Abstract
Background and purpose Many studies have suggested that navigation-based implantation can improve cup positioning in total hip arthroplasty (THA). We conducted a systematic review and meta-analysis to compile the best available evidence, and to overcome potential shortcomings because of small sample sizes in individual studies.
Methods The search strategy covered the major medical databases from January 1976 through August 2007, as well as various publishers' databases. The internal validity of individual studies was evaluated independently by 3 reviewers. We used random-effects modeling to obtain mean differences in cup angulation and relative risk (RR) of cup positioning outside Lewinnek's safe zone.
Results Of 363 citations originally identified, 5 trials of moderate methodology enrolling a total of 400 patients were included in the analysis. Mean cup inclination and anteversion were not statistically significantly different between the conventional groups and the navigated groups. Navigation reduced the variability in cup positioning and the risk of placing the acetabular component beyond the safe zone (RR = 0.21, CI: 0.13–0.32).
Interpretation Based on the current literature, navigation is a reliable tool to optimize cup placement, and to minimize outliers. However, long-term outcomes and cost utility analyses are needed before conclusive statements can be drawn about the value of routine navigation in THA.
The work flow in operating rooms worldwide has been markedly influenced by computer-assisted surgery (CAS) (Stindel et al. Citation2007). About 10 years after its introduction, many applications are available for orthopedic and trauma procedures (Jenny Citation2006, Holly and Foley Citation2007, Stindel et al. Citation2007). CAS has gained acceptance, especially for arthroplasty of the knee and hip (Amiot and Poulin Citation2004, Stindel et al. Citation2007, Bauwens et al. Citation2007). There are 3 types of imaging systems used to simultaneously generate different planes of the target object, all of which need intraoperative registration of anatomical landmarks (Sikorski and Chauhan Citation2003). Either CT-based, fluoroscopically-assisted, or imageless methods are used to simultaneously generate different planes of the therapeutic object to be treated (Grutzner et al. Citation2004, Widmer and Grutzner Citation2004, Ottersbach and Haaker Citation2005, Honl et al. Citation2006, Kalteis et al. Citation2006a).
Recent studies have shown that even experienced surgeons often fail to place the acetabular component within Lewinnek's “safe zone” (i.e. inclination of 40° ± 10°, anteversion of 15° ± 10°) (Lewinnek et al. Citation1978) when using a freehand technique (Saxler et al. Citation2004a, Tannast et al. Citation2005a, Honl et al. Citation2006, Kalteis et al. Citation2006a, Bosker et al. Citation2007, Leichtle et al. Citation2007).
On the other hand, preliminary results from laboratory studies, larger case series, and multicenter experience suggest that navigation-based implantation improves cup positioning in THA (Saxler et al. Citation2004b, Honl et al. Citation2006, Minoda et al. Citation2006, Kalteis et al. Citation2006a, Leichtle et al. Citation2007, Parratte and Argenson Citation2007, Sugano et al. Citation2007). However, conflicting statements and suspected methodological limitations in an arbitrary sample of the studies that we reviewed led us to conduct a systematic review of the international literature on navigated THA with emphasis on cup orientation.
We wanted to compile the current best evidence by pooling all RCT and quasi-RCT studies of comparisons between navigated and conventional cup positioning in THA, and to examine whether they support the assumption of better radiographic and clinical results with navigation.
Methods
We identified all investigations that (1) compared navigation-based THA and conventional THA with emphasis on cup implantation, regardless of the underlying condition, disease, or navigation system (ITT), and that (2) met a level of evidence of II or higher, according to the suggestions of the Oxford Center for Evidence-Based Medicine (i.e. prospective cohort study, low-quality RCT, quasi-RCT, and individual RCT). We made no restrictions about language.
Study designs representing a lower level of evidence, especially retrospective cohort studies, were excluded from the analysis. We reasoned that only experimental and quasi-experimental designs minimize the risk of confounding, and allow valid estimates of the efficacy of navigation.
Our search strategy covered all major medical databases (Medline, Embase, SciSearch, Cinahl, and the Cochrane Central Register of Trials) from January 1976 through August 2007.
We used the following medical subject headings, or their equivalents: ‘position*’, ‘orient*’, ‘inclin*’, ‘anteversion’, ‘dislocation’, ‘luxation’, ‘wear’, ‘loosening’, ‘computer assisted’, ‘computer based’, ‘imageless’, ‘image based’, ‘CT-based’, ‘navig*’, ‘CAOS’, ‘CAS’, each in combination with ‘hip’, ‘cup’, ‘arthroplasty’, ‘THA’ ‘prospective’, ‘meta’, ‘review’ and ‘random*’. We also scanned publishers’ databases and conducted manual searches in the Journal of Bone and Joint Surgery (American and British Volumes, including supplements), Clinical Orthopaedics and Related Research, Journal of Arthroplasty, and Acta Orthopaedica. The bibliographies of the papers identified were searched for additional relevant citations. Potentially eligible studies were selected by taking the title and abstract. If the title and the abstract were inadequate to reach a final decision, we obtained the full paper.
The internal validity of individual studies was evaluated independently by 3 reviewers (JB, CL, and DS). We assessed the following methodological issues: (1) Did the authors put forward a clear study hypothesis? (2) Did they perform a sample-size calculation? (3) Did they report their results according to the CONSORT statement (including an illustration of the flow)? (4) did they respect the intention-to-treat principle (e.g. were patients who had been assigned to navigated THA still analyzed as navigated if the system had failed? (5) Did they provide sufficient numerical information in order to be able to recalculate the results reported?
To test the hypothesis that cup placement in THA is more precise with navigation (compared to the conventional technique), we focused on the inclination and anteversion of the cup as target criteria. We also used criteria according to Lewinnek's ‘safe zone’ to investigate this hypothesis.
Statistics
We abstracted and tabulated baseline details of patients enrolled in individual studies, where available (e.g. age, sex, underlying condition). Weighted means and weighted mean differences in inclination and anteversion between navigated and conventional cup placement were calculated with their 95% confidence intervals (CIs). We also computed the risk ratio (RR) of cup placement outside Lewinnek's ‘safe zone’. Heterogeneity was assessed with chi-square statistics. A p-value of < 0.1 was considered suggestive of statistical heterogeneity, prompting random effects modeling.
We attempted to measure publication bias—that is, a lack of small studies without significant results—by the linear regression test for funnel plot asymmetry described by Egger et al. (Citation1997). However, because of the small sample of eligible studies, this was meaningless. Also, the sample size prohibited random-effects meta-regression to adjust common effect estimates for potential confounders.
All analyses were performed in an exploratory fashion. We used the STATA statistical software package version 10.0 (StataCorp, College Station, TX) for all analyses.
Results
Search results
Our search strategy revealed 363 citations, 326 of which were excluded after scanning the title and the abstract. 37 clinical reports were considered potentially eligible for this meta-analysis and were retrieved as full text. The study flow according to the QUOROM (Quality of Reporting Meta-Analyses) is depicted in . Identified and excluded studies are listed in and (See Appendix).
Figure 1. Study selection process according to QUOROM (Quality of Reporting of Meta-Analyses) standards.
Table 1. Demographic baseline data
Table 2. Studies included in the meta-analysis, with details of methodology
The selection procedure left 5 eligible studies involving 400 enrolled patients (198 men, 202 women) with a mean age of 61 (SD 25) years. Of these, 2 studies were published in English, 2 in German, and 1 was published in the Czech language. 4 studies specified the underlying etiology of the osteoarthritis (OA), with 261/300 replacements (87%) performed because of primary OA. Patient samples were well balanced with regard to the basic demographic items available ().
One trial (Parratte and Argenson Citation2007) was published twice, in French and English. We included only the English paper. The authors’ line, IRB reference number, recruitment period, and number of subjects noted in another paper was suggestive of continued work (Kalteis et al. Citation2005, Kalteis et al. Citation2006a). We only included the most recent study in our analysis, which was a three-arm trial (CT-based navigation versus imageless-navigation versus conventional cup positioning). Since both navigation methods showed similar trends compared to conventional surgery—proportion of cups outside the safe zone: CT-based 5/30 (0.2, CI: 0.1–0.4), imageless 2/30 (0.1, CI: 0.1 – 0.2), freehand 16/30 [0.5, CI: 0.3–0.7)—results of the computer-assisted procedures were merged to facilitate analysis and to increase power.
Altogether, the methodological quality was moderate (). 1 trial indexed as RCT was, in fact, a matched-pair analysis in which “the first patient was randomly chosen and then one patient was selected out of every eight patients on a list of all patients meeting the inclusion criteria who were candidates for a THA. The patients assigned to the freehand cup placement group were matched for gender, age within five years, pathological condition, operatively treated side, and body-mass index within 3 points.” (Leenders et al. Citation2002). They mixed a cohort design with an RCT. The authors reported on 50 patients undergoing THA at their department prior to the establishment of a navigation system. Another 100 patients were randomly allocated to either CAS or conventional surgery. Of note, while the precision in cup positioning improved over time, there was no difference between navigated and freehand cup placement in the RCT part of the study. We only included the results from randomly assigned patients. The reasoning for the target sample size was reported in a single paper (Kalteis et al. Citation2006a). None fulfilled the ITT principle or represented a consort flow diagram. Studies provided no detailed information on complication rates, length of hospital stay, functional scoring, and other clinically relevant outcomes, or on costs or cost utility.
Treatment results
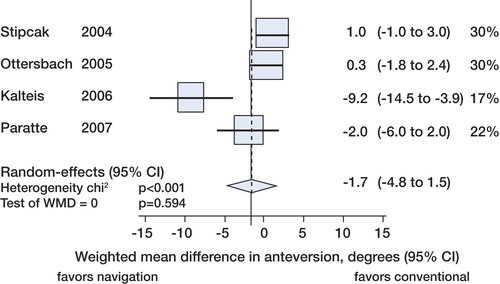
Cup inclination averaged 44° (CI: 40 – 48) in the conventional arm and 43° (CI: 40 – 46) in the navigation arm. The weighted mean difference in inclination between conventional and computer-assisted positioning was not statistically significant (–0.89°, CI: -4.2–2.4) (). Means from Leenders' trial had to be derived from a histogram. When excluding this trial from random-effects pooling, the mean difference between groups was –0.30° (CI: -0.83–0.22). Cup anteversion averaged 17° (CI: 11–22) in the conventional arm and 15° (CI: 11–18) in the navigation arm. Again, this difference was compatible with chance ().
Figure 2. Forest plot showing that there was no statistically significant difference in mean inclination of cups placed with and without navigational support. Mean effect sizes of individual studies are expressed as squares, with larger squares denoting larger sample sizes, higher precision, and higher relative weight within the meta-analysis. Values lower than zero favor navigation and values higher than zero favor conventional cup positioning. The diamond shows the pooled overall effect size with the 95% confidence interval. When the 95% confidence interval includes the zero, it can be assumed that there is no statistical significance at the two-tailed p < 0.05 level.
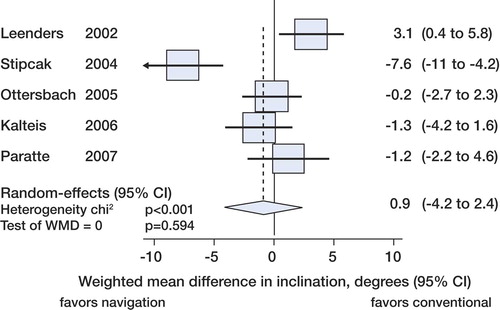
Figure 3. Forest plot showing that there was no statistically significant difference in mean anteversion of cups placed with and without navigational support. No information on anteversion was available in the trial by Leenders et al. (Leenders et al. Citation2002).
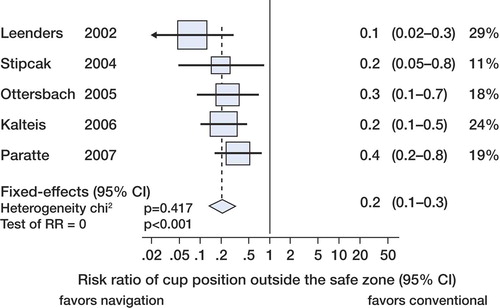
Overall, navigation reduced the variability in cup positioning statistically significantly, and reduced the risk of placing the acetabular component beyond the safe zone (). The pooled RR of 0.21 (CI: 0.13–0.32) translates to a risk difference of 37% (CI: 45–29) in favor of navigation.
Discussion
Correct cup positioning is crucial for the short- and long-term success of THA. Many studies have suggested that there is improved cup positioning with navigation-based implantation (Saxler et al. Citation2004a, Honl et al. Citation2006, Kalteis et al. Citation2006a, Leichtle et al. Citation2007, Parratte and Argenson Citation2007). However, individual studies are too small to allow conclusive statements on the potential benefit of navigation in THA.
Our meta-analysis demonstrates a clear advantage of navigated cup orientation over conventional freehand cup orientation in THA. As discussed later, however, various severe pitfalls and possible inherent error or bias must be considered. As with total knee arthroplasty and screw positioning in spinal surgery, the major benefit of navigation is the reduction of outliers, that is, cup positioning beyond the “safe zone” with an inclination of 40° (± 10°) and anteversion of 15° (± 10°) (Saxler et al. Citation2004a, Honl et al. Citation2006, Kalteis et al. Citation2006a, Minoda et al. Citation2006, Leichtle et al. Citation2007, Parratte and Argenson Citation2007, Sugano et al. Citation2007). Moreover, it seems that navigation-based cup positioning in THA meets the criteria of evidence by reducing the amount of outliers in cup orientation (Leenders et al. Citation2002, Stipcak et al. Citation2004, Ottersbach and Haaker Citation2005, Kalteis et al. Citation2006a, Parratte and Argenson Citation2007).
The findings from experimental and quasi-experimental investigations are supported by those from observational studies that were excluded from the present meta-analysis. Sugano et al. (Citation2007) found none of 59 navigated cups as compared to 31 of 111 conventional implanted cups to be outside the “safe zone” (p < 0.001). There was no significant difference in mean inclination, but a significantly greater mean anteversion with conventional cup placement (p < 0.001). In a multicenter study, a significantly higher variability in both inclination and anteversion (p < 0.001) was found after conventional cup implantation (Saxler et al. Citation2004a).
In a minimally invasive THA study, significant variances in both inclination (p < 0.01) and anteversion (p < 0.03) were reported (Wixson and MacDonald Citation2005). In retrospective studies, a statistically significant difference in variation for both inclination and anteversion has been found (Haaker et al. Citation2007), and also an advantage in navigation-based cup placement in dysplastic hips (Haaker et al. Citation2003).
The reduction of outliers is of clinical relevance, as malpositioning of the acetabular component may cause impingement and restrict the range of motion. It is a known risk factor for dislocation and can lead to increased and premature wear, with elevated metal-ion concentrations in serum and an overall increased risk of loosening and revision (Patil et al. Citation2003, Brodner et al. Citation2004, Nishii et al. Citation2004).
The proven advantages of navigation must be traded off against the argument of prolonged surgery and higher costs (Eingartner Citation2007).
The number of studies, patients, and outcome data is still limited, and we also noted some weaknesses in trial methodology, which highlights various pitfalls and possible inherent error or bias that warrant further discussion. First, there was no clear evidence of publication error, and it is likely that the published information reflects the best results currently achievable with navigated cup positioning in THA. Future trials must adhere to methodological standards such as proper random assignment and intention-to-treat analyses, and aim for a thorough comparison of radiographic and functional results, complication and survival rates, quality of life, and also extra costs and cost utility.
Secondly, one uncertainty and limitation of evidence is the status of current discussion about the correct incorporation of the pelvic anatomy (Beckmann et al. Citation2008) regarding the generation of landmarks as a basis for imageless navigation (Lembeck et al. Citation2005, Richolt et al. Citation2005, Stiehl et al. Citation2005, Wolf et al. Citation2005, Mayr et al. Citation2006, Spencer et al. Citation2006, Beckmann et al. Citation2008) and the correct radiological assessment of the implant position (Olivecrona et al. Citation2004, Blendea et al. Citation2005, Tannast et al. Citation2005b, Jaramaz and Eckman Citation2006, Kalteis et al. Citation2006b, Liaw et al. Citation2006, Marx et al. Citation2006, Muller et al. Citation2006, Penney et al. Citation2007, Beckmann et al. Citation2008).
Thirdly, apart from cup orientation, outcomes such as longevity, range of motion, impingement, and dislocation further depend on the head-neck ratio, the offset, and the stem orientation (D'Lima et al. Citation2000, Widmer and Zurfluh Citation2004, Pedersen et al. Citation2005, Widmer and Majewski Citation2005, Masaoka et al. Citation2006, Yoshimine Citation2006, Malik et al. Citation2007, Widmer Citation2007). In addition, the surgical approach and endogenous factors such as comorbidity and muscular status may contribute to the fate of the hip joint (Soong et al. Citation2004, Zwartele et al. Citation2004, Meek et al. Citation2006).
Lastly, although we took care not to miss any relevant publication, we did not ask the authors for individual patient data or ongoing studies. Occasionally, editing of manuscripts and limited space in scientific journals may obscure some methodological features originally respected by study protocols.
In conclusion, based on the current literature, navigation is a reliable tool for optimization of cup placement in THA. Navigation reduces the incidence of outliers beyond the so-called desired “safe zone”. Long-term outcomes have to be awaited before making final statements about longevity of the prosthesis and patient satisfaction, which depend on factors other than just cup orientation. A corresponding cost utility analysis must also be done.
Acknowledgements
JB and CL initiated the study and contributed to all parts of the manuscript. DS, MT, and JüG did the statistical analyses and proofreading. JoG supervised the study as head of the department.
No competing interests declared.
- Amiot LP, Poulin F.. Computed tomography-based navigation for hip, knee, and spine surgery.. Clin Orthop 2004; (421): 77–86.
- Bauwens K, Matthes G, Wich M, Gebhard F, Hanson B, Ekkernkamp A, Stengel D.. Navigated total knee replacement. A meta-analysis.. J Bone Joint Surg (Am) 2007; 89: 261–9.
- Beckmann J, Luring C, Tingart M, Anders S, Grifka J, Kock FX.. Cup positioning in THA: current status and pitfalls. A systematic evaluation of the literature.. Arch Orthop Trauma Surg 2008; 129: 863–72.
- Bernsmann K, Langlotz U, Ansari B, Wiese M.. Computer-assisted navigated cup placement of different cup types in hip arthroplasty—a randomised controlled trial.. Z Orthop Ihre Grenzgeb 2001; 139: 512–7.
- Blendea S, Eckman K, Jaramaz B, Levison TJ, Digioia AMIII. Measurements of acetabular cup position and pelvic spatial orientation after total hip arthroplasty using computed tomography/radiography matching.. Comput Aided Surg 2005; 10: 37–43.
- Bosker BH, Verheyen CC, Horstmann WG, Tulp NJ.. Poor accuracy of freehand cup positioning during total hip arthroplasty.. Arch Orthop Trauma Surg 2007; 127: 375–9.
- Brodner W, Grubl A, Jankovsky R, Meisinger V, Lehr S, Gottsauner-Wolf F.. Cup inclination and serum concentration of cobalt and chromium after metal-on-metal total hip arthroplasty.. J Arthroplasty 2004; 19: 66–70.
- D'Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CWJr. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios.. J Bone Joint Surg (Am) 2000; 82: 315–21.
- Egger M, Davey SG, Schneider M, Minder C.. Bias in meta-analysis detected by a simple.. graphical test. BMJ 1997; 315: 629–34.
- Eingartner C.. Current trends in total hip arthroplasty.. Ortop Traumatol Rehabil 2007; 9: 8–14.
- Grutzner PA, Zheng G, Langlotz U, von RJ, Nolte LP, Wentzensen A, Widmer KH, Wendl K. C-arm based navigation in total hip arthroplasty-background and clinical experience.. Injury (Suppl 1) 2004; 35: S-5.
- Haaker R, Tiedjen K, Rubenthaler F, Stockheim M.. [Computer-assisted navigated cup placement in primary and secondary dysplastic hips].. Z Orthop Ihre Grenzgeb 2003; 141: 105–11.
- Haaker RG, Tiedjen K, Ottersbach A, Rubenthaler F, Stockheim M, Stiehl JB.. Comparison of conventional versus computer-navigated acetabular component insertion.. J Arthroplasty 2007; 2: 151–9.
- Holly LT, Foley KT.. Image guidance in spine surgery.. Orthop Clin North Am 2007; 38: 451–61.
- Honl M, Schwieger K, Salineros M, Jacobs J, Morlock M, Wimmer M.. Orientation of the acetabular component. A comparison of five navigation systems with conventional surgical technique.. J Bone Joint Surg (Br) 2006; 88: 1401–5.
- Jaramaz B, Eckman K.. 2D/3D registration for measurement of implant alignment after total hip replacement.. Med Image Comput Comput Assist Interv Int Conf Med Image Comput Comput Assist Interv 2006; 9: 653–61.
- Jenny JY.. The history and development of computer assisted orthopaedic surgery.. Orthopade 2006; 35: 1038–42.
- Kalteis T, Handel M, Herold T, Perlick L, Baethis H, Grifka J.. Greater accuracy in positioning of the acetabular cup by using an image-free navigation system.. Int Orthop 2005; 29: 272–6.
- Kalteis T, Handel M, Bathis H, Perlick L, Tingart M, Grifka J.. 2006a; Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation?. J Bone Joint Surg (Br) 88: 163–7.
- Kalteis T, Handel M, Herold T, Perlick L, Paetzel C, Grifka J.. 2006b; Position of the acetabular cup—accuracy of radiographic calculation compared to CT-based measurement.. Eur J Radiol 58: 294–300.
- Leenders T, Vandevelde D, Mahieu G, Nuyts R.. Reduction in variability of acetabular cup abduction using computer assisted surgery: a prospective and randomized study.. Comput Aided Surg 2002; 7: 99–106.
- Leichtle U, Gosselke N, Wirth CJ, Rudert M.. Radiologic evaluation of cup placement variation in conventional total hip arthroplasty.. Rofo 2007; 179: 46–52.
- Lembeck B, Mueller O, Reize P, Wuelker N.. Pelvic tilt makes acetabular cup navigation inaccurate.. Acta Orthop 2005; 76: 517–23.
- Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR.. Dislocations after total hip-replacement arthroplasties.. J Bone Joint Surg (Am) 1978; 60: 217–20.
- Liaw CK, Hou SM, Yang RS, Wu TY, Fuh CS.. A new tool for measuring cup orientation in total hip arthroplasties from plain radiographs.. Clin Orthop 2006; (451): 134–9.
- Malik A, Maheshwari A, Dorr LD.. Impingement with total hip replacement.. J Bone Joint Surg (Am) 2007; 89: 1832–42.
- Marx A, von KM, Pfortner J, Wiese M, Saxler G.. Misinterpretation of cup anteversion in total hip arthroplasty using planar radiography.. Arch Orthop Trauma Surg 2006; 126: 487–92.
- Masaoka T, Yamamoto K, Shishido T, Katori Y, Mizoue T, Shirasu H, Nunoda D.. Study of hip joint dislocation after total hip arthroplasty.. Int Orthop 2006; 30: 26–30.
- Mayr E, de la Barrera JL, Eller G, Bach C, Nogler M.. The effect of fixation and location on the stability of the markers in navigated total hip arthroplasty: a cadaver study.. J Bone Joint Surg (Br) 2006; 88: 168–72.
- Meek RM, Allan DB, McPhillips G, Kerr L, Howie CR.. Epidemiology of dislocation after total hip arthroplasty.. Clin Orthop 2006; (447): 9–18.
- Minoda Y, Kadowaki T, Kim M.. Acetabular component orientation in 834 total hip arthroplasties using a manual technique.. Clin Orthop 2006; (445): 186–91.
- Muller O, Reize P, Trappmann D, Wulker N.. Measuring anatomical acetabular cup orientation with a new X-ray technique.. Comput Aided Surg 2006; 11: 69–75.
- Murray DW.. The definition and measurement of acetabular orientation.. J Bone Joint Surg (Br) 1993; 75: 228–32.
- Nishii T, Sugano N, Miki H, Koyama T, Takao M, Yoshikawa H.. Influence of component positions on dislocation: computed tomographic evaluations in a consecutive series of total hip arthroplasty.. J Arthroplasty 2004; 19: 162–6.
- Olivecrona H, Weidenhielm L, Olivecrona L, Beckman MO, Stark A, Noz ME, Maguire GQJr, Zeleznik MP, Svensson L, Jonson T.. A new CT method for measuring cup orientation after total hip arthroplasty: a study of 10 patients.. Acta Orthop Scand 2004; 75: 252–60.
- Ottersbach A, Haaker R.. Optimization of cup positioning in THA–comparison between conventional mechanical instrumentation and computer-assisted implanted cups by using the orthopilot navigation system.. Z Orthop Ihre Grenzgeb 2005; 143: 611–5.
- Parratte S, Argenson JN.. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty. A prospective, randomized, controlled study.. J Bone Joint Surg (Am) 2007; 89: 494–9.
- Patil S, Bergula A, Chen PC, Colwell CWJr, D'Lima DD.. Polyethylene wear and acetabular component orientation.. J Bone Joint Surg (Am) (Suppl 4) 2003; 85: 56–63.
- Pedersen DR, Callaghan JJ, Brown TD.. Activity-dependence of the “safe zone” for impingement versus dislocation avoidance.. Med Eng Phys 2005; 27: 323–8.
- Penney GP, Edwards PJ, Hipwell JH, Slomczykowski M, Revie I, Hawkes DJ.. Postoperative calculation of acetabular cup position using 2-D-3-D registration.. IEEE Trans Biomed Eng 2007; 54: 1342–8.
- Pradhan R.. Planar anteversion of the acetabular cup as determined from plain anteroposterior radiographs.. J Bone Joint Surg Br 1999; (81): 431–435.
- Richolt JA, Effenberger H, Rittmeister ME.. How does soft tissue distribution affect anteversion accuracy of the palpation procedure in image-free acetabular cup navigation? An ultrasonographic assessment.. Comput Aided Surg 2005; 10: 87–92.
- Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grutzner PA, Steffen R, von KM, Holland-Letz T, Bernsmann K.. 2004a; [Cup placement in hip replacement surgery–A comparison of free-hand and computer assisted cup placement in total hip arthroplasty –a multi-center study.. Z Orthop Ihre Grenzgeb 142: 286–91.
- Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grutzner PA, Steffen R, von KM, Holland-Letz T, Bernsmann K.. 2004b; The accuracy of free-hand cup positioning–a CT based measurement of cup placement in 105 total hip arthroplasties.. Int Orthop 28: 198–201.
- Sikorski JM, Chauhan S.. Computer-assisted orthopaedic surgery: do we need CAOS?. J Bone Joint Surg (Br) 2003; 85: 319–23.
- Soong M, Rubash HE, Macaulay W.. Dislocation after total hip arthroplasty.. J Am Acad Orthop Surg 2004; 12: 314–21.
- Spencer JM, Day RE, Sloan KE, Beaver RJ.. Computer navigation of the acetabular component: a cadaver reliability study.. J Bone Joint Surg (Br) 2006; 88: 972–5.
- Stiehl JB, Heck DA, Lazzeri M.. Accuracy of acetabular component positioning with a fluoroscopically referenced CAOS system.. Comput Aided Surg 2005; 10: 321–7.
- Stindel E, Merloz P, Graf P, Massin P, Gruber P, Robert H, Moineau G, Colmar M.. Computer assisted orthopedics surgery.. Rev Chir Orthop Reparatrice Appar Mot 2007; 93: 2S11–2S32.
- Stipcak V, Stoklas J, Hart R, Janecek M.. Implantation of a non-cemented acetabulum with the use of a navigation system.. Acta Chir Orthop Traumatol Cech 2004; 71: 288–91.
- Sugano N, Nishii T, Miki H, Yoshikawa H, Sato Y, Tamura S.. Mid-term results of cementless total hip replacement using a ceramic-on-ceramic bearing with and without computer navigation.. J Bone Joint Surg (Br) 2007; 89: 455–60.
- Tannast M, Langlotz F, Kubiak-Langer M, Langlotz U, Siebenrock KA.. 2005a; Accuracy and potential pitfalls of fluoroscopy-guided acetabular cup placement.. Comput Aided Surg 10: 329–36.
- Tannast M, Langlotz U, Siebenrock KA, Wiese M, Bernsmann K, Langlotz F.. 2005b; Anatomic referencing of cup orientation in total hip arthroplasty.. Clin Orthop (436): 144–50.
- Widmer KH.. A simplified method to determine acetabular cup anteversion from plain radiographs.. J Arthroplasty 2004; 19: 387–90.
- Widmer KH.. Containment versus impingement: finding a compromise for cup placement in total hip arthroplasty.. Int Orthop (Suppl 1) 2007; 31: S29–S33.
- Widmer KH, Grutzner PA.. Joint replacement-total hip replacement with CT-based navigation.. Injury (Suppl 1) 2004; 35: S-9.
- Widmer KH, Majewski M.. The impact of the CCD-angle on range of motion and cup positioning in total hip arthroplasty.. Clin Biomech (Bristol, Avon) 2005; 20: 723–8.
- Widmer KH, Zurfluh B.. Compliant positioning of total hip components for optimal range of motion.. J Orthop Res 2004; 22: 815–21.
- Wixson RL, MacDonald MA.. Total hip arthroplasty through a minimal posterior approach using imageless computer-assisted hip navigation.. J Arthroplasty 2005; 20: 51–6.
- Wolf A, Digioia AMIII, Mor AB, Jaramaz B.. Cup alignment error model for total hip arthroplasty.. Clin Orthop 2005; (437): 132–7.
- Yoshimine F.. The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements.. J Biomech 2006; 39: 1315–23.
- Zwartele RE, Brand R, Doets HC.. Increased risk of dislocation after primary total hip arthroplasty in inflammatory arthritis: a prospective observational study of 410 hips.. Acta Orthop Scand 2004; 75: 684–90.
APPENDIX
Table 3. Excluded studies