Abstract
Background The acetabular component has remained the weakest link in hip arthroplasty regarding achievement of long-term survival. Primary fixation is a prerequisite for long-term performance. For this reason, we investigated the stability of a unique cementless titanium-coated elastic monoblock socket and the influence of supplementary screw fixation.
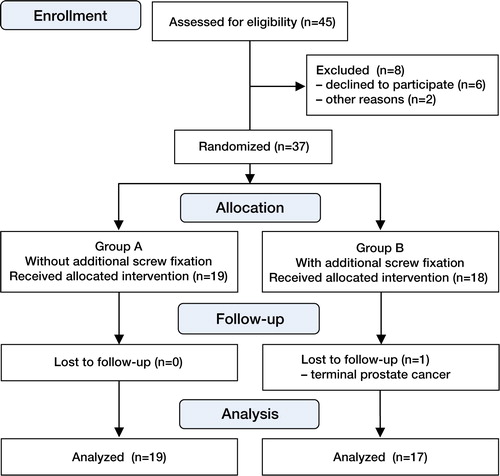
Patient and methods During 2006–2008, we performed a randomized controlled trial on 37 patients (mean age 63 years (SD 7), 22 females) in whom we implanted a cementless press-fit socket. The socket was implanted with additional screw fixation (group A, n = 19) and without additional screw fixation (group B, n = 18). Using radiostereometric analysis with a 2-year follow-up, we determined the stability of the socket. Clinically relevant migration was defined as > 1 mm translation and > 2º rotation. Clinical scores were determined.
Results The sockets without screw fixation showed a statistically significantly higher proximal translation compared to the socket with additional screw fixation. However, this higher migration was below the clinically relevant threshold. The numbers of migratory sockets were not significantly different between groups. After the 2-year follow-up, there were no clinically relevant differences between groups A and B regarding the clinical scores. 1 patient dropped out of the study. In the others, no sockets were revised.
Interpretation We found that additional screw fixation is not necessary to achieve stability of the cementless press-fit elastic RM socket. We saw no postoperative benefit or clinical effect of additional screw fixation.
During the last 5 years, several long-term reports on different methods to achieve primary stability in cementless sockets have shown excellent survival using aseptic loosening as the endpoint (Kim Citation2005, Kim et al. Citation2005, Firestone et al. Citation2007, Suckel et al. Citation2009, Pakvis et al. Citation2011).
During the last 2 decades, we have used the cementless RM classic socket with good to excellent long-term results (Diks et al. Citation2005, Pakvis et al. Citation2011). Ihle et al. (Citation2008) also reported good long-term results for this cementless, titanium particle-coated socket. This socket is based on the philosophy that an elastic polyethylene RM socket (approx 1,000 N/mm2), in contrast to a titanium-calcium phosphate rigid metal shell (approx 105,000 N/mm2), provides the elastic properties of acetabular bone (approx 500–6,000 N/mm2). The resulting physiological distribution of articular forces protects the acetabular bone and provides optimal conditions for ingrowth, with subsequent long-term component fixation. Due to stress shielding, rigid sockets may reduce the acetabular bone quality (Wright et al. Citation2001, Huo and Osier Citation2008). In comparison to femoral stress shielding, acetabular stress shielding results in osteolysis and component migration requiring revision surgery.
The primary stability of the RM classic socket is achieved by 2 pegs and additional screw fixation; secondary stability is achieved from biological ingrowth into the titanium-particle coating. At our specialized orthopedic training hospital, we have encountered implantation difficulties, leading to a learning curve for optimal positioning of the pegs. In a primary series, this resulted in malpositioning of the socket and a high rate of early to short-term revisions (Diks et al. Citation2005). The new design of the peg-less, titanium particle-coated RM press-fit cup is expected to make it easier to implant ().
The effect of adding screws to a press-fit socket to optimize primary stability has been unclear. Some authors have seen no additional effect (Onsten et al. Citation1996, Thanner et al. Citation2000, Rohrl et al. Citation2006, Roth et al. Citation2006, Iorio et al. Citation2010), while other authors have described an extra stabilizing effect of the screws on the primary stability of press-fit sockets (Hadjari et al. Citation1994, Thanner et al. Citation1996). When additional screw fixation is used, some potentially negative effects on long-term survival must be accepted. The development of osteolytic lesions is believed to be the result of the transmission of articular pressure and of wear particles to the acetabular bone via the screw channels (Schmalzried et al. Citation1997).
To our knowledge, only Thanner et al. (Citation2000) have performed a radiostereometric analysis-based (RSA) randomized controlled trial (RCT); they found no effect of the additional screw fixation in a rigid metal-backed modular titanium-mesh HA- (hydroxyapatite-) coated socket.
We performed an RCT to evaluate the stability of the cementless, RM press-fit socket with and without additional screw fixation. We used RSA to determine the stability in each group. We hypothesized that there would be a difference in stability between the cementless RM press-fit sockets with additional screw fixation and those without: that due to the elastic modulus of the RM press-fit socket without additional screw fixation, there would be a larger degree of migration shortly after surgery but that it would stabilize during the two-year follow-up.
Patients and methods
This study was performed in compliance with the declaration of Helsinki for medical research involving human subjects. It was a single-center, equally randomized, parallel-grouped study, conducted between 2006 and 2008 at the Sint Maartenskliniek, Nijmegen. It was approved by the local ethics committee (reg. no 2006032). Patients were followed for 2 years. Randomization was done prior to the start of the trial using computer-generated random patient allocation in blocks of four for each participating surgeon (Block Stratified Randomization version 4.4, 1997; S. Piantadosi, Baltimore, Maryland). Only after the implantation of the socket were the participating surgeons informed of the allocated treatment by opening a closed envelope. The inclusion criteria were unilateral primary osteoarthritis, BMI < 30, age between 18 and 70 years, and written informed consent. Patients who were pregnant and those who had secondary osteoarthritis were excluded from the study.
Surgical technique
All hips were implanted by the senior authors (GvH, MS). Preoperative third-generation cephalosporins were given to all patients. All arthroplasties were performed using a posterolateral approach in a clear-air operating theater with laminar flow. Reaming of the acetabulum was undersized by 1.6 mm to achieve adequate press-fit. The RM press-fit socket (Mathys AG, Bettlach, Switzerland) is an all-polyethylene socket with a titanium-particle coating. The socket has a hemispherical monoblock design with a flatted pole and is made from nitrogen-radiated sterilized UHMW (ISO 5834-1+2) polyethylene.
For additional fixation (when performed), two 4.0-mm screws of variable length were placed through 2 of the four screw openings situated in the rims of the sockets. A cementless, grit-blasted, titanium-alloy (Ti6Al4V ISO 5832-3) CLS Spotorno femoral stem (Zimmer, Warsaw, IN) was used in all cases. In all patients, a 32-mm ceramic (Al2O3) head on polyethylene articulation was used.
All patients were mobilized on the first postoperative day and direct full weight bearing was allowed using crutches during the postoperative rehabilitation period, which was supervised by a physiotherapist. All patients received nadoparine for 6 weeks as thromboprofylaxis.
RSA
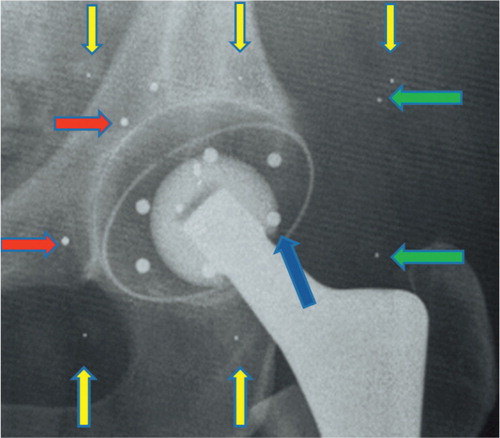
Six 1.2-mm tantalum markers were inserted preoperatively into pre-existing openings in the polyethylene rim of the RM press-fit socket using a specially developed insertion system (Mathys AG) (). During the operation, markers of 0.8 mm in diameter were inserted into the acetabular bone after the acetabulum had been reamed to the required diameter. At least 6 markers were inserted using an insertion gun, at a depth of 10 mm in all regions of the acetabular bone, resulting in scattered positions to fulfill the conditions for accurate RSA measurements (Mathys AG). During the first postoperative week, baseline digital RSA radiographs (Agfa-Gevaert AG, Rijswijk, the Netherlands) were taken (). Follow-up images were taken during the outpatient clinic visit at 2, 6, 12, and 24 months. A calibration cage (Medis, Leiden, the Netherlands) was placed beneath the patient as described by Selvik (Citation1990). All RSA radiographs (165 dpi and 11-bit gray scale resolution) were analyzed by using RSA-CMS software (version 4.3; Medis). Upper limits for errors were set to maintain the quality of RSA measurements; for transformation errors at 0.2, for focus errors at 2.0, and for the crossing errors of 2 connected markers at 0.15. For the rigid body errors, the limit was set at 0.5; however, most of the time the error was below 0.3 for both the cup and the bone. Unstable markers (with > 0.3 mm change in distance in consecutive radiographs) were excluded from analysis by the software. Finally, we double-checked measurements in which migration was apparent, to be sure that this was not caused by a measurement error.
Figure 2. The RM press-fit socket with 6 tantalum markers (1.2 mm) inserted into pre-existing openings in the polyethylene rim of the RM press-fit socket.
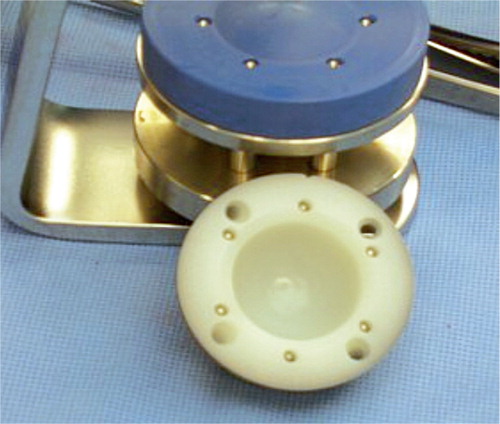
Figure 3. Pelvic radiograph showing the tantalum acetabular and socket markers after implantation of the cementless RM press-fit socket without any additional screw fixation. Yellow arrows: fiducial cage markers; green arrows: control cage markers; red arrows: acetabular bone markers; blue arrow: socket marker.
Migration was defined as micromotion of the center of gravity of the RM cup relative to the acetabular bone in the 3 translational and 3 rotational directions (Vrooman et al. Citation1998, Valstar et al. Citation2005). The precision of the RSA analysis was assessed using double examinations in all patients at the 2-month follow-up; the second set was done after complete repositioning of the patient and equipment. The differences in migration between the double radiographs, 30 for translational directions and 29 for rotational directions, were used to calculate the migration detection limits by the Bland-Altman method (). Migration was calculated between the postoperative baseline moment and each follow-up moment at 2, 6, 12, and 24 months.
Table 1. The detection limits of the RSA method (precision), based on the analysis of double examinations at 2 months and calculated using the Bland-Altman method
Clinical outcome
The Harris hip score (HHS) and the Oxford hip score were determined preoperatively and at each follow-up. All adverse events and complications were recorded and analyzed, to monitor the safety of the technique used.
Statistics
An a priori calculation with a significance level of 0.05, 90% power, and standard deviations of 0.4 mm (translation) and 0.9° (rotation) (Röhrl et al. Citation2004) indicated that 17 individuals per group would be needed to detect a significant migration difference of 0.4 mm or 0.9° between the groups. At each follow-up, mean migration for the 3 translations and the 3 rotations was determined, together with the SD and minima and maxima.
To test our hypothesis, we needed to compare the migration patterns of the 2 groups. However, because of the multiple primary endpoints (3 translations and 3 rotations to describe a 3-dimensional migration measured at 4 follow-up moments) and the small sample size, we could not construct a mathematical model. Therefore, we used a repeated-measures ANOVA (analysis of variance) for each individual translation and rotation parameter, with time as the within-subject factor and with/without screws as between-subjects factor. Post hoc, Scheffe’s test was used to identify follow-up moments in which the migration pattern was different between the groups.
Since, to our knowledge, no clinically relevant migration values for uncemented cups are available in the literature, we arbitrarily defined a translation of > 1 mm and/or a rotation of > 2º as being clinically relevant. The numbers of sockets with migration above those thresholds were counted for each group and a chi-square test was used to determine whether there was a statistically significant difference between the groups.
To compare the preoperative and the postoperative (2-year) clinical scores between the groups, the clinical scores were evaluated using the Mann-Whitney U test.
Statistical analyses were performed using SPSS and p-values of < 0.05 were considered to be statistically significant.
Results
45 patients were assessed for eligibility in this prospective study. 6 patients declined to participate. During the preparation for surgery, the sets used to place the tantalum markers were not available for 2 patients and these patients could not be enrolled. The remaining 37 enrolled patients (mean age 63 years (SD 7), 22 women) were not informed about the allocation result (). Group A consisted of 19 patients (11 women) treated without the additional screw stabilization. In group B, the 18 patients (11 women) received additional screw fixation ().
Table 2. Study demographics
Radiostereometric analysis
The repeated-measures ANOVA revealed statistically significantly more proximal-distal translation for the group without additional screw fixation (p = 0.04) (). Although this effect was consistent at all follow-up evaluations, the mean translation remained well below the defined clinically relevant migration threshold of 1 mm (). No other statistically significant differences in fixation could be found for the medial–lateral and anterior–posterior translations or for the 3 rotation parameters.
Figure 5. Migration patterns (translation or rotation) of the sockets with and without additional screws. Light gray: no additional screws; medium gray: with additional screws.
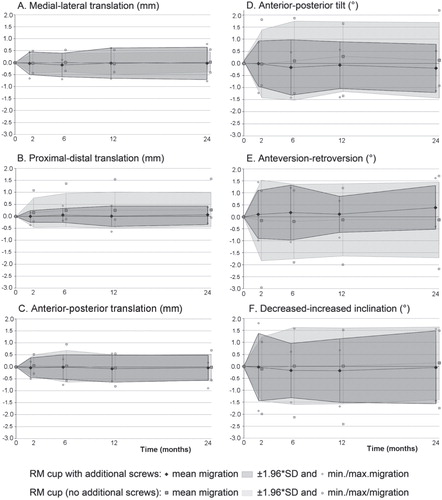
Table 3. RSA measurements: translations and rotations at the 2-year follow-up. Values are mean (95% CI)
At the 2-month and the 24-month follow-up, the numbers of sockets migrating more than the predetermined clinically relevant threshold was not significantly different between the groups (p = 0.2 for both follow-up occasions). In group B (with screws), zero sockets showed migration values greater than the thresholds that were considered clinically relevant. The 2 sockets from group A (without additional screw fixation) which showed migration above the predetermined clinically relevant threshold at 2 months had stabilized by the later follow-up assessments. At 2 years, 2 other sockets from group A showed migration that exceeded the clinically relevant values: 1 socket showed a proximal translation of slightly more than 1 mm and a second socket showed a retroversion of 2.2° (Figure 5).
Clinical results
The preoperative Harris hip score and the Oxford hip score were not significantly different between the 2 groups (). At 2 years, there was no statistically significant difference between the groups in either clinical score (p = 0.05 for HHS and p = 0.4 for Oxford score).
Table 4. Clinical scores (Harris hip score and Oxford hip score). Values are median (range)
Adverse events
None of the implanted sockets were revised. 1 patient (with the additional screw fixation) dropped out of the study due to terminal prostate cancer; the radiographic and clinical assessments at 1 year showed no complications. 2 femoral revisions due to dislocations were performed. Both showed no clinically relevant socket migration at the 2-year follow-up, although the patient with the periprosthetic fracture had persistent thigh pain, leading to a poor clinical result.
1 patient underwent an additional operation due to a deep infection treated within 6 weeks of the primary operation with lavage and appropriate culture-guided antibiotics. At the 2-year follow-up, migration analysis showed a stable socket; the clinical scores were excellent. Another patient sustained a neuropraxia of the sciatic nerve due to a postoperative hematoma. A surgical evacuation of the hematoma resulted in full remission of the clinical symptoms. At the last follow-up, both RSA and clinical scores showed excellent results. 2 other patients complained of mild thigh pain without socket migration or scintigrafic signs of complications.
Discussion
We found a statistically significant but clinically non-relevant higher proximal migration in the RM press-fit sockets without additional screw fixation. This proximal translation was detected during the settling phase of the press-fit socket at the 2-month follow-up, after which no additional statistically significant migration was seen. There was no statistically significant difference between groups in the distribution of sockets showing migration above the clinically relevant threshold. Thus, our hypothesis could be confirmed: although additional screw fixation resulted in direct stability of the socket during the first 2 months, without additional screws the press-fit RM cup becomes a stable socket after the settling phase, with migrations remaining below the clinically relevant threshold (> 1 mm of translation, > 2° of rotation).
Radiostereometric analysis is a sensitive predictor of the long-term stability of arthroplasties (CitationRyd et al. 1995, Orstein et al. Citation2006, Rohrl et al. Citation2006, Derbyshire et al. Citation2009). In particular, it has demonstrated the stability of acetabular components in total hip arthroplasty (Nivbrant et al. Citation1996, Citation1997, Onsten et al. Citation1996, Thanner et al. Citation2000, Digas et al. Citation2004, Rohrl et al. Citation2004, Zhou et al. Citation2006). However, we have not found any articles reporting the effect on stability of additional screw fixation for the cementless, elastic press-fit socket. Our study supports the proposed potential advantage of the titanium particle-coated, cementless, elastic monoblock. This construction seems to promote osseointegration of the titanium-particle coating without affecting the elastic properties of the socket. Thus, it permits transmission of the physiological articular stresses, thereby reducing acetabular stress shielding and the development of acetabular osteolysis. In an unpublished, finite element study we have found high interfacial micromotions between the acetabular bone and the RM press-fit socket. This could be explained as being due to the elastic modulus of both the acetabular bone and the RM press-fit socket. Sufficient reduction of interfacial micromotions is necessary to produce adequate bone ingrowth and to achieve stability.
In vitro and computer analysis studies have reported contradicting views concerning the necessity of additional screw fixation (CitationWon et al.1995, Hsu et al. Citation2006, Hsu and Lin Citation2010). While in the present study we found an initial statistically significant proximal migration for sockets implanted without additional screw fixation, this effect remained well below the clinically relevant level. We attribute this minimal migration during the early postoperative period to the socket settling itself into the reamed acetabular bone. This has also been reported by Thanner et al. (Citation2000) who postulated that the placement of additional screws could compromise the required settling of the implant that is beneficial for the biological ingrowth when using a press-fit, metal-backed socket, as did Rohrl et al. (Citation2004). Schmalzried and co-workers had already noted the settling along the vector line of the hip joint reaction force in 1994 (Schmalzried et al. Citation1994). In addition, other authors have reported the advantages and disadvantages of additional screw fixation in cementless sockets (Perona et al. Citation1992, Huk et al. Citation1994, Barrack et al. Citation1997, Hsu et al. Citation2007). Recently, Zilkens et al. (Citation2011) used “ein bild” radiographic analysis (EBRA) to show that there was no effect when using additional screw fixation in rigid cementless press-fit sockets.
The values found in this study for the mean translations (< 0.3 mm) and the mean rotations (< 0.4°) in each directions for both groups are comparable to or below the migration values found in other RSA studies for sockets with or without additional fixation and with different surfaces (Onsten et al. Citation1996, Thanner et al. Citation2000, Rohrl et al. Citation2004, Zhou et al. Citation2006).
Multiplicity concerns could be raised when interpreting our results. Migration of a socket is a 3-dimensional process that—for explanatory purposes—has been determined in 2-dimensional planes between or around the x, y, and z-axes. When conducting statistical analyses on RSA data, one should keep in mind that by definition translation found within a plane defined by 2 axes defines the translation along the third axis. As a larger sample size was not possible for practical reasons, we used repeated-measures ANOVA to correct for multiplicity. Another limitation in interpreting the results of hip arthroplasty RSA studies is the clinical relevance of RSA migration values. In this study, the clinically relevant thresholds were based on the experience of orthopedic surgeons performing more than 100 total hip arthoplasties a year.
Based on the present data, this cementless press-fit elastic socket with a ceramic-on-PE articulation, without additional screw fixation, could have long-term survival and has the quality of reducing the potentially clinically relevant acetabular stress shielding as described in Wolff’s law. We are performing further clinical studies using quantative CT (computer tomography) bone mineral density measurements to evaluate the long-term effect of socket elasticity on acetabular bone quality.
In conclusion, we found a statistically significant proximal translation of the press-fit sockets without the additional screw fixation that was well below our clinically relevant threshold for migration. However, this migration appeared during the settling phase in the first 2 months postoperatively; after that period, the sockets became stable. We therefore see no benefit from additional screw fixation for this cementless, elastic press-fit socket.
The study protocol and further information concerning this study is available through the corresponding author, DP.
DP: primary investigator, study design, data analysis, and manuscript preparation. JL: RSA analysis, statistical analysis, and manuscript preparation. GvH and MS: senior surgeons, manuscript preparation.
We thank Dr Petra Heesterbeek of the Department of Research, Development and Education at the Sint Maartenskliniek for statistical advice and assistance in preparation of the the final manuscript. We also thank Patricia G. Anderson of the Department of Research, Development and Education at the Sint Maartenskliniek for English editing.
This study was funded by Mathys orthopaedics, Bettlach Ltd, Switzerland, and prior to this study there were no limitations described by either party, on publishing the data resulting from this scientific study.
- Barrack R, Folgueuras A, Munn B, Tvetden D, Sharkey P. Pelvic osteolysis and polyethylene wear at 5-8 years in an uncemented total hip. Clin Orthop 1997; (335): 211-7.
- Derbyshire B, Prescott R, Porter M. Notes on the use and interpretation of radiostereometric analysis. Acta Orthop 2009; 80: 124-30.
- Digas G, Thanner J, Anderberg C, Karrholm J. Bioactive cement or ceramic/porous coating vs conventional cement to obtain early stability of the acetabular cup. Randomised study of 96 hips followed with radiostereometry. J Orthop Res 2004; 22: 1035-43.
- Diks M, van den Broek CM, Anderson PG, van Limbeek J, Spruit M. The uncemented, titanium coated RM cup: Survival and analysis of failures. Hip Int 2005; 15: 71-7.
- Firestone D, Callaghan J, Liu S, Goetz D, Sullivan P, Vittetoe D, Johnston R. Total hip arthroplasty with a cemented, polished femoral stem, and a cementless acetabular component. A follow-up study at a minimum of ten years. J Bone Joint Surg (Am) 2007; 89: 126-32.
- Hadjari M, Hollis J, Hofmann O, Nelson C. Initial stability of porous coated acetabular implants. The effect of screw placement, screw tightness, defect type, and oversize implants. Clin Orthop 1994; (307): 117-23.
- Hsu J, Lin D. Effects of screw eccentricity on the initial stability of the acetabular cup in artificial foam bone of different quality. Artif Organs 2010; 34: E10-6.
- Hsu J, Lai K, Chen Q, Zobitz M, Huang H, An K, Chang C. The relation between micromotion and screw fixation in acetabular cup. Comput Methods Programs Biomed 2006; 84: 34-41.
- Hsu J, Chang C, Huang H, Zobitz M, Chen W, Lai K, An K. The number of screws, bone quality, and friction coefficient affect acetabular cup stability. Med Eng Phys 2007; 29: 1089-95.
- Huk O, Bansal M, Betts F, Rimnac C, Lieberman J, Huo M, Salvati E. Polyethylene and metal debris generated by non-articulating surfaces of modular acetabular components. J Bone Joint surg (Br) 1994; 76: 568-74.
- Huo MH, Osier CJ. Is cement still a fixation option for total hip arthroplasty? J Arthroplasty 2008; 23: 51-4.
- Ihle M, Mai S, Pfluger D, Siebert W. The results of the titanium-coated RM acetabular component at 20 years: a long-term follow-up of an uncemented primary total hip replacement. J Bone Joint Surg (Br) 2008; 90: 1284-90.
- Iorio R, Puskas B, Healy W, Tilzey J, Specht L, Thompson S. Cementless acetabular fixation with and without screws. J Arthroplasty 2010; 25: 309-13.
- Kim Y. Long-tern results of the cementless porous-coated anatomic total hip prosthesis. J Bone Joint Surg (Br) 2005; 87: 623-7.
- Kim YG, Kim SY, Kim SJ, Park BC, Kim PT, Ihn JC. The use of cementless expansion acetabular component and an alumina-polyethylene bearing in total hip arthroplasty for osteonecrosis. J Bone Joint Surg (Br) 2005; 87: 776-80.
- Nivbrant B, Karrholm J, Onsten I, Carlsson A, Snorrason F. Migration of porous press-fit cups in hip revision arthroplasty. J Arthroplasty 1996; 11: 390-6.
- Nivbrant B, Karrholm J. Migration and wear of hydroxyapatite-coated press-fit cups in revision hip arthroplasty. A radiostereometric study. J Arthroplasty 1997; 12: 904-12.
- Onsten I, Carlsson A, Sanzen L, Besjakov J. Migration and wear of a hydroxyapatite-coated hip prosthesis. J Bone Joint Surg (Br) 1996; 78: 85-91.
- Ornstein E, Franzen H, Johnsson R, Stefansdottir, Sundberg M, Tagil M. Five-year follow up of socket movements and loosening after revision with impacted morselized allograft bone and cement. J Arthroplasty 2006; 21: 975-84.
- Pakvis D, Biemond L, van Hellemondt G, Spruit M. A cementless elastic monoblock socket in young patients: a ten to 18-year clinical and radiological follow-up. Int Orthop 2011; 35: 1445-51.
- Perona P, Lawrence J, Paprosky W, Patwardhan A, Sartori M. Acetabular micromotion as a measure of initial implant stability in primary hip arthroplasty. An in vitro comparison of different methods of initial acetabular component fixation. J Arthroplasty 1992; 7: 537-47.
- Rohrl A, Nivbrant B, Strom H, Nilsson K. Effect of augmented cup fixation on stability, wear, and osteolysis. A 5-year follow up of total hip arthroplasty with RSA. J Arthroplasty 2004; 19: 962-71.
- Rohrl S, Nivbrant B, Snorrason F, Karrholm J, Nilsson K. Porous coated cups fixed with screws. A 12 year clinical and radiostereometric follow up of 50 hips. Acta Orthop 2006; 77: 393-401.
- Roth A, Winzer T, Sander K, Anders J, Venbrocks. Press fit fixation of cementless cups: how much stability do we need indeed? Arch Orthop Trauma Surg 2006; 126: 77-81.
- Ryd L, Albrektsson B, Carlsson L, Dansgard F, Herberts P, Lindstrand A, Regner L, Toksvig-Larsen S. J Bone Joint Surg (Br) 1995; 77: 377-83.
- Schmalzried T, Wessinger S, Hill G, Harris W. The Harris-Galante porous acetabular component press-fit without screw fixation. Five-year radiographic analysis of primary cases. J Arthroplasty 1994; 9: 235-42.
- Schmalzried T, Akizuki K, Fedenko A, Mirra J. The role of access of joint fluid to bone in periarticular osteolysis. A report of four cases. J Bone Joint Surg (Am) 1997; 79: 447-52.
- Selvik G. Roentgen stereophotogrammetric analysis. Acta Radiol 1990; 31: 113-26.
- Suckel A, Geiger F, Kinz L, Wulker N, Garbrecht M. Long term results for the uncemented Zweymuller/alloclassic hip endoprosthesis. A 15-year minimum follow-up of 320 hip operations. J Arthroplasty 2009; 24: 846-53.
- Thanner J, Karrholm J, Malchau H, Wallinder L, Herberts P. Migration of press-fit cups fixed with poly-l-lactic acid or titanium screws: A randomized study using radiostereometry. J Orthop Res 1996; 14: 895-900.
- Thanner J, Karrholm J, Herberts P, Malchau H. Hydroxyapatite and tricalcium phosphate-coated cups with and without screw fixation. A randomized study of 64 patients. J Arthroplasty 2000; 15: 405-12.
- Valstar ER, Gill R, Ryd L, Flivik G, Borlin N, Karrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005; 76: 563-72.
- Vrooman HA, Valstar ER, Brand GJ, Admiraal DR, Rozing PM, Reiber JH. Fast and accurate automated measurements in digitized stereophotogrammetric radiographs. J Biomech 1998; 31: 491-8.
- Won C, Hearn T, Tile M. Micromotion of cementless hemispherical acetabular components. Does press-fit need adjunctive screw fixation. J Bone Joint Surg (Br) 1995; 77: 484-9.
- Wright JM, Pellicci PM, Salvati EA, Ghelman B, Roberts MM, Koh JL. Bone density adjacent to press-fit acetabular components. A prospective analysis with quantitative computed tomography. J Bone Joint Surg (Am) 2001; 83: 529-36.
- Zhou Z, Li M, Borlin N, Wood D, Nivbrant B. No increased migration in cups with ceramic-on-ceramic bearing. An RSA study. Clin Orthop 2006; (448): 39-45.
- Zilkens C, Djalali S, Bittersohl B, . Migration pattern of cementless press fit cups in the presence of stabilizing screws in total hip arthroplasty. Eur J Med Res 2011; 28: 127-32.