Abstract
Background and purpose The first generations of total ankle replacements (TARs) showed a high rate of early failure. In the last decades, much progress has been made in the development of TARs, with the newer generation showing better results. We evaluated TARs implanted with rheumatoid arthritis (RA) or juvenile inflammatory arthritis (JIA) as indication.
Patients and methods 58 total ankle prostheses (Buechel-Pappas and STAR type) were implanted in patients with RA (n = 53) or JIA (n = 5) in 54 patients (4 bilateral). After a mean follow-up of 2.7 (1–9) years, all patients were reviewed by two orthopedic surgeons who were not the surgeons who performed the operation. Standard AP and lateral radiographs were taken and a Kofoed ankle score was obtained; this is a clinical score ranging from 0–100 and consists of sub-scores for pain, disability, and range of motion.
Results 2 patients died of unrelated causes. Of the 52 patients who were alive (56 prostheses), 51 implants were still in place and showed no signs of loosening on the most recent radiographs. The mean Kofoed score at follow-up was 73 points (SD 16, range 21–92). 4 patients showed a poor result (score < 50) with persistent pain for which no obvious reason could be found. 5 implants were removed, 4 because of infection and 1 because of aseptic loosening.
Interpretation Medium-term results of the STAR and BP types of TAR in RA were satisfactory. The main reason for failure of the implant was infection.
The standard treatment for end-stage arthritis of the ankle joint due to rheumatoid arthritis (RA) has been an ankle fusion. In the last decades, much progress has been made in the development of total ankle replacements (TARs). Most TARs are implanted in patients with RA and posttraumatic arthritis. The first generations of TARs were implants with 2 parts, one inserted in the distal tibia and one placed on top of the talus. These implants showed a high rate of early failure, especially early loosening. The current TARs consist of three components, a metal implant placed in the distal tibia, a metal component in the talus, and a polyethylene insert in-between. These implants allow a certain amount of gliding and rotation, whereas the previous more constrained prostheses behaved as a hinge.
This study was undertaken to evaluate all TARs implanted at our centers in patients with RA or juvenile inflammatory arthritis (JIA) as indication.
Patients and methods
Patient characteristics ()
Between 1996 and 2004, 58 total ankle prostheses were implanted in 54 patients with RA or JIA (53 and 5 TARs, respectively; 4 bilateral) at the Radboud University Nijmegen Medical Center and Sint Maartenskliniek, both in Nijmegen, the Netherlands. 48 implants were placed in women, and 10 in men. Mean age at the time of operation was 55 (27–82) years. All patients were operated by experienced senior orthopedic surgeons (JWL, MdWM) using the same technique.
Types of implants and surgical technique
Two different implants were used, both consisting of 2 metal components and a polyethylene bearing. One surgeon (JWL) always used the Scandinavian-Type Ankle Replacement (STAR, Waldemar Link, Hamburg, Germany) (n = 29), while the other surgeon (MdWM) used the same implant for 3 years (n = 8); the rest of the implants were Buechel-Pappas type (BP; Endotec, South Orange, NJ) (n = 21) ().
After antibiotic prophylaxis (1 gram Cefazolin i.v.) and placement of a tourniquet, an anterior approach was used. After mobilization of the neurovascular bundle to the lateral side, the joint was opened and the synovium excised. The bony surfaces of the distal tibia and the talus were prepared for placement of the 2 metal components, whereafter the polyethylene bearing was inserted in-between. The wound was closed over a suction drain, which was removed on the second postoperative day. After the postoperative swelling had diminished, a lower leg cast was applied. Antithrombotic prophylaxis was by means of 0.3 mL nadroparin subcutaneously for 6 weeks. Patients started weight bearing after 2 weeks, when a walking cast was applied. After 4 weeks, the cast was removed and patients could start to ambulate as tolerated and to practice movement of the artificial joint. Normally, physiotherapy was not needed.
Outcome measures
After a mean follow-up of 2.7 (1–9) years, all patients were reviewed by 2 orthopedic surgeons who were not the surgeons who performed the operation. Standard AP and lateral radiographs were taken and a Kofoed score was obtained. We analyzed 2 forms of failure: firstly, the traditional failure rate consisting of removal of the prosthesis or amputation. The second endpoint was defined as removal of the prosthesis for any reason or a clinical score below 50.
Results
Complications
During implantation of the prostheses, 10 cases sustained a medial malleolar fracture, 3 a lateral malleolar fracture, and in 3 patients a fracture of the posterior part of the tibial plafond occurred. The occurrence of a fracture was unrelated to the type of implant used, the surgeon, or the total number of implants the surgeon had placed before. The posterior tibial plafond fractures and 6 medial malleolar fractures were treated with the normal aftercare (6 weeks with below-knee walking cast) and healed uneventfully. The 3 lateral malleolar fractures and the remaining medial fractures were treated with reduction and internal fixation (malleolar screw on the medial side; lag screw and neutralization plate on the lateral side).
One implant became infected after a wound-healing problem over a medial malleolar fracture, which had been treated with osteosynthesis. This implant was removed and the ankle was fused 6 months after the index operation. Another implant lost its tibial fixation and had to be removed; a fusion was performed subsequently. The remaining 14 fractures healed uneventfully. 3 patients had early surgical site infections that were treated by exploration of the surgical site and debridement of the wound, and systemic and local antibiotics. 2 early infections were treated successfully. In the other patient, the implant had to be removed and an ankle fusion was performed.
Two chronic infections occurred, the first was the above-mentioned patient with a wound-healing problem over a fracture. Initially, the wound appeared to heal well but after a few weeks the patient developed a deep infection, which was treated by removal of the implant and fusion of the ankle, 6 months after the index operation. Another late infection was seen 4 years after implantation of the TAR; this patient had an ipsilateral infected total knee replacement. Both the infected knee prosthesis and the TAR could not be treated adequately with antibiotics and several surgical debridements, and she underwent an above-knee amputation.
One STAR talar component showed symptomatic migration and was removed after 4.2 years, and the ankle was subsequently fused.
A summary of all complications is given in .
Table 1. Summary of complications and outcome.
Outcome
2 patients died of an unrelated cause 4 and 4.3 years after unilateral TAR operations; at the last follow-up there had been no radiographic signs of loosening.
In the 52 patients who were alive at the latest follow-up (56 prostheses), 51 implants were still in place after a mean follow-up of 2.7 (1–9) years. The mean Kofoed ankle score at follow-up was 73 points (SD 16, range 21–92). 4 patients showed a poor result (with a Kofoed score of < 50). These 4 patients all had persistent pain, for which no obvious reason could be found ().
Table 2. Results in relation to the type of implant used.
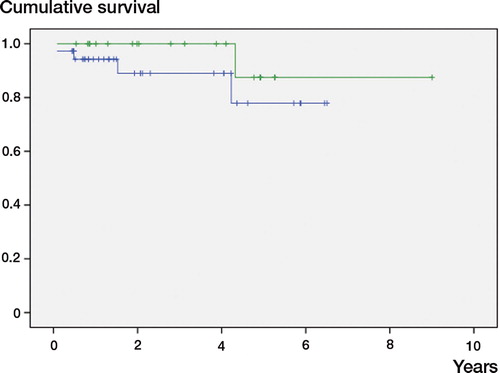
With removal of the implant as endpoint, the success rate was over 92% (). Taking clinical failure (Kofoed score < 50) into account, the success rate was 88%. A logistic regression analysis with implant failure as dependent variable showed that infection was the most important factor (p < 0.001). Type of implant (p = 0.08), surgeon (p = 0.4), peroperative fracture (p = 0.6), side operated (p = 0.7), and sex (p = 0.3) did not reach statistical significance. Logistic regression analysis with implant failure or a clinical score below 50 as endpoint showed the same results: infection was the only significant predictive factor (p < 0.01); type of implant (p = 0.08), surgeon (p = 0.8), peroperative fracture (p = 0.2), side operated (p = 0.6), and sex (p = 0.08) were not significant.
Figure 3. Kaplan-Meier survival curve with removal of the prosthesis as outcome measure. The green line represents the BP prosthesis, the blue line the STAR.
The relative risk (RR) of implant failure with or without infection was 15 (CI: 2–45). The RR of failure with or without a perioperative fracture was 1.66 (CI: 0.3–9).
Discussion
Total ankle replacement in RA showed good medium-term results in our series, similar to those in a recently published meta-analysis (Stengel et al. Citation2005). Early and especially late infection of the prosthesis is a major threat. The high incidence of peroperative fractures did not influence the outcome. It is important to recognize that complications such as peroperative fracture do not necessarily lead to a poor outcome; on the other hand, the absence of complications or radiographic findings does not guarantee a good clinical result. In many studies regarding the medium- or long-term results of endoprostheses, the endpoint has been revision for any reason. Failure may also be defined as patient dissatisfaction with the result of the procedure, regardless of the symptoms or physical findings (Hasan et al. Citation2002).
Rheumatoid arthritis frequently involves the hindfoot (Michelson et al. Citation1994, Klenerman Citation1995, Cracchiolo Citation1997). Unfortunately, this part of the foot is often overlooked when caring for these patients—who often have multiple areas of involvement giving pain and producing deformity. Early treatment consists of proper or custom-made footwear and occasional injections of corticosteroids (Cracchiolo Citation1997). Early synovectomy may be valuable, but it is controversial whether a synovectomy can halt the progression of joint destruction (Akagi et al. Citation1997, Nakamura et al. Citation2004). Ankle fusion is a well-established operation with few complications and good pain relief, and improvement in walking ability (Maenpaa et al. Citation2001, Panotopoulos et al. Citation2005, Winson et al. Citation2005).
With an arthrodesis of the talotibial joint, the normal function of the hindfoot is altered. This results in altered walking kinematics—especially an earlier heel-off—and this becomes worse when walking barefoot or with increased speed (Beyaert et al. Citation2004). The loss of ankle motion caused by an ankle fusion increases strain on the adjacent joints of the ipsilateral foot, and many patients develop degenerative changes in the subtalar and midtarsal joints (Mazur et al. Citation1979, Muir et al. Citation2002). It is important to know that in the literature prior to 1979, the results obtained with ankle arthrodesis were generally graded as good if arthrodesis was achieved or poor if nonunion resulted, so the result “good” or “poor” was only based on the radiograph; the clinical result was not taken into account (Abidi et al. Citation2000).
The advantages of total ankle replacement over ankle arthrodesis include preservation of motion and reduced stresses on the midfoot and subtalar joints (Su et al. Citation2004). Especially patients with rheumatoid arthritis may already have subtalar degeneration when they present with ankle pain, making ankle arthrodesis a less appealing treatment. Secondary procedures to the foot, and especially the subtalar joint, are often part of the surgical plan and are performed either before or simultaneously with ankle replacement (Greisberg et al. Citation2004).
The early TAR design components were highly constrained; these implants showed an unacceptable rate of loosening—as high as 50% within a few years (Dini and Bassett Citation1980, Newton Citation1982, Helm and Stevens Citation1986). This high failure rate is probably due to the greater stress at the bone-prosthesis interface, as constrained implants do not allow rotation and sliding during extension and flexion (Conti and Wong Citation2001). The current generation of implants, consisting of 3 components including a mobile polyethylene bearing, shows a lower loosening rate after medium-term follow-up (Buechel and Pappas Citation1992, Kofoed and Sorensen Citation1998, Kofoed and Lundberg-Jensen Citation1999, Buechel et al. Citation2002, Anderson et al. Citation2003, Buechel et al. Citation2003, Kofoed Citation2004, Su et al. Citation2004, Doets et al. Citation2006, San Giovanni et al. Citation2006). Both implants used in our series are well documented. The STAR prosthesis has shown comparable results in other studies (Kofoed and Sorensen Citation1998, Kofoed and Lundberg-Jensen Citation1999, Anderson et al. Citation2003, Wood and Deakin Citation2003, Kofoed Citation2004), as has the Buechel-Pappas type (Buechel and Pappas Citation1992, Buechel et al. Citation2002, Buechel et al. Citation2003, Su et al. Citation2004, Doets et al. Citation2006, San Giovanni et al. Citation2006). Most studies regarding the results of implants have been from the institute of the designer of the implant. The experience of these individuals, while valuable, is not necessarily representative of the experience of orthopedic surgeons in general. Furthermore, in most outcome studies different indications are included; in our study only RA and JIA patients were included.
In a radiostereometric analysis of the tibial component of the Buechel-Pappas type of implant, a migration of the tibial component of 0.9 mm was observed during the first 3 months, but this stabilized by the 6-month follow-up (Nelissen et al. Citation2006). We are not aware of any reports regarding the initial stability of the talar component of the BP prosthesis. For the STAR type, a similar migration pattern was found: some migration during the initial postoperative period but little or no migration after 6 weeks (Carlsson et al. Citation2005).
Although complications are commonly described and the surgery is technically demanding (Greisberg et al. Citation2004), in experienced hands and with a good indication, this kind of surgery may yield good results. However, a suboptimal placement of the prosthesis will lead to early failure (Greisberg et al. Citation2004). The results for patients with degeneration due to osteoarthritis do not differ from those suffering from rheumatoid arthritis (Kofoed and Sorensen Citation1998); furthermore, age does not seem to affect the outcome (Kofoed and Lundberg-Jensen Citation1999).
Compared to a standard ankle fusion, ankle fusion after a failed arthroplasty more often results in a non-union (Hopgood et al. Citation2006, Kotnis et al. Citation2006). In our group, 2 patients showed a delayed union—for which a new intervention was necessary, but all fusions united. Although the function of a total ankle prosthesis is never the same as a normal ankle joint and clinical results are sometimes poor when looking at a subjective score, patient satisfaction is higher than expected from these scores (Nishikawa et al. Citation2004).
Acknowledgments
Study design: HH and JWL; review of patients: HH and BS; data analysis and interpretation: HH, JWL, FvdH, and MdWM; preparation of manuscript: all authors.
As a fellow in rheumatoid arthritis surgery, Huub J.L. van der Heide has been partially sponsored by the Dutch Arthritis Association.
- Abidi NA, Gruen GS, Conti SF. Ankle arthrodesis: indications and techniques. J Am Acad Orthop Surg 2000; 8: 200–9
- Akagi S, Sugano H, Ogawa R. The long-term results of ankle joint synovectomy for rheumatoid arthritis. Clin Rheumatol 1997; 16: 284–90
- Anderson T, Montgomery F, Carlsson A. Uncemented STAR total ankle prostheses. Three to eight-year follow-up of fifty-one consecutive ankles. J Bone Joint Surg (Am) 2003; 85: 1321–9
- Beyaert C, Sirveaux F, Paysant J, Mole D, Andre JM. The effect of tibio-talar arthrodesis on foot kinematics and ground reaction force progression during walking. Gait Posture 2004; 20: 84–91
- Buechel FF, Pappas MJ. Survivorship and clinical evaluation of cementless, meniscal-bearing total ankle replacements. Semin Arthroplasty 1992; 3: 43–50
- Buechel FF, Sr., Buechel FF, Jr., Pappas MJ. Eighteen-year evaluation of cementless meniscal bearing total ankle replacements. Instr Course Lect 2002; 51: 143–51
- Buechel FF, Sr., Buechel FF, Jr, Pappas MJ. Ten-year evaluation of cementless Buechel-Pappas meniscal bearing total ankle replacement. Foot Ankle Int 2003; 24: 462–72
- Carlsson A, Markusson P, Sundberg M. Radiostereometric analysis of the double-coated STAR total ankle prosthesis. Acta Orthop 2005; 76(4)573–9
- Conti SF, Wong YS. Complications of total ankle replacement. Clin Orthop 2001, 391: 105–14
- Cracchiolo A, III. Rheumatoid arthritis. Hindfoot disease. Clin Orthop 1997, 340: 58–68
- Dini AA, Bassett FH, III. Evaluation of the early result of Smith total ankle replacement. Clin Orthop 1980, 146: 228–30
- Doets HC, Brand R, Nelissen RG. Total ankle arthroplasty in inflammatory joint disease with use of two mobile-bearing designs. J Bone Joint Surg (Am) 2006; 88: 1272–84
- Greisberg J, Hansen J, Digiovanni C. Alignment and technique in total ankle arthroplasty. Operative Techn Orthop 2004; 14: 21–30
- Hasan SS, Leith JM, Campbell B, Kapil R, Smith KL, Matsen FA, III. Characteristics of unsatisfactory shoulder arthroplasties. J Shoulder Elbow Surg 2002; 11: 431–41
- Helm R, Stevens J. Long-term results of total ankle replacement. J Arthroplasty 1986; 1: 271–7
- Hopgood P, Kumar R, Wood PL. Ankle arthrodesis for failed total ankle replacement. J Bone Joint Surg (Br) 2006; 88: 1032–8
- Klenerman L. The foot and ankle in rheumatoid arthritis. Br J Rheumatol 1995; 34: 443–8
- Kofoed H. Scandinavian Total Ankle Replacement (STAR). Clin Orthop 2004, 424: 73–9
- Kofoed H, Lundberg-Jensen A. Ankle arthroplasty in patients younger and older than 50 years: a prospective series with long-term follow-up. Foot Ankle Int 1999; 20: 501–6
- Kofoed H, Sorensen TS. Ankle arthroplasty for rheumatoid arthritis and osteoarthritis: prospective long-term study of cemented replacements. J Bone Joint Surg (Br) 1998; 80: 328–32
- Kotnis R, Pasapula C, Anwar F, Cooke PH, Sharp RJ. The management of failed ankle replacement. J Bone Joint Surg (Br) 2006; 88: 1039–47
- Maenpaa H, Lehto MU, Belt EA. Why do ankle arthrodeses fail in patients with rheumatic disease?. Foot Ankle Int 2001; 22: 403–8
- Mazur JM, Schwartz E, Simon SR. Ankle arthrodesis. Long-term follow-up with gait analysis. J Bone Joint Surg (Am) 1979; 61: 964–75
- Michelson J, Easley M, Wigley FM, Hellmann D. Foot and ankle problems in rheumatoid arthritis. Foot Ankle Int 1994; 15: 608–13
- Muir DC, Amendola A, Saltzman CL. Long-term outcome of ankle arthrodesis. Foot Ankle Clin 2002; 7: 703–8
- Nakamura H, Tanaka H, Yoshino S. Long-term results of multiple synovectomy for patients with refractory rheumatoid arthritis. Effects on disease activity and radiological progression. Clin Exp Rheumatol 2004; 22: 151–7
- Nelissen RG, Doets HC, Valstar ER. Early Migration of the Tibial Component of the Buechel-Pappas Total Ankle Prosthesis. Clin Orthop 2006, 448: 146–51
- Newton SE, III. Total ankle arthroplasty. Clinical study of fifty cases. J Bone Joint Surg (Am) 1982; 64: 104–11
- Nishikawa M, Tomita T, Fujii M, Watanabe T, Hashimoto J, Sugamoto K, Ochi T, Yoshikawa H. Total ankle replacement in rheumatoid arthritis. Int Orthop 2004; 28: 123–6
- Panotopoulos J, Hanslik-Schnabel B, Wanivenhaus A, Trieb K. Outcome of surgical concepts in haemophilic arthropathy of the hindfoot. Haemophilia 2005; 11: 468–71
- San Giovanni TP, Keblish DJ, Thomas WH, Wilson MG. Eight-year results of a minimally constrained total ankle arthroplasty. Foot Ankle Int 2006; 27: 418–26
- Stengel D, Bauwens K, Ekkernkamp A, Cramer J. Efficacy of total ankle replacement with meniscal-bearing devices: a systematic review and meta-analysis. Arch Orthop Trauma Surg 2005; 125: 109–19
- Su EP, Kahn B, Figgie MP. Total ankle replacement in patients with rheumatoid arthritis. Clin Orthop 2004, 424: 32–8
- Winson IG, Robinson DE, Allen PE. Arthroscopic ankle arthrodesis. J Bone Joint Surg (Br) 2005; 87: 343–7
- Wood PL, Deakin S. Total ankle replacement, the results in 200 ankles. J Bone Joint Surg (Br) 2003; 85: 334–41