. PubMed PMID: 16611654.
- Zhong N, Wang C, Yao W, Chen P, Kang J, Huang S, et al. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am J Respir Crit Care Med 2007; 176(8):753–760. Epub 2007/06/19. doi: 200612-1749OC [pii] 10.1164/rccm.200612-1749OC. PubMed PMID: 17575095.
- McKay AJ, Mahesh PA, Fordham JZ, Majeed A. Prevalence of COPD in India: a systematic review. Prim Care Respir J 2012; 21(3):313–321. Epub 2012/07/14. doi: pcrj-2012-02-0034-R1 [pii] 10.4104/pcrj.2012.00055. PubMed PMID: 22790612.
- Islam M, Hossain M, Pasha M, Azad A, Murshed K. Prevalence and risk factors of chronic obstructive pulmonary disease (COPD) in Dhaka city population. Mymensingh Med J 2013; 22(3):547–551.
- Stang P, Lydick E, Silberman C, Kempel A, Keating ET. The prevalence of COPD using smoking rates to estimate disease frequency in the general population. Chest J 2000; 117(5_suppl_2):354S–359S.
- World Health Organization (WHO). Global Adult Tobacco Survey: Bangladesh Report 2009. Bangladesh: WHO, 2009.
- Bangladesh Society of Medicine. Bangladesh NCD Risk Factor Survey2010. Dhaka, Bangladesh: Director General of Health Services, 2011.
- Chan-Yeung M, Ho AS, Cheung AH, Liu RW, Yee WK, Sin KM, et al. Determinants of chronic obstructive pulmonary disease in Chinese patients in Hong Kong. Int J Tuberc Lung Dis 2007; 11(5):502–507. Epub 2007/04/19. PubMed PMID: 17439672.
- Salvi SS, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009; 374(9691):733–743. Epub 2009/09/01. doi: S0140-6736(09)61303-9 [pii] 10.1016/S0140-6736(09)61303-9. PubMed PMID: 19716966.
- Rehfuess E, Mehta S, Prüss-Üstün A. et al. Assessing household solid fuel use: multiple implications for the Millennium Development Goals. Environ Health Perspect 2005; 114(3):373–378.
- Guder G, Brenner S, Angermann CE, Ertl G, Held M, Sachs AP, et al. GOLD or lower limit of normal definition? A comparison with expert-based diagnosis of chronic obstructive pulmonary disease in a prospective cohort-study. Respir Res 2012; 13(1):13. doi: 10.1186/1465-9921-13-13. PubMed PMID: 22309369; PubMed Central PMCID: PMC3299632.
- Swanney MP, Ruppel G, Enright PL, Pedersen OF, Crapo RO, Miller MR, et al. Using the lower limit of normal for the FEV1/FVC ratio reduces the misclassification of airway obstruction. Thorax 2008; 63(12):1046–1051. doi: 10.1136/thx.2008.098483. PubMed PMID: 18786983.
- Pauwels RA, Buist AS, Calverley PMA, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Amer J Respirat Crit Care Med 2001; 163(5):1356–1276.
- Ginneken JV, Bairagi R, Francisco AD, Sarder AM, Vaughan P. Health and demographic surveillance in Matlab: past, present, and future, Dhaka: International Centre for Diarrhoeal Disease Research, Bangladesh, 1999.
- International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b). Registration of Health and Demographic Events 2011. Dhaka: International Centre for Diarrhoeal Disease Research, Bangladesh, 2012.
- International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b). Kamalapur 2005–2007 Census Results. Dhaka: International Centre for Diarrhoeal Disease Research, Bangladesh, 2008.
- Lange P, Groth S, Nyboe J, Appleyard M, Mortensen J, Jensen G, et al. Chronic obstructive lung disease in Copenhagen: cross-sectional epidemiological aspects. J Intern Med 1989; 226(1):25–32. Epub 1989/07/01. PubMed PMID: 2787829.
- Mannino DM, Gagnon RC, Petty TL, Lydick E. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med 2000; 160(11):1683–1689. Epub 2000/06/10. PubMed PMID: 10847262.
- Fukuchi Y, Nishimura M, Ichinose M, Adachi M, Nagai A, Kuryama T, et al. COPD in Japan: the Nippon COPD Epidemiology study. Respirology. 2004(9):458–465.
- Plywaczewski R, Bednarek M, Jonczak L, J Z. Prevalence of COPD in Warsaw population. Pneumonol Alergol Pol. 2003; 71:329–335.
- Halbert RJ, Isonaka S, George D, Iqbal A. Interpreting COPD prevalence estimates: what is the true burden of disease? Chest 2003; 123(5):1684–1692. Epub 2003/05/13. PubMed PMID: 12740290.
- Menezes AM, Perez-Padilla R, Jardim JR, Muino A, Lopez MV, Valdivia G, et al. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet 2005; 366(9500):1875–81. Epub 2005/11/29. doi: S0140-6736(05)67632-5 [pii] 10.1016/S0140-6736(05)67632-5. PubMed PMID: 16310554.
- Tzanakis N, Anagnostopoulou U, Filaditaki V, Christaki P, Siafakas N. Prevalence of COPD in Greece. Chest 2004; 125(3):892–900. Epub 2004/03/10. PubMed PMID: 15006947.
- Schirnhofer L, Lamprecht B, Vollmer WM, Allison MJ, Studnicka M, Jensen RL, et al. COPD prevalence in Salzburg, Austria: results from the Burden of Obstructive Lung Disease (BOLD) Study. Chest. 2007; 131(1):29–36. Epub 2007/01/16. doi: 131/1/29 [pii] 10.1378/chest.06-0365. PubMed PMID: 17218553.
- Ahsan Karar Z, Alam N, Kim Streatfield P. Epidemiological transition in rural Bangladesh, 1986–2006. Glob Health Action 2009; 2. Epub 2009/12/23. doi: 10.3402/gha.v2i0.1904. PubMed PMID: 20027273.
- Alam DS, Jha P, Ramasundarahettige C, Streatfield PK, Niessen LW, Chowdhury MA, et al. Smoking-attributable mortality in Bangladesh: proportional mortality study. Bull World Health Organ 2013; 91(10):757–764. Epub 2013/10/12. doi: 10.2471/BLT.13.120196 BLT.13.120196 [pii]. PubMed PMID: 24115799.
- Bhome AB. COPD in India: Iceberg or volcano? J Thorac Dis 2012; 4(3):298–309.
- Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years' observations on male British doctors. Br Med J 2004; 328(7455):1519.
- Ekici A, Ekici M, Kurtipek E, Akin A, Arslan M, Kara T, et al. Obstructive airway diseases in women exposed to biomass smoke. Environ Res. 2005;99(1):93–98. Epub 2005/08/02. doi: S0013-9351(05)00006-X [pii] 10.1016/j.envres.2005.01.004. PubMed PMID: 16053933.
- Kurmi OP, Semple S, Simkhada P, Smith WC, Ayres JG. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax 2010; 65(3):221–228. Epub 2010/03/26. doi: 65/3/221 [pii] 10.1136/thx.2009.124644. PubMed PMID: 20335290.
- Alam DS, Chowdhury MAH, Siddiquee AT, Ahmed S, Hossain MD, Pervin S, et al. Adult cardiopulmonary mortality and indoor air pollution: a 10-year retrospective cohort study in a low-income rural setting. Global Heart 2012; 7(3):215–221.
- Silva GE, Sherrill DL, Guerra S, Barbee RA. Asthma as a risk factor for COPD in a longitudinal study. Chest 2004; 126(1):59–65. Epub 2004/07/14. doi: 10.1378/chest.126.1.59126/1/59 [pii]. PubMed PMID: 15249443.
- Hardie JA, Buist AS, Vollmer WM, Ellingsen I, Bakke PS, Mørkve O. Risk of over-diagnosis of COPD in asymptomatic elderly never-smokers. Euro Respir J 2002; 20:1117–1122.
- American Thorasic Society. Lung function testing: selection of reference values and interpretative strategies. American Thoracic Society. Amer Rev Respir Dis 1991; 144(5):1202–1218. doi: 10.1164/ajrccm/144.5.1202. PubMed PMID: 1952453.
- ndd Medizintechnik AG. ndd EasyGuide Operator's Manual. EasyOne™ Spirometer Zürich, Switzedland: ndd Medizintechnik AG, 2011.

