To the Editor:
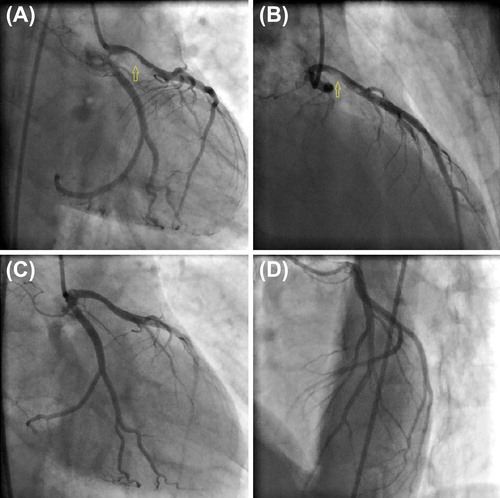
A 40-year-old homeless man without previous medical history presented to the emergency department with chest pain 2 h after he had inhaled thinner for the first time. On admission, his arterial blood pressure was 145/95 mmHg and his heart rate was 106 beats/min. Electrocardiography (ECG) revealed mild sinus tachycardia with poor R-wave progression in leads V1–V6 (). His serum biomarkers of myocardial injury were elevated and his Troponin I, CK, and CK-MB levels were 41.6 ng/dl (0–0.04 ng/dL), 383 U/L, and 93 U/L, respectively. Other routine laboratory results including platelet count, electrolyte levels, renal function, liver function, and coagulation tests [i.e., INR, PT, aPTT, and bleeding time were 0.9 (0.8–1.2), 11 s (9.7–14 s), 29 s (16–36 s), and 3.4 min (2–5 min), respectively] were normal. Following the administration of a loading dose of clopidogrel (600 mg) and acetylsalicylic acid (300 mg), he was immediately taken to the catheterization laboratory for urgent angiography and was diagnosed with acute anterior myocardial infarction. Coronary angiography revealed critical thrombotic stenosis at the proximal segment of the left anterior descending artery (LAD) ( and , Supplementary Movies 1 and 2 to be found online at http://informahealthcare.com/doi/abs/10.3109/15563650.2013.818683). Nonstenotic atherosclerotic plaques in the circumflex and right coronary arteries were also noted. Because of extensive thrombus burden, the patient was given 25 μg/kg Tirofiban over 3 min by intravenous bolus, which was followed by an infusion of 0.15 μg/kg Tirofiban per minute for 24 h. After 3 days, repeated coronary angiography demonstrated patent LAD with no residual stenosis ( and , Supplementary Movies 3 and 4 to be found online at http://informahealthcare.com/doi/abs/10.3109/15563650.2013.818683). The patient's in-hospital course was uneventful and he was discharged from the hospital after 7 days without any complaints.
Fig. 1. Electrocardiogram (ECG) showing sinus tachycardia with poor R-wave progression in precordial leads.
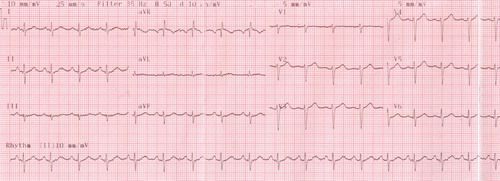
Fig. 2. (A and B) Selective left coronary angiogram showing severe thrombotic stenosis at the proximal portion of the left anterior descending artery (yellow arrows). (C and D) Selective left coronary angiogram obtained 3 days after intravenous Tirofiban infusion showing patent left anterior descending artery without residual stenosis.
Paint thinner, which is commonly used as a cleaning agent to dilute household paints, ink, and adhesives, contains a mixture of various halogenated and aromatic hydrocarbons (e.g., toluene, xylene, N-hexane, and benzene).Citation1,Citation2 Recent studies suggest that the prevalence of volatile substance abuse to achieve a euphoric state was 73% among homeless children in Istanbul, Turkey.Citation3 Following skin contact or inhalation of thinner, hydrocarbon ingredients, especially toluene, rapidly diffuse into the blood because of their lipophilic properties and easily penetrate tissues that are rich in lipids (e.g., the central nervous system, lung, kidney, liver, and adrenal gland). In target tissues, toluene is oxidized by monooxidase enzymes, and as a result of this oxidation, extensive free radicals are released, causing tissue damage.Citation4 Toluene is one of the most important components of paint thinner, and it can cause dyspnea, tachypnea, central nervous system toxicity (euphoria, ataxia, convulsions, tremor, and coma), renal tubular acidosis, and electrolyte abnormalities (especially hypophosphatemia).
Acute coronary syndrome (ACS) is relatively very rare when compared to other cardiovascular manifestations such as atrial or ventricular arrhythmias (by effecting myocardial sodium channels), sudden cardiac death, myocarditis, and dilated cardiomyopathy (by causing hypophosphatemia). In our case, the main clinical presentation of thinner intoxication was associated with acute myocardial infarction. Thus far, only a few cases of acute myocardial infarction associated with thinner (toluene) abuse have been reported (), and therefore clinical experience with such cases is limited.Citation5–8 The exact mechanism of ACS due to thinner inhalation is not well known. However, possible mechanisms include coronary vasospasm caused by an increased sensitivity to catecholamines, a decrease in cardiac output, nonperfusing arrhythmias, and the development of severe renal tubular acidosis, which effects platelet function and the coagulation cascade.Citation6,Citation8 Based on what we saw in our case, coronary thrombus formation may also be one of the possible mechanisms. The management of thinner-induced acute myocardial infarction should be no different from the management of classical acute myocardial infarction. Percutaneous coronary intervention could serve as a basic treatment for cases with hemodynamic instability, the development of life-threatening arrhythmias, or with ST segment elevation myocardial infarction. In the absence of these conditions, anticoagulant or antiaggregant treatment such as glycoprotein IIb/IIIa inhibitors could be performed, particularly in the ACS cases with massive thrombus burden.
Table 1. Case reports of acute myocardial infarction associated with thinner abuse.
In conclusion, myocardial infarction associated with thinner abuse is very rare and may be life-threatening. Therefore, follow-up with ECG and cardiac enzymes should be considered for the early detection of coronary events in a patient with thinner intoxication. In such cases, coagulation and platelet function tests should also be performed.
Supplementary Movies 1 to 4
Download PDF (161.9 KB)Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Inoue T, Ikeda M, Ogata M, Saito K, Sakurai H, Takeuchi Y, et al. [A nationwide survey on the use of organic solvents in Japan]. Sangyo Igaku 1984; 26:518–538.
- Saito J, Ikeda M. Solvent constituents in paint, glue and thinner for plastic miniature hobby. Tohoku J Exp Med 1988; 155:275–283.
- Ogel K, Taner S, Eke C, Erol B. Report of the prevelance of tobacco, alcohol and substance abuse amongst 10th grade students in Istanbul. Publication number 15. Istanbul, 2005.
- Halifeoglu I, Canatan H, Ustundag B, Ilhan N, Inanc F. Effect of thinner inhalation on lipid peroxidation and some antioxidant enzymes of people working with paint thinner. Cell Biochem Funct 2000; 18:263–267.
- Vural M, Dayı SU, Tartan Z, Kaşikçioğlu H, Okmen E, Cam N. [A case of myocardial infarction developed after paint thinner exposure]. Anadolu Kardiyol Derg 2003; 3:363–365.
- Carder JR, Fuerst RS. Myocardial infarction after toluene inhalation. Pediatr Emerg Care 1997; 13:117–119.
- Hussain TF, Heidenreich PA, Benowitz N. Recurrent non-Q-wave myocardial infarction associated with toluene abuse. Am Heart J 1996; 131:615–616.
- Cunningham SR, Dalzell GW, McGirr P, Khan MM. Myocardial infarction and primary ventricular fi brillation after glue sniffing. Br Med J (Clin Res Ed) 1987; 294:739–740.